GASTRO-JEJUNO-COLIC FISTULA
Transcript of GASTRO-JEJUNO-COLIC FISTULA

1348
Fig. 2-Blisters caused by bright skyshine. The large blister is of
thermal type. To the left of this blister is the hot dry anhidroticarea with rivulets of sweat from above. The smaller blisters are
sudamina.
SUNBURN BLISTERS
From the second day onwards after exposure to sun-light or u.v. lamp, provided erythema has been strongenough to cause desquamation, and environmentaltemperatures are high, successive crops of thin-walledvesicles containing sweat appear over the exposed areas.These vesicles are indistinguishable from the sudaminadescribed in standard textbooks of dermatology-e.g.,Sequeira (1919)-as occurring in acute fevers. Theyare caused by pressure of sweat which forces up the
injured surface layer of epidermis in which the mouthsof the sweat-gland ducts have been occluded. Severeexposure to u.v. radiation may in addition cause deeperblisters closely resembling thermal blister burns.A blond chief petty officer, aged 35, exposed himself in
swimming-trunks to bright skyshine (but not direct sunlight)for five hours on Changi beach, Singapore, on Feb. 21, 1949.Later on the same day severe erythema appeared. Thermal-
type blisters appeared next day, and sudamina on Feb. 24.By Feb. 29, 1949, the thermal-type blisters had healed withoutinfection or scarring.
Fig. 2 shows the right shoulder on Feb. 24, 1949. Rivuletsof sweat from the scalp may be seen traversing a zone whichwas free from blisters, and was hot and dry to the touch.This area had been exposed the most; and, in addition tosuperficial occlusion of sweat ducts, as in sudamina, thesecretion of sweat was probably reduced or absent. Theskin of sudaminous areas was moist and cool, showing thatsome sweat glands were functioning normally.The thermal-type blister lay between the dermis and the
epidermis ; its fluid contained chloride equivalent to 0’485%sodium chloride, protein (heavy coagulum), and white blood-cells (10 per high-power field). The sudaminous vesicles arosein the epidermis during sweating ; the contents resembledsweat (chloride equivalent to 0’210% sodium chloride, withoutprotein and white blood-cells).
DISCUSSION
It had previously been shown that u.v. radiation causeda reduction in sweating-rate, and the possibility was fore-seen that this might contribute to collapse in the heat incertain circumstances (Thomson 1951a).
It may be shown that under arid conditions a sweatdeficit of 100 ml. would allow a rise of 1°C (1-8°F) inbody-temperature; hence a sweat deficit of 230 ml.
might have caused the observed harmful rise in rectaltemperature (2°F) in Ha. The possibility that reducedsweating was also responsible for collapse in Al. cannotbe excluded, because O’Brien (1947) has shown thatwhen a proportion of sweat glands are out of action theremainder hypersecrete.The doses of u.v. light received from sun or lamp were
not measured quantitatively ; but, since they did notcause thermal blistering, which may result from
injudicious exposure to the sun even in England, it is
clear that greater injury may result from tropical sun-light. Heatstroke can obviously occur in the absenceof sunlight where environmental temperatures are
intolerably high. The findings reported here suggestthat sunburn may lower tolerance to heat, that exposureto the tropical sun should be carefully graduated, andthat initial exposure is best avoided during very hotweather.
SUMMARY
Two men collapsed in a heated room a day afterreceiving ultraviolet burns, one from the sun, and theother from an ultraviolet lamp. They had withstood theenvironmental conditions (effective temperature 91’Pon control days without undue hardship.Two kinds of blisters may develop after ultraviolet
burn. The more important type arises between thedermis and the epidermis within forty-eight hours ofinjury, contains a plasma-like exudate, and should betreated like thermal second-degree burns. The secondtype (sudamina) arises superficially in the corneum fromthe second day onwards after injury, contains sweat,and requires no treatment.
I am grateful to the Medical Director-General of the Navyfor permission to publish this article ; to Dr. J. S. Weiner,of the department of human anatomy in the University ofOxford, for permission to cite his data for Ha. on May 10and to use the climatic chamber and the men ; to theobservers, Mr. J. W. Jack and Mr. W. S. Cague ; and to Ha.and Al.
REFERENCES
Aron, H. (1911) Philipp. J. Sci. B. 6, 101.Blum, H. F. (1945) Physiol. Rev. 25, 483.O’Brien, J. P. (1947) Brit. J. Derm. 59, 125.Sequeira, J. H. (1919) Diseases of the Skin. 3rd ed., London;
p. 582.Thomson, M. L. (1951a) J. Physiol. 112, 22.
— (1951b) Ibid, p. 31.
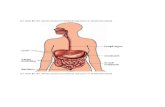
GASTRO-JEJUNO-COLIC FISTULA
C. C. HOLMANM.B. Camb., F.R.C.S.
CONSULTANT SURGEON, NORTHAMPTON GENERAL HOSPITAL
As gastro-enterostomy is superseded by subtotal
gastrectomy, so will gastro-jejuno-colic fistula recedeinto the background. Meanwhile, though such a fistulais relatively uncommon it presents the surgeon witha formidable problem. -
To reduce the risk of the operation various two-stageprocedures have been advised. Surgeons have donepreliminary colostomy, ileocolostomy, or even ileostomy.The fortitude of the average patient is such that a two-stage operation is accepted with good grace. I hope,however, that the technique described here will allow aone-stage operation to be done without undue risk.I have not been able to find any published description ofa similar method.
CASE-RECORD
Case l.-A man, aged 41, was admitted to hospital in 194?with a perforated duodenal ulcer. The perforation was
closed and a posterior gastro-enterostomy done. The patientremained well for three years and then began to have abdominaldiscomfort and diarrhoea. The diarrhoea became worse, andradiography in July, 1947, showed that a barium enemaflowed into the stomach. The patient’s condition was

1349
reasonably good. After a preliminary course of succinylsulphathiazole an operation was done on Aug. 22, 1947.Operation.-After the abdomen had been opened the
jejunum was divided on either side of the stoma, and themiddle part was left attached to the stomach after the endshad been closed. The proximal and distal parts were joinedend to end. Next the duodenum was divided and closed andthe stomach freed as far as the stoma, where the portionattached to the fragment of jejunum was divided betweenclamps, close to the anastomosis. The small detached
fragment of stomach was closed after the mucosa had beenremoved. Finally subtotal gastrectomy was done (fig. 1).Progress.-The pqtient made a good recovery. A barium
enema in October, 1948, showed nothing abnormal. In
November, 1950, the patient reported that he was carryingon reasonably well in a sedentary occupation and had notconsulted his doctor in the past two years.Case 2.-A man, aged 63, had undergone posterior gastro-
enterostomy some years previously, and was emaciated andhad intractable diarrhoea.
Operation revealed so much induration and fixation in theregion of the stoma that I thought the condition was malignantand inoperable. In the hope of giving relief I divided thecolon on either side of the fistula, united the two ends, andclosed the ends of the excluded segment (fig. 2). The mucosaof the bowel appeared spotless, as if scoured by the gastriccontents.
Progress.-To my surprise the patient made a rapid recovery.Two years later he is in reasonably good health. Radiographyshows the stoma to be functioning. The attached segmentof colon was not seen.
COMMENTS
When I performed this operation I was unaware thatit had already been described by Moroney (1948).In case 1 the detached fragment of stomach, bereft
of mucosa, should cause no trouble. One assumes
that any secretion from the excluded segment of jejunumwill continue to drain into the colon. Similarly, in case 2the excluded colon should drain into the stomach. Ifvisions of subsequent distension and rupture of theexcluded bowel disturb the surgeon’s peace of mind,removal at a later date should present no great difficulty.
REFERENCE
Moroney, J. (1948) Brit. J. Surg. 35, 374.
BULLET WOUND THROUGH BOTH
FRONTAL LOBES WITH RECOVERY
JOHN SLORACHM.B., B.Sc. Aberd., D.P.M.
DEPUTY PHYSICIAN-SUPERINTENDENT, PARK PREWETT HOSPITAL,BASINGSTOKE
THE following case-record may be of interest in viewof the circumstances of the incident and the subsequentrecovery of the patient with minimal personality changes.A man, aged 55, was discovered by his wife, fully dressed
and partaking of his breakfast, with blood trickling downboth sides of his face from a wound on either side of his scalp.At 11 P.M. the night before, when in bed, he had shot himselfthrough the head with a 0.38 revolver ; but in the morning hehad got up, dressed himself (even brushing his hair) and hadcooked his own breakfast.He was one of twelve children, all of whom were well, and
there was no psychopathy in the family history. His four
grown-up children were doing well. A regular officer, hislife had been spent in the Army, and he had attained fieldrank. He had always been of a melancholy disposition,selfish, independent, and inconsiderate, though a hard worker.Since retirement in 1942 he had been unsettled, becomingparanoid, solitary, moody, bad-tempered, and depressed,and had threatened to shoot himself. He had no hobbies,drank to excess, and had incurred considerable debts justbefore his suicidal attempt.When admitted to a general hospital, he was fully conscious
and replied to questions, but was uncooperative and deluded.lie had a circular wound 1/2 inch in diameter with blackenededges on the right temple, a star-shaped lacerated wound inthe left upper temple also 1/2 inch in diameter, and a swelling
of his right lower jaw. He had no neurological signs apartfrom absence of both upper abdominal reflexes. Toilet of thewounds was carried out and loose bone was removed. The
patient was transferred to his present hospital 6 days aftershooting himself.On admission he was r0Ristive, restless, aggressive, and
impulsive, and resented examination, but was accessible,though retarded in thought. He was disoriented in time andplace, and said he was living on the roof of his house. He hadno memory of the shooting and a patchy memory of his stayin the general hospital. He also showed falsification of memory,and had great difficulty in finding nouns. He described, forexample, the white-coated nurses as
"
sugar-iced people," anddescribed one as a " toy manufacturer." He was aurallyhallucinated, and expressed delusions of persecution. Heshowed no neurological signs on physical examination. The
radiologist’s report on the X-ray examinations of the skullwas : " I am quite satisfied that the bullet traversed thebrain and so produced a leucotomy. The bullet entered theskull on the right side just above the zygoma, passed obliquelyupwards, forwards, and inwards, and made its exit at a higherlevel through the upper part of the frontal bone 2-3 in. abovethe left eye. The entry wound is quite small (1/2 inch indiameter) and sharp. The exit wound is much larger, and thevault is fractured over a wide area. The track of the bulletwould pass through both frontal lobes."Progress.-The patient quickly settled down. He became
rather apathetic and uninterested in his surroundings, butmade steady progress. After 3 months he was mentally alert,rational, more interested in his surroundings, cooperative, andread the daily papers. He denied ever having been depressedand was unwilling to accept the idea that he had inflictedthe wound on himself. His wife said that he was just asintolerant, selfish, inconsiderate, stubborn, and awkward aspreviously, though not tense or depressed. He expressed nosorrow for the trouble he had caused his family. He showed aretrograde amnesia of 6 hours and had little memory of theevents of the first 7 days after the incident. Psychometrictests showed a deterioration of 32%. An electro-encephalo.gram, taken 3 months after the suicidal attempt, was normal,and the patient was discharged from hospital 2 months later.Follow-up.-Nine months after his discharge he was found
to have made an uneventful recovery, with no recurrence ofhis depression, but was just as bad tempered, unreasonable,and difficult to live with as before.
DISCUSSION
Freeman and Watts (1942) in their review of injuriesof the frontal lobes, cited several cases of through-and-through wounds which produced remarkably littlediscomfort to the patient immediately afterwards.A child, whose case was reported in the 19th century,
sustained a through-and-through wound of the temples andsat up happily in its crib playing with its toys, with no dis-comfort. In the " American crowbar case " reported first byHarlow in 1848, a man of 25 was wounded by a tamping iron3 ft. 7 in. long and P/4 in. in diameter and weighing 131/4 lb.,which passed through his face and brain. Though thrownbackwards, he talked to his mates and later, with little assis-tance, walked up a flight of stairs in his hotel to receive medicalattention.Swanson (1931) reported the case of a youth of 19 who was
brought to hospital sitting in a wheel-chair with an air-pumpplunger rod 18 in. long and 5/16 in. in diameter through hishead. He was conscious and replied to questions.Foxton (1947) reported the case of a man found walking on
to a hospital ship during the first world war with a through-and-through bullet wound of his temporal lobes, little the worsefor his experience.As in the cases reported by Guttmann (1943) and
Rogers (1948), the suicidal attempt cleared up the
depression from which the patient was suffering. Recov-
ery in these cases is due to a combination of psychologicaland physical factors, and it is difficult to assess the relativeimportance of each. Apart from the shock in this case,the act accomplished a purpose by the completion of asuicidal attempt long contemplated, as well as removingthe patient from an environment to which he wasmaladjusted.One would presume that the right frontal lobe was
seriously damaged, but the left not a great deal, since