Van Dijk.2750-Proefschrift 10 - COnnecting REpositories · 2018-07-07 · 507383-L-bw-van Dijk ª...
Transcript of Van Dijk.2750-Proefschrift 10 - COnnecting REpositories · 2018-07-07 · 507383-L-bw-van Dijk ª...

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Fiona van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
ISBN
978-94-6284-086-7
Cover illustration
Alexander Hertog
Design/lay-out
Promotie In Zicht, Arnhem
Ipskamp Printing, Enschede
© Fiona van Dijk, 2017
All rights reserved. No part of this thesis may be reproduced or printed in any form or by any means,
electronically, mechanically, including photocopy, recording or any information storage and retrieval
system without written permission of the author.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Proefschrift
ter verkrijging van de graad van doctor
aan de Radboud Universiteit Nijmegen
op gezag van de rector magnificus prof. dr. J.H.J.M. van Krieken,
volgens besluit van het college van decanen
in het openbaar te verdedigen op vrijdag 3 maart 2017
om 16.30 uur precies
door
Fiona Eva van Dijk
Geboren op 2 december 1973
te Hardenberg

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Promotoren
Prof. dr. J.K. Buitelaar
Prof. dr. R.J. Verkes
Copromotoren
Dr. J.C. Glennon
Dr. C.C. Kan
Manuscriptcommissie
Prof. dr. J.B. Prins
Prof. dr. P.P.G. Hodiamont
Dr. J.J.S. Kooij (PsyQ, Den Haag)

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Contents
Chapter 1 General introduction 7
Chapter 2 ADHD, personality and its disorders 19
Chapter 3 Lifespan attention deficit/hyperactivity disorder and
borderline personality disorder symptoms in female patients:
a latent class approach
49
Chapter 4 Symptomatic overlap between attention-deficit/hyperactivity
disorder and borderline personality disorder in women:
the role of temperament and character traits
71
Chapter 5 Do cognitive measures of response inhibition differentiate
between attention deficit/hyperactivity disorder and
borderline personality disorder?
89
Chapter 6 Five Factor Model personality traits relate to adult attention-
deficit/hyperactivity disorder but not to their distinct
neurocognitive profiles
109
Chapter 7 Summary and General Discussion 131
Nederlandse samenvatting
List of publications
Dankwoord
Curriculum Vitae
Donders Graduate School for Cognitive Neuroscience
155
159
161
165
167

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
General introduction
1

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
9
GENERAL INTRODUCTION
1
General introduction
This thesis originates from clinically driven questions about the relationship
between adult attention-deficit/hyperactivity disorder (ADHD) and borderline
personality disorder (BPD) symptoms. It intends to contribute to the understanding
of the origin of the overlap and differences in both disorders on the level of
classification, personality traits, and neurocognition. The general introduction is
a synopsis of what is currently known about adult ADHD and BPD in general and
more specifically about their clinical overlap, temperament traits, and neuro-
cognitive features. After that, I will describe the overall aim and outline of this
thesis.
Adult attention-deficit hyperactivity disorder ADHD is defined as a childhood-onset neurodevelopmental disorder in the American
Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders
(5th edition; DSM-5) and is characterized by the presence of developmentally
inappropriate and impairing levels of inattention, hyperactivity, and impulsivity
(APA 2013). ADHD was perceived as a childhood-onset disorder with limited effect
on adult psychopathology. However the symptoms and impairments that define
ADHD often affect the adult population, for an overview of key conceptual issues
in adult ADHD see (Asherson, Buitelaar et al. 2016). The estimated prevalence of
ADHD in adults ranges from 2-5% to 3-4% (Fayyad, De Graaf et al. 2007; Simon,
Czobor et al. 2009). Worldwide, up to 50% of children with ADHD continue to meet
diagnostic criteria for ADHD as adults (Lara, Fayyad et al. 2009) with some
European studies suggesting persistence rates of ADHD even up to 80% (van
Lieshout, Luman et al. 2016). Although there is the possibility that ADHD might
emerge after childhood (Moffitt, Houts et al. 2015), for most adult patients with
ADHD there is a clear history of ADHD from childhood. A male: female adult ratio
of 3-4:1 is recorded in epidemiological samples (Biederman, Kwon et al. 2005) but
in clinical practice the rate of persistent ADHD does not significantly differ across
genders (Cortese, Faraone et al. 2016). Factors influencing course and outcome of
ADHD include general cognitive ability, severity of ADHD, causal factors (genes
and environment), brain maturation and development, and the presence of
co-occurring mental health and neurodevelopmental disorders (Faraone, Asherson
et al. 2015).
Despite the high prevalence of adult ADHD and known links to psychosocial,
functional, and mental health problems, high rates of undiagnosed or untreated
ADHD have been found (Huntley, Maltezos et al. 2012; Young, Moss et al. 2015).
Therefore, improving understanding of the clinical presentation of ADHD in
adulthood is of great importance.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
10
CHAPTER 1
Symptoms of ADHD cluster together in two major dimensions: inattention
and hyperactivity-impulsivity. They reflect continuous traits rather than a categorical
disorder which also means that the symptoms do not reflect a change from the
premorbid state (as is also the case in personality disorders). The definition of a
clinically significant disorder is therefore based on the presence of clinically
significant impairment of functioning (APA 2013). The core symptoms of ADHD
tend to decline with age, although inattentive features persist over the longer
term across the lifespan (Faraone, Biederman et al. 2006). In clinical practice a full
understanding of the broader issues in ADHD is needed to improve diagnostic
outcome. ADHD is also linked to executive function impairments, sleep problems,
emotional dysregulation, mental restlessness, in addition to functional impairments
such as traffic accidents and occupational underachievement (Van Veen, Kooij et al.
2010; Adler, Dirks et al. 2013; Skirrow and Asherson 2013; Surman, Biederman
et al. 2013; Mowlem, Skirrow et al. 2016). High levels of concurrent comorbidity
with other neurodevelopmental disorders such as autism spectrum disorder,
learning and motor disorders, intellectual disability, and tic disorders exist in
those with ADHD (Jensen and Steinhausen 2015). In addition ADHD also co-occurs
with substance use disorders, anxiety, depression, personality disorders, and conduct
problems (Jensen and Steinhausen 2015; Matthies and Philipsen, 2016; Smith and
Samuel, 2016). Understanding the similarities and differences between adult
ADHD and common co-occurring mental disorders is important in order to
prevent under-diagnosis of ADHD. The pervasive nature of emotional instability
in adult mental health means that all individuals with a non-episodic form
of emotional instability should be screened for ADHD, including those with
personality disorders (Asherson, Buitelaar et al. 2016).
Borderline personality disorder Borderline personality disorder is characterized by a pervasive pattern of instability
in emotional regulation, interpersonal relationships and self-image, along with
marked impulsivity. It is associated with suicide, high rates of comorbid mental
disorders, and substantial costs to society (Leichsenring, Leibing et al. 2011).
Despite continued controversy regarding the diagnosis of BPD prior to adulthood
there is a growing body of research showing that youth BPD is a valid construct,
supporting the clinical recognition of the disorder in youth (Winsper, Lereya et al.
2016). Etiological factors leading to BPD remain only partially elucidated, though
it is recognized that genetic, neurobiological and psychosocial factors all contribute
to the development of the disorder (Crowell, Beauchaine et al. 2009). BPD affects up
to 3% of the general population (Lenzenweger 2008). In primary care, the prevalence
of BPD ranges from 4 to 6% (Moran, Jenkins et al. 2000; Gross, Olfson et al. 2002).
In epidemiological samples the prevalence is roughly equal male to female, whereas

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
11
GENERAL INTRODUCTION
1
in clinical services there is a clear preponderance of women, who are more likely
to seek treatment (Torgersen, Kringlen et al. 2001; Zimmerman, Chelminski et al.
2008).
Despite evidence of the reliability and validity of the diagnosis and the
treatability of the condition, many people with BPD remain undiagnosed in
clinical practice, placing them at risk for ineffective or possibly harmful treatment
(Chanen 2015; Tyrer, Reed et al. 2015). One cause of diagnostic confusion is the
high rate of comorbid disorders. BPD is a heterogeneous condition and its symptoms
overlap considerably with depressive, schizophrenic, impulsive, dissociative and
identity disorders. This overlap is also linked to comorbidity and in clinical
practice it may therefore be difficult to determine if the presenting symptoms are
those of borderline personality disorder or a related comorbid condition.
Adult ADHD and BPD: Clinical overlap In clinical practice, ADHD and BPD can sometimes be difficult to distinguish.
Several symptoms such as impulsivity, emotional/affective instability, risk taking
behavior, difficulty in controlling anger and impaired stress tolerance are found
in ADHD as well as in BPD patients. Among these features, impulsivity has been
identified as one of the most common traits occurring within this overlap (Dowson,
Bazanis et al. 2004; Davids and Gastpar 2005). Deficits in affect regulation are a
key feature of BPD but are also recognized as an associated feature of ADHD
(Skirrow and Asherson 2013). The same applies to disturbed interpersonal
relationships; a symptom often experienced by BPD patients, but adults with
ADHD may also show interpersonal problems as a consequence of their ADHD
symptoms (Philipsen 2006). Indistinguishable comorbidity rates have been found
for substance abuse, anxiety and eating disorders and high levels of cyclothymia
(Eich, Gamma et al. 2014). Additionally, both disorders show a chronic trait like
course, and although historically BPD was seen as a disorder presenting mostly in
late adolescence and early adulthood, we now know that symptoms can already
present in childhood (Winsper, Lereya et al. 2016). Moreover, ADHD and BPD often
co-occur (Biederman 2004), with rates of BPD among adult ADHD ranging from
19% to 37% (Miller, Flory et al. 2008). Despite the evidence of overlap and
co-occurrence, the nature of the relation between both disorders remains not
fully understood. A further challenge in this field of research are the gender
differences in the prevalence of these disorders; equivalent prevalence of adult
ADHD in males and females and a higher prevalence of BPD among female versus
male patients in clinical settings (Skodol and Bender 2003). Gender may therefore
be an important factor to consider in understanding the relationship between
ADHD and BPD.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
12
CHAPTER 1
Adult ADHD and BPD: temperament and personality traits Dimensional models of personality may be helpful in addressing problems of
excessive co-occurrence, heterogeneity among persons with the same diagnosis,
and artefactual or epiphenomenal diagnostic distinctions (Widiger and Simonsen
2005). While ADHD is viewed in categorical terms in the DSM-IV and DSM-5, there
is support for a dimensional view of it (Marcus and Barry 2011; Coghill and
Sonuga-Barke 2012). Similar to personality dimensions, ADHD is stable across time
and highly heritable (Biederman 2005). Indeed, ADHD and BPD share a number of
temperament/personality traits and a “typical ADHD temperament” seem to
correspond to an explosive/borderline type of personality (Anckarsater, Stahlberg
et al. 2006). Insight into the associations between temperament/personality traits
and ADHD and co-occurring BPD may help delineate possible developmental
pathways and explain comorbid disorder development. Predictive data concerning
the development of BPD comes from prospective studies and showed that a
diagnosis of ADHD in childhood was predictive of later BPD symptoms (Burke and
Stepp 2012; Stepp, Burke et al. 2012), but little is known about the process(es)
underlying this path (Storebø and Simonsen 2013). Action-oriented temperament/
personality traits like impulsivity, novelty seeking and conduct problem could
mediate the relation between childhood ADHD symptoms and adult BPD features
(Carlotta, Borroni et al. 2013).
Adult ADHD and BPD: Cognitive functioning ADHD has been associated with neurocognitive deficits in multiple cognitive
domains. The main domains of neuropsychological dysfunction in ADHD are:
memory, inhibitory control, delay aversion, decision making, timing, and response
variability. The levels of deficiency in each of these domains differ more or less
independently within patients with ADHD, and there is considerable overlap
between neuropsychological performance in patients with ADHD and normal
controls (Coghill, Seth et al. 2014). Although at a behavioral level executive
dysfunctions are strongly related to ADHD, it is much debated whether it reflects
primary causal processes in ADHD. There is substantial heterogeneity in cognitive
functioning, and there is no straightforward association between cognitive
performance and the trajectory of clinical symptoms (van Lieshout, Luman et al.
2013; Coghill, Hayward et al. 2014; Coghill, Seth et al. 2014; Mostert, Hoogman
et al. 2015; Mostert, Onnink et al. 2015).
Neuropsychological deficits have also been identified as a robust feature of
BPD. Since impulsivity is a core feature in PD, it is not surprising that poor
inhibitory functioning has been a consistent finding in BPD (Nigg, Silk et al. 2005).
However, compared to healthy controls significant impairment was found across
the full range of traditional neuropsychological tests. The most consistent deficits

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
13
GENERAL INTRODUCTION
1
were found in the domains of attention, cognitive flexibility, learning and memory,
planning, processing speed, and visuospatial abilities (Ruocco 2005). Meta analyses
of BPD samples with higher percentage of comorbidity (i.e. personality disorder,
major depression, eating disorders and substance abuse disorders) showed worse
neuropsychological functioning than patients with less percentage of such
comorbid disorders (Unoka and Richman 2016). A recent study examined the
comorbid presentation of ADHD and BPD and suggested more informant, but not
self-reported, symptoms of impulsivity and lower intellectual and attentional
functioning compared to a group with only ADHD (O’Malley, McHugh et al. 2016).
Co-occurring disorders thus seem to affect the cognitive performance of BPD
patients. To clarify the influence of ADHD and BPD on each other and improve
their phenotypic characterization, it is important to establish whether and how
ADHD and BPD are related on a neurocognitive level.
Aims and outline of the thesis The aim of the current thesis was to critically appraise the association between
Adult ADHD and BPD. This was assessed by investigating the overlap and differences
between adult ADHD and BPD on the level of symptoms, temperament (and
character) traits, and neurocognitive performance. In chapter 2 we presented a
literature review on ADHD, personality disorders, and personality traits. This
work resulted in a book chapter for ADHD in Adults: Characterization, Diagnosis
and Treatment (van Dijk and Anckarsater 2011). In chapter 3, Latent Class Analyses
were undertaken to identify mutually exclusive classes of female ADHD and BPD
subjects with homogeneous symptom profiles (van Dijk, Lappenschaar et al. 2011).
This first study provided a basis for its sequel (chapter 4). In chapter 4, we build on
the knowledge that ADHD and BPD seem to share a number of temperament and
character traits. In this study we account for the comorbid presence of BPD in
ADHD and vice versa. We examined the role of temperament and character traits
in the differentiation of classes of patients with similar ADHD and BPD symptom
profiles and possible pathways between early temperament and future ADHD and/
or BPD were evaluated in a female population (van Dijk, Lappenschaar et al. 2012).
In chapter 5 we studied whether cognitive measures of response inhibition derived
from a Continuous Performance Task are able to differentiate between adult
ADHD, BPD and healthy controls (van Dijk, Schellekens et al. 2014). Response
inhibition was chosen as a cognitive construct to study given the significant
impairment in this domain reported in ADHD and BPD. Finally, in chapter 6 we
investigated interactions between adult ADHD, cognitive profiles, and personality
traits in comparison to healthy controls. (Van Dijk, Mostert et al. 2016). In chapter 7
all studies presented in this thesis are integrated and a critical discussion along
with suggestions for future directions presented.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
14
CHAPTER 1
References
Adler, L. A., B. Dirks, et al. (2013). “Self-Reported quality of life in adults with attention-deficit/hyperactivity
disorder and executive function impairment treated with lisdexamfetamine dimesylate: a randomized,
double-blind, multicenter, placebo-controlled, parallel-group study.” BMC Psychiatry 13: 253.
Anckarsater, H., O. Stahlberg, et al. (2006). “The impact of ADHD and autism spectrum disorders on
temperament, character, and personality development.” Am J Psychiatry 163(7): 1239-1244.
APA (2013). Diagnostic and Statistical Manualof Mental Disorders - DSM 5. Washington, DC, American
Psychiatric Publishing.
Asherson, P., J. Buitelaar, et al. (2016). “Adult attention-deficit hyperactivity disorder: key conceptual issues.”
The Lancet.
Biederman, J. (2004). “Impact of comorbidity in adults with attention-deficit/hyperactivity disorder.” J Clin
Psychiatry 65 Suppl 3: 3-7.
Biederman, J. (2005). “Attention-deficit/hyperactivity disorder: a selective overview.” Biol Psychiatry 57(11):
1215-1220.
Biederman, J., A. Kwon, et al. (2005). “Absence of gender effects on attention deficit hyperactivity disorder:
findings in nonreferred subjects.” Am J Psychiatry 162(6): 1083-1089.
Burke, J. D. and S. D. Stepp (2012). “Adolescent disruptive behavior and borderline personality disorder
symptoms in young adult men.” J Abnorm Child Psychol 40(1): 35-44.
Carlotta, D., S. Borroni, et al. (2013). “On the relationship between retrospective childhood ADHD symptoms
and adult BPD features: the mediating role of action-oriented personality traits.” Compr Psychiatry
54(7): 943-952.
Chanen, A. M. (2015). “Borderline Personality Disorder in Young People: Are We There Yet?” J Clin Psychol
71(8): 778-791.
Coghill, D. and E. J. Sonuga-Barke (2012). “Annual research review: categories versus dimensions in the
classification and conceptualisation of child and adolescent mental disorders--implications of recent
empirical study.” J Child Psychol Psychiatry 53(5): 469-489.
Coghill, D. R., D. Hayward, et al. (2014). “A longitudinal examination of neuropsychological and clinical
functioning in boys with attention deficit hyperactivity disorder (ADHD): improvements in executive
functioning do not explain clinical improvement.” Psychol Med 44(5): 1087-1099.
Coghill, D. R., S. Seth, et al. (2014). “A comprehensive assessment of memory, delay aversion, timing,
inhibition, decision making and variability in attention deficit hyperactivity disorder: advancing
beyond the three-pathway models.” Psychol Med 44(9): 1989-2001.
Cortese, S., S. V. Faraone, et al. (2016). “Gender differences in adult attention-deficit/hyperactivity disorder:
results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC).” J Clin
Psychiatry 77(4): e421-428.
Crowell, S. E., T. P. Beauchaine, et al. (2009). “A biosocial developmental model of borderline personality:
Elaborating and extending Linehan’s theory.” Psychol Bull 135(3): 495-510.
Davids, E. and M. Gastpar (2005). “Attention deficit hyperactivity disorder and borderline personality
disorder.” Prog Neuropsychopharmacol Biol Psychiatry 29(6): 865-877.
Dowson, J., E. Bazanis, et al. (2004). “Impulsivity in patients with borderline personality disorder.” Compr
Psychiatry 45(1): 29-36.
Eich D., Gamma A. et al. (2014). Temperamental differences between bipolar disorder, borderline personality
disorder, and attention deficit/hyperactivity disorder: some implications for their diagnostic validity.
J Affect Disord. 169:101-104.
Faraone, S. V., P. Asherson, et al. (2015). “Attention-deficit/hyperactivity disorder.” Nat Rev Dis Primers 1: 15020.
Faraone, S. V., J. Biederman, et al. (2006). “The age-dependent decline of attention deficit hyperactivity
disorder: a meta-analysis of follow-up studies.” Psychol Med 36(2): 159-165.
Fayyad, J., R. De Graaf, et al. (2007). “Cross-national prevalence and correlates of adult attention-deficit
hyperactivity disorder.” Br J Psychiatry 190: 402-409.
Gross, R., M. Olfson, et al. (2002). “Borderline personality disorder in primary care.” Arch Intern Med 162(1):
53-60.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
15
GENERAL INTRODUCTION
1
Huntley, Z., S. Maltezos, et al. (2012). “Rates of undiagnosed attention deficit hyperactivity disorder in
London drug and alcohol detoxification units.” BMC Psychiatry 12: 223.
Jensen, C. M. and H. C. Steinhausen (2015). “Comorbid mental disorders in children and adolescents with
attention-deficit/hyperactivity disorder in a large nationwide study.” Atten Defic Hyperact Disord 7(1):
27-38.
Lara, C., J. Fayyad, et al. (2009). “Childhood predictors of adult attention-deficit/hyperactivity disorder:
results from the World Health Organization World Mental Health Survey Initiative.” Biol Psychiatry
65(1): 46-54.
Leichsenring, F., E. Leibing, et al. (2011). “Borderline personality disorder.” Lancet 377(9759): 74-84.
Lenzenweger, M. F. (2008). “Epidemiology of personality disorders.” Psychiatr Clin North Am 31(3): 395-403, vi.
Marcus, D. K. and T. D. Barry (2011). “Does attention-deficit/hyperactivity disorder have a dimensional
latent structure? A taxometric analysis.” J Abnorm Psychol 120(2): 427-442.
Matthies S. and Philipsen A. (2016). Comorbidity of Personality Disorders and Adult Attention Deficit
Hyperactivity Disorder (ADHD)--Review of Recent Findings. Curr Psychiatry Rep. 18(4):33.
Miller, C. J., J. D. Flory, et al. (2008). “Childhood attention-deficit/hyperactivity disorder and the emergence
of personality disorders in adolescence: a prospective follow-up study.” J Clin Psychiatry 69(9):
1477-1484.
Moffitt, T. E., R. Houts, et al. (2015). “Is Adult ADHD a Childhood-Onset Neurodevelopmental Disorder?
Evidence From a Four-Decade Longitudinal Cohort Study.” Am J Psychiatry 172(10): 967-977.
Moran, P., R. Jenkins, et al. (2000). “The prevalence of personality disorder among UK primary care
attenders.” Acta Psychiatr Scand 102(1): 52-57.
Mostert, J. C., M. Hoogman, et al. (2015). “Similar Subgroups Based on Cognitive Performance Parse
Heterogeneity in Adults With ADHD and Healthy Controls.” J Atten Disord.
Mostert, J. C., A. M. Onnink, et al. (2015). “Cognitive heterogeneity in adult attention deficit/hyperactivity
disorder: A systematic analysis of neuropsychological measurements.” Eur Neuropsychopharmacol.
Mowlem, F. D., C. Skirrow, et al. (2016). “Validation of the Mind Excessively Wandering Scale and the
Relationship of Mind Wandering to Impairment in Adult ADHD.” J Atten Disord.
Nigg, J. T., K. R. Silk, et al. (2005). “Disinhibition and borderline personality disorder.” Dev Psychopathol
17(4): 1129-1149.
O’Malley G.K., McHugh L. et al. (2016). Characterizing adult attention-deficit/hyperactivity-disorder and
comorbid borderline personality disorder: ADHD symptoms, psychopathology, cognitive functioning
and psychosocial factors. Eur Psychiatry. 31:29-36.
Philipsen, A. (2006). “Differential diagnosis and comorbidity of attention-deficit/hyperactivity disorder
(ADHD) and borderline personality disorder (BPD) in adults.” Eur Arch Psychiatry Clin Neurosci 256
Suppl 1: i42-46.
Ruocco, A. C. (2005). “The neuropsychology of borderline personality disorder: a meta-analysis and review.”
Psychiatry Res 137(3): 191-202.
Simon, V., P. Czobor, et al. (2009). “Prevalence and correlates of adult attention-deficit hyperactivity
disorder: meta-analysis.” Br J Psychiatry 194(3): 204-211.
Smith T.E. and Samuel D.B.(2016). A Multi-Method Examination of the Links Between ADHD and Personality
Disorder. J Pers Disord. 4:1-23.
Skirrow, C. and P. Asherson (2013). “Emotional lability, comorbidity and impairment in adults with attention-
deficit hyperactivity disorder.” J Affect Disord 147(1-3): 80-86.
Skodol, A. E. and D. S. Bender (2003). “Why are women diagnosed borderline more than men?” Psychiatr Q
74(4): 349-360.
Stepp, S. D., J. D. Burke, et al. (2012). “Trajectories of attention deficit hyperactivity disorder and oppositional
defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent
girls.” J Abnorm Child Psychol 40(1): 7-20.
Storebø O.J. and Simonsen E. (2013). Is ADHD an early stage in the development of borderline personality
disorder? Nord J Psychiatry. 64:1-7.
Surman, C. B., J. Biederman, et al. (2013). “Understanding deficient emotional self-regulation in adults with
attention deficit hyperactivity disorder: a controlled study.” Atten Defic Hyperact Disord 5(3): 273-281.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
16
CHAPTER 1
Torgersen, S., E. Kringlen, et al. (2001). “The prevalence of personality disorders in a community sample.”
Arch Gen Psychiatry 58(6): 590-596.
Tyrer, P., G. M. Reed, et al. (2015). “Classification, assessment, prevalence, and effect of personality disorder.”
Lancet 385(9969): 717-726.
Unoka, Z. and M. J. Richman (2016). “Neuropsychological deficits in BPD patients and the moderator effects
of co-occurring mental disorders: A meta-analysis.” Clin Psychol Rev 44: 1-12.
van Dijk, F., M. Lappenschaar, et al. (2011). “Lifespan attention deficit/hyperactivity disorder and borderline
personality disorder symptoms in female patients: a latent class approach.” Psychiatry Res 190(2-3):
327-334.
Van Dijk, F., J. Mostert, et al. (2016). “Five Factor Model personality traits relate to Adult Attention-Deficit/
Hyperactivity Disorder but not to their distinct neurocognitive profiles.” Under review..
van Dijk, F., A. Schellekens, et al. (2014). “Do cognitive measures of response inhibition differentiate
between attention deficit/hyperactivity disorder and borderline personality disorder?” Psychiatry
Res 215(3): 733-739.
van Dijk, F. E. and H. Anckarsater (2011). ADHD, personality, and its disorders. ADHD in Adults: Character-
ization, Diagnosis and Treatment. J. Buitelaar, C. C. Kan and P. Asherson. Cambridge, Cambridge
University Press.
van Dijk, F. E., M. Lappenschaar, et al. (2012). “Symptomatic overlap between attention-deficit/hyperactivity
disorder and borderline personality disorder in women: the role of temperament and character
traits.” Compr Psychiatry 53(1): 39-47.
van Lieshout, M., M. Luman, et al. (2013). “Does neurocognitive functioning predict future or persistence of
ADHD? A systematic review.” Clin Psychol Rev 33(4): 539-560.
van Lieshout, M., M. Luman, et al. (2016). “Neurocognitive Predictors of ADHD Outcome: a 6-Year Follow-up
Study.” J Abnorm Child Psychol.
Van Veen, M. M., J. J. Kooij, et al. (2010). “Delayed circadian rhythm in adults with attention-deficit/
hyperactivity disorder and chronic sleep-onset insomnia.” Biol Psychiatry 67(11): 1091-1096.
Widiger, T. A. and E. Simonsen (2005). “Alternative dimensional models of personality disorder: finding a
common ground.” J Pers Disord 19(2): 110-130.
Winsper, C., S. T. Lereya, et al. (2016). “The aetiological and psychopathological validity of borderline
personality disorder in youth: A systematic review and meta-analysis.” Clin Psychol Rev 44: 13-24.
Young, S., D. Moss, et al. (2015). “A meta-analysis of the prevalence of attention deficit hyperactivity disorder
in incarcerated populations.” Psychol Med 45(2): 247-258.
Zimmerman, M., I. Chelminski, et al. (2008). “The frequency of personality disorders in psychiatric
patients.” Psychiatr Clin North Am 31(3): 405-420, vi.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
17
GENERAL INTRODUCTION
1

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Published as:
Van Dijk, FE & Anckarsäter, H. (2011). ADHD, personality, and its disorders.
In J.K. Buitelaar, C.C.Kan & P. Asherson (Eds.), ADHD in Adults: Characterization, Diagnosis,
and Treatment (pp174-190). New York, Cambridge University Press.
ADHD, personality and its disorders
2

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
21
ADHD, PERSONALITY AND ITS DISORDERS
2
Introduction
From clinical, neurocognitive, and neurobiological perspectives (Faraone, 2005),
ADHD is regarded as a meaningful diagnosis today, in childhood as well as in
adulthood. However, the adult symptom profile and ADHD’s complex pattern of
overlap with other mental health problem constellations have yet to be detailed
and clarified (McGough & Barkley, 2004; Nigg, Blaskey, et al., 2002). So far, relatively
little attention has been paid to the relationship of ADHD to maladaptive
personality traits and personality disorders in adults (Lewinsohn et al., 1997;Nigg,
John, et al., 2002), most probably because of the theoretical hiatus between the
fields of child neuropsychiatry and adult personality and its disorders. Yet the
coexistence of ADHD and personality disorders certainly does matter, not only for
longitudinal prediction but especially for a deeper understanding of adult problem
arrays, for better phenotype characterization in neurobiological research, and for
the development of new treatment strategies.
ADHD is the term chosen for the fourth edition of the Diagnostic and
Statistical Manual of Mental Disorders (American Psychiatric Association, 1994),
whereas the two earlier editions – DSM-III (American Psychiatric Association,
1980) and DSM-III-R (American Psychiatric Association, 1987) – contained related
diagnostic definitions focusing on the inattentive facet of the syndrome disorder.
In DSM-IV, ADHD is diagnosed on the basis of problems with attention (inattentive
subtype), action and impulse control (hyperactive subtype), or both (combined
subtype).The current version of the International Classification of Diseases (ICD-10;
WHO, 1990) includes a definition based on hyperactivity – hyperkinetic disorder
– in which inattention is seen as a frequently complicating, coexisting problem
rather than as an aspect of the syndrome. As this textbook sets out from the ADHD
concept, we consistently use the term “hyperactivity,” which thus covers also the
description of hyperkinesia.
According to DSM-IV, the essential feature of a personality disorder is “an
enduring pattern of inner experience and behavior that deviates markedly from
what is expected in the individual’s culture.” This definition contains several
problems. Inner experiences are difficult to operationalize into diagnostic criteria,
whereas diagnosing personality disorders on the basis of behavioral patterns may
short-circuit attempts to “explain” behaviors by personality traits. At the same
time, systematic definitions of behaviors are the most readily available features
and will remain central among diagnostic criteria as long as interrater agreement
is a priority. In this situation, it is important to recognize behaviorally defined
disorders for what they are – relatively stable phenotypes for the study of cognitive,
biological, and/or social covariates.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
22
CHAPTER 2
Although Axis II of DSM-IV is theoretically available to record personality
disorders at all ages (with the exception of antisocial personality disorder), these
disorders are rarely diagnosed before young adulthood (i.e. at an age when a more
stable personality organization is being developed). Conversely, disorders classified
as “usually first diagnosed in infancy, childhood, or adolescence” are not often
assessed in adults. There is, however, every reason to assume that personality traits
or such differences in reaction patterns (temperaments) that form the basis on
which adult traits develop are discernible at a very early stage of child development
(Caspi et al., 2003). By tradition, temperaments and personality are defined on the
basis of the variance in the whole population, whereas psychiatric diagnoses, such
as ADHD or personality disorders, focus on small groups of persons with disabling
or distressful symptoms; these different perspectives have made it difficult to
understand that different designations may refer to similar underlying phenomena.
The growing awareness of “childhood” disorders, such as ADHD, among adults,
of temperament differences already in infancy, and of manifestations of some
Axis II disorders at least by adolescence (Lewinsohn et al., 1997) certainly calls
for cross-disciplinary reexamination of data and definitions.
ADHD and personality disorders
Antisocial personality disorderA number of diagnostic definitions have been proposed to capture specific personality
traits among persistently aggressive, destructive and dishonest persons, children
as well as adults. These definitions have mainly relied on behavioral criteria, such
as those in the DSM system, which defines ASPD as a pervasive and stable pattern
of aggressive and/or covert antisocial behaviors with onset before the age of 15,
corresponding to the diagnostic criteria for conduct disorder (CD). As an
“intermediary” diagnosis between ADHD and CD, the DSM system has included
oppositional-defiant disorder (ODD) to describe severely oppositional attitudes
and provocative behaviors. The combination of early-onset disruptive behaviors
with deficient emotional reactions to others and to the consequences of one’s
own behavior, as well as with dishonest and dominance- seeking interpersonal
strategies, has been described as “psychopathy,” first in the European psychiatric
tradition of personality disorders and then in North America, based on Cleckley’s
1951 book, The Mask of Sanity. This proposed syndrome has not been included in the
ICD or DSM classifications, even if the ICD-10 dissocial personality disorder includes
more criteria reflecting interpersonal and emotional aspects than the more
behavior-based DSM-IV definition of ASPD. However, this proposed syndrome has
had considerable impact on research on personality in association with criminal

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
23
ADHD, PERSONALITY AND ITS DISORDERS
2
behaviors, especially violence, not least because of its operationalization in the
PsychopathyChecklist (PCLR; Hare, 1980).
Factor analyses of the items in this checklist demonstrated a three-factor
structure comprising “destructive and impulsive behavioral patterns” (factor 3),
“blunted emotional integration of morally charged cognitions” (factor 2), and “a
glib, dominance-seeking and dishonest interpersonal style” (factor 1; Cooke &
Michie, 2001); Hare later proposed that the behavioral factor be split in two,
distinguishing impulsive behaviors from outright norm-breaking. By comparing
this factor structure to ADHD and other childhood-onset neuropsychiatric
problems, we hope to add clarity to the nosology of these factors. The behavioral,
third factor of the PCL-R and DSM-IV diagnostic criteria for ASPD and childhood
disruptive behavior disorders, especially CD and ODD but also ADHD, all contain
items that reflect impulsive, aggressive, or self-promoting behaviors with negative
consequences that are not sufficiently evaluated before action takes place. However,
the different diagnoses are based on criteria describing such behaviors in relation
to heterogeneous settings or situations that occur at different stages of development,
so that hyperactivity can be noted in an infant, whereas norm-breaking demands
at least a basic understanding of what norms are meant to be. Inattention is defined
by behaviors in task-related situations that require painstaking control, ODD by
interpersonal norm-breaking, and CD by infractions of social norms for behavior
during childhood, getting farther and farther into the realm of criminal acts as
the perpetrator gets older.
There is no lack of longitudinal, prospective studies assessing the long-term
development of ADHD or related definitions. Longitudinal studies that have used
clinical diagnostic definitions are briefly reviewed in Table 16.1. Because they
require diagnostics, the studies presented are mostly based on clinic referrals.
In addition, several population-based studies have followed representative cohorts
and are informative about longitudinal development and associations between
symptom assessments at various stages and outcomes; for example, studies from
San Francisco (Babinski et al., 1999), Pittsburgh (Loeber et al., 1998), Dunedin
(Moffitt & Caspi, 2001), Sweden (Klinteberg et al., 1993) and London (Farrington,
2000). We reference these population-based studies in the following sections when
appropriate, but let us start by summarizing the main findings from the clinical
studies; we then examine a number of methodological problems that need to be
considered when interpreting and using the results.
Comparisons of children identified as hyperactive to controls clearly and
consistently show increased risks for CD, ASPD, and criminality later in life (Table
16.2). It may even be concluded with reasonable confidence that a majority of clin-
ic-referred children with hyperactive ADHD (i.e. combined or hyperactive subtype),
at least during some phase, exhibit oppositional-defiant attitudes and behaviors,

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
24
CHAPTER 2
that at least one-third develop an early-onset CD, and that at least one-fifth go on
to develop adult ASPD, according to a recent meta-analysis based on all longitudinal,
prospective studies providing prevalence figures among index cases and controls
(Hofvander et al., 2009). Another salient finding was that only small subgroups of
those initially identified with hyperactivity or ADHD still met criteria for these
diagnoses at follow-up. Longitudinal studies invariably have to deal with attrition,
but the majority of the studies discussed here have high follow-up rates, and even
in the single study with the highest attrition, the one from Montreal, indirect
information from parents and official records supported that those retained in the
study were representative of the whole initial group, at least regarding criminal
histories (Weiss et al., 1985).
To avoid leaving the longitudinal literature with an oversimplified view of the
findings, we must examine some methodological problems in these studies. Let us
start with the manner of recruitment and the inclusion criteria for both index
subjects and controls. The longitudinal studies’ samples are either clinic referred
or population based. Clinic-referred children may not be representative of the
hyperactive children in the general population. This is difficult to establish as the
reports often omit more specific information on how and by whom the subjects
were referred. Criteria for study inclusion have included “minimal brain
dysfunction (MBD),” “hyperkinesia,” “hyperactivity/ impulsivity,” or ADHD, often
casually understood as ADHD in its broadest sense. Having found no study where
attention-deficit disorder without hyperactivity (ADD or ADHD inattentive type)
has been specifically investigated in relation to ASPD or associated features, we
conclude that inattention is not confirmed as a risk factor in this context.
Population based studies generally provide more detailed information on the
background population and ways of selection, but use broader definitions to
describe traits rather than conditions and often have arbitrary cutoffs within the
assumed normal distribution of problems (such as the lowest or highest quartile or
ratings below or above two standard deviations from the mean) to yield proxies for
diagnoses.
As hyperactivity is a common phenomenon among children, group comparisons
between index subjects and controls thought to form a representative sample from
the general population (including hyperactives) will differ from those using
controls selected to be “hypernormal” (i.e. without signs of this or that), and thus
they are no longer “normal” in a statistical sense. Controls recruited among
children referred for other mental health problems will naturally differ from
controls recruited among friends or from school registers. We also know that
subjects with hyperactivity or ADHD more often than not have other concomitant
behavioral or mental problems. It is therefore crucial to know whether such
problems precluded inclusion in the first place and whether the included children

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
25
ADHD, PERSONALITY AND ITS DISORDERS
2
were seen as representative of all hyperactive children or only of subgroups with
or without some specific combination of problem areas. For example, in the study
of outcome in the form of conduct problems, criminality, or diagnoses including
such behaviors, the extent to which index children had these or similar problems
already at inclusion and which definitions were used at follow-up are essential
information.
Longitudinal studies also challenge our capacity to keep the effects of time on
the studied phenomena constantly in mind. For the developmental problems of
interest to us, the degree of overlap between behavior types and thereby between
disorders depends on the age at which the cross-section is done. Unfortunately, the
majority of studies used broad age ranges already at inclusion, often recruiting
small children as well as prepubertal or pubertal adolescents. Operational criteria
for categorical diagnoses often mix current symptoms with lifetime problem
histories, which may obscure both developmental features and the role of
subsyndromal problems. Our targeted conditions are also most likely to represent
problems that follow a waxing and waning course and thereby may oscillate over
and under any diagnostic cut-off (Biederman et al., 2001; Lahey et al., 2002). These
methodological problems have to be considered when reassessing whether ADHD
in the absence of early-onset conduct deviance is really a risk factor for adult
antisocial behaviors (Lilienfeld &Waldman, 1990).
The Montreal study, which did not exclude children with conduct problems
at inclusion, demonstrated that all subjects who eventually developed ASPD had
an early onset of conduct problems as noted at the initial screening or at the
first follow-up (Herrero, Hechtman, & Weiss, 1994). In the Wisconsin study, adult
“predatory-overt” criminality was predicted by teenaged CD only (Barkley et al.,
2004). In the Developmental Trends Study, in which boys referred to outpatient
clinics had annual assessments, ADHD in the absence of conduct problems at
inclusion did not predict the later onset of CD (Loeber et al., 1995). In the Los
Angeles study, the absence of childhood conduct problems indicated a very low
risk for later CD and criminality, as illustrated by 16 children with hyperactivity
but no conduct problems who committed only minor adolescent offenses in two
cases and no adult offenses at follow-up (Satterfield & Schell, 1997). The Pittsburgh
study showed that ”callous unemotional behaviors,” depression, and onset of
marijuana use between 13 and 17 years of age predicted antisocial personality
development, whereas ODD and ADHD in the absence of conduct problems showed
no such association (Loeber et al., 2002). In the London based study, 8- and 9-year-old
boys were classified according to the presence or absence of hyperactivity
impulsivity and conduct problems. Follow-up results indicated that both factors
were independently predictive for adolescent convictions (age 10–16), whereas for
adult convictions (age 17–25), conduct problems alone remained a significant

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
26
CHAPTER 2
predictor (Farrington, 2000). A cluster analysis of teacher assessments of 13-
year-old boys in Sweden followed until ages 18–23 documented an increased risk
for criminality in the aggression-hyperactivity-inattention cluster, but not in the
hyperactivity-inattention cluster (Bergman & Magnusson, 1986). In several of the
studies, it was noted that the presence of even one single behavioral problem in
childhood (e.g. fighting, stealing, or lying) was an important risk factor for
subsequent antisocial development (e.g. Montreal, Los Angeles).The risk of
antisocial development was also higher in subjects with persistent hyperactivity
than in those who had remitted during the follow-up period. Children who did not
display any behavioral risk factors generally fared well (Herrero et al., 1994).
However, some studies have reported conflicting findings and claim that there
is a direct relationship between ADHD and ASPD, even in the absence of early-onset
CD. The New York City longitudinal study tried to establish study groups of
children with hyperactivity but no conduct problems at inclusion. Again, the
increased risk of adolescent CD and antisocial personality development was
significantly associated with previously noted, even low-grade, conduct problems,
just as in the Montreal study; however, in the New York study increased risk was
seen also among children who had reportedly shown no conduct problems at
inclusion. Hyperactivity in itself, even in the absence of early conduct problems,
was therefore claimed to constitute a risk factor for the later development of
antisocial behaviors and/or ASPD (Mannuzza et al., 2004). This claim is problematic
as conduct problems were not systematically assessed at inclusion, especially not
in the first New York study group. Included boys were reported not to have
aggressive behaviors as the “primary reason for referral” (Mannuzza et al., 1993) or
“clinically significant presenting problems involving aggression or other antisocial
behaviors” (Mannuzza et al., 1998). A report from the San Francisco study also
portrayed hyperactivity-impulsivity as an independent predictor of adult criminality,
which actually was the case only for some categories of less severe crimes among
males only. Crimes against people were again only predicted by conduct problems
(Babinski et al., 1999).
Many longitudinal studies have also included children of considerably varying
ages at the “baseline” assessments. In the New York City study discussed earlier,
children were included from the age of 6, and in the San Francisco study from the
age of 5, which means that no matter how carefully conduct problems were
assessed at inclusion, it would be possible for subgroups of children to develop an
early-onset CD after inclusion in the study, but before the age of 10 (which is the
DSM definition for early-onset CD) or at least the onset of puberty, and then go on
to have adult problems. The Pittsburgh study also included first, fourth, and fifth
graders, which may have influenced the authors’ perspective on overlap between
hyperactivity-impulsivity and conduct problems. The Boston study demonstrated

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
27
ADHD, PERSONALITY AND ITS DISORDERS
2
that, in children with ADHD, CD almost always developed before the age of 12
(Biederman et al., 1996), and it has been reported that the mean age at onset of CD
may be early in childhood (Kim-Cohen et al., 2005); however, we actually know
little about the development of CD in relation to prepuberty. The best hypothesis
therefore remains that ADHD is a precursor to early-onset conduct problems and
aggression and then, and only then, constitutes a major risk factor for adulthood
severe criminality and ASPD.
As for the nosological status of ODD, Loeber and co-workers (2002) proposed
that ODD symptoms act as an independent risk factor in addition to ADHD and CD
or as an intermediary state between those conditions. In most of the reviewed
studies (e.g. New York City, Developmental Trends, and Boston), however, ODD did
not predict CD development in a statistical sense, probably as it is so common
among children with ADHD at some stage. ADHD-based ODD and CD instead seem
to represent two sequential developmental complications of hyperactivity and
may, of course, result from interacting or additional risk factors in the form of
genetic factors associated with aggression or environmental factors related to
criminality. This does not make them “independent” disorders. In the Boston and
New York studies, virtually all children with ADHD who developed CD had already
developed ODD, and early-onset CD almost always develops out of a condition
marked by hyperactivity or the like (Lahey & Loeber, 1997).
Support for this notion also comes from twin studies that demonstrate
common genetic mechanisms underlying hyperactivity and oppositional/conduct
problems (Nadder et al., 2002; Silberg et al., 1996). A recent twin study examined
possible explanatory models for the overlap between ADHD and CD and found that
a model with “three different disorders” could be rejected, as both common genetic
and environmental effects for ADHD and CD could be identified (Rhee et al., 2008).
We have now arrived at the question of prediction. Is there any reliable way to
assess traits or features that give a valid prediction of later antisocial outcome
among children? Despite the number of studies presented, no predictive model
has yet been established, and in view of the figures presented, it seems reasonable
to assume that the increased risks are so unspecific that predictions will over
include children to such a degree that they become of little practical value. No
other feature is as predictive as early-onset antisocial behaviors (“nothing predicts
behavior as behavior”), and this effect precludes additions of predictive value from
other factors in statistical models, even if it could be interesting to study more
detailed characteristics of childhood behavior, such as age at onset or severity.
Underlying this continuity of aggression and antisocial behaviors, genetic effects
explain between 65% and 70% of the inter-individual variance in aggression (Burt,
2009; Frisell et al., 2010), and some of these effects are common with ADHD (Rhee
et al., 2008).

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
28
CHAPTER 2
Another salient feature that seems to be associated with poor outcomes of
ADHD is its persistence or that of some of its symptoms, such as restlessness, into
adulthood. In both the Montreal and New York studies, the risk of antisocial
behaviors was associated with the persistence of ADHD or of ADHD-related
symptoms. This, however, is not of much use for prediction. Lynam’s (1996)
suggestion that the combination of ADHD and CD identifies a group of “fledgling
psychopaths” may be consistent with the literature to the extent that this
combination represents the most risk laden subgroup, but as we have seen, at least
one-third of all children with ADHD also develop CD, and a considerable
proportion, between one-third and one-half in the cited studies, of these children
will not go on to be antisocial or criminal in adulthood. Note that the definitions
of “criminality” are quite loose and seldom include severe violent crimes. Figures
on the group level may also be elusive, as when 160 of 174 non theft crimes in the
Montreal study were perpetrated by four subjects (Hechtman &Weiss, 1986). Of
course, it would have been of societal good to be able to identify these 4 among the
initial 104 kids, but research at its current level is very far from being able to do so.
ADHD and the early-onset progression into ODD and CD ending up in ASPD
thus explain the third, behavioral factor of the proposed psychopathy construct.
The second factor of psychopathy describes deficient handling of stimuli and
words related to concepts such as “guilt,” “responsibility,” “love,” and “fear”
without appropriate accompanying emotional resonance, indicating both that the
person has a reduced or aberrant understanding of their meaning and will not
have the same access to emotions to guide behavioral reactions as others. This was
already referred to as “semantic blindness” by Cleckley (1951), who thought that it
was a core deficit in the condition he described. It is reflected by the operational
criteria for ASPD and has been demonstrated in many psychophysiological
research models (Hofvander et al., 2009). This emotional deficit facet of psychopathy
or ASPD was also associated both with ADHD and childhood autistic traits in a
retrospective study of adult offenders (Soderstromet al., 2005) and may be the
result of autistic-like traits interacting with disruptive behavior problems on the
ADHD-ODD-CD spectrum.
Finally on treatment, there is a striking contrast between our relatively
detailed knowledge about the longitudinal outcome of hyperactivity and the
means available for treatment aimed at preventing or changing a destructive
development. The established treatment for ADHD, psychostimulants, does not
have documented efficacy for treating either ODD or CD and nearly all the
longitudinal studies have included children who have actually been treated with
stimulants (Table 16.1). More recently, atypical neuroleptics have been used to treat
disruptiveness, but they are so far not recommended for general use because of
their considerable side effects and the lack of evidence for efficacy from controlled

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
29
ADHD, PERSONALITY AND ITS DISORDERS
2
trials. Other therapeutic measures for ADHD or CD, such as cognitive-behavior
therapy, group therapies, and psychoeducative measures or training, are equally
untested in the longitudinal developmental frame discussed in this chapter.
Borderline personality disorder BPD is a complex and seriously disabling mental disorder. It is estimated to occur
in about 1% or 2% of the general population (Torgersen, Kringlen, & Cramer, 2001),
and it is the most common personality disorder in psychiatric clinical settings.
Studies commonly suggest a three-factor structure consisting of a pervasive pattern
of disturbed relations to other persons, affective or emotional dysregulation, and
behavioral dyscontrol or impulsivity (Sanislow, Grilo, & McGlashan, 2000).These
factors are thought to express core dimensions of borderline psychopathology,
which may reflect underlying abnormal neurobiological processes involving
genetic and developmental susceptibility. The three factors are conspicuously
analogous to the factor solution proposed for psychopathy, again capturing the
triad of interpersonal attitudes, emotional processing, and behavior dyscontrol.
Even if this structure may merely represent one common to personality disorders,
there is an obvious overlap for at least the impulsivity of the third factor, and it is
also evident from a clinical point of view that patients with ADHD, ASPD and BPD
share symptoms of impulsivity. Of course, a common trait such as this one may
cause artifactual coexistence and obscure the aspects that really are specific for
the conditions.
Over the past years, a few studies have addressed a possible relationship
between ADHD and BPD. In contrast to the high-quality prospective follow-up
studies that have assessed the association between ADHD and ASPD, studies on
ADHD and BPD have generally relied on clinical cross-sectional designs. BPD is
mainly diagnosed in women and seems to have a presumed gender ratio that is the
reverse of that for ASPD (American Psychiatric Association, 1994). In addition, as
familial associations between ASPD and BPD are well demonstrated (Goldman,
D’angelo, & DeMaso, 1993), a closer investigation of the relationship between
ADHD and BPD seems well justified. In contrast to the previous section, here we
review the literature chronologically. Again we have to take into account several
methodological problems when interpreting the results. Ways of recruitment and
inclusion of subjects and controls, small sample sizes, and the definitional vagaries
that were already discussed have to be kept in mind.
Research on ADHD symptomatology and BPD started in the early 1980s.
Andrulonis and co-workers identified three distinct subtypes of BPD in a group of
106 hospitalized adult borderline patients: those with no history of organicity;
those with a history of trauma, encephalitis, or epilepsy; and those with a history
of attention deficits or learning disabilities. They reported a considerable overlap

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
30
CHAPTER 2
Table 1 The main reviewed prospective longitudinal studies on the association between childhood hyperactivity (using clinical diagnostic categories at inclusion) and antisocial personality disorder
Study, Main Reference
Approximate years of inclusion Cases Controls Treatment Follow-up
Clinic-referred study groups
MontrealWeiss et al., 1985Hechtman & Weiss, 1986
1962-1965 104 (95 boys and 9 girls) long-term hyperactive children (aged 6-12)
45 matched ‘hypernormal’a
school-mate controls
4 received psychostimulants, and 20 a conventional high-dose neuroleptic
59% were followed up after 15 years at 21-33 years of age, by blind and non-blind clinical assessments, court records, and for those lost to follow-up by parental contacts, contacts over the phone etc.
New YorkGroup 1Gittelman et al., 1985Mannuzza et al., 1993Group 2Mannuzza et al., 1991Mannuzza et al., 1998Group 1 & 2Mannuzza et al., 2004
1970-1977 115 (Group 1) and 111 (Group 2) hyperactive boys (aged 6-12)
178 matched hypernormal non-psychiatric outpatient controls
All subjects had “medication and/or behavior therapy”
About 90% were followed after a mean interval of 16.1 and 17 years at mean ages 26, 24.1 och 23.5, by blind structured assessments and, for the first group, by official files.
BostonBiederman et al., 1992 (basic), 1996 (follow-up)
1992 basic1996 follow-up
140 referred or recruited boys with ADHD (aged 6-17)
120 unmatched control boys from out-patient services or recruited by advertisements
89% had a life-time history of treatment with psychostimulants, 44% during the follow-up period
91% were followed-up after 4 years by blind/semiblind new assessments
Los AngelesSatterfield et al., 1982
1970-1972 110 hyperactive boys between (aged 6-12)
75 matched payed public school controls, 13 non-ADHD brothers of cases
“most” or “all” subjects had CS medication 81% were followed up until age 25 through official records
WisconsinBarkley et al., 2004Fischer, 2002
1979-1980 158 consecutive hyperactive children (144 boys, 14 girls, aged 4-12)
81 matched non-hyperactive controls recruited among the subjects’ friends
22% vs 0% had treatment with stimulants during the high-school years
≥90% were followed up after a mean interval of 13.8 years at between 19-25 y o a through structured interviews and official records.
Developmental Trends StudyLoeber et al., 1987
1987 177 out-patient boys at three clinics, (aged 7-12), 75% of whom referred for disruptive behaviours
No controls Medication in an unknown proportionb but required to discontinue two days prior to assessments
About 90% remained in the study and were followed by blind structured assessments yearly until ages 18-19.
Population-based study
Rasmussen & Gillberg, 2000 1977 61 7-years old children (47 boys, 14 girls) with ADD with or without DCD (about 90%), most of whom met DSM-IV criteria for AD/HD, or with DCD (about 10%)
51 population-based controls (27 boys, 24 girls) matched for SES and age
No one had medication with psychostimulants 90% were followed up with blind structured assessments and official files at 22 years of age.
Note: Several well-known longitudinal studies are referred in the text but not included in the table as
they did not use clinical diagnostics at baseline (e.g. the Dunedin and Philadelphia studies). For a more
comprehensive table including these studies and meta-analyses of results please see Hofvander et al.,
2009.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
31
ADHD, PERSONALITY AND ITS DISORDERS
2
Table 1 The main reviewed prospective longitudinal studies on the association between childhood hyperactivity (using clinical diagnostic categories at inclusion) and antisocial personality disorder
Study, Main Reference
Approximate years of inclusion Cases Controls Treatment Follow-up
Clinic-referred study groups
MontrealWeiss et al., 1985Hechtman & Weiss, 1986
1962-1965 104 (95 boys and 9 girls) long-term hyperactive children (aged 6-12)
45 matched ‘hypernormal’a
school-mate controls
4 received psychostimulants, and 20 a conventional high-dose neuroleptic
59% were followed up after 15 years at 21-33 years of age, by blind and non-blind clinical assessments, court records, and for those lost to follow-up by parental contacts, contacts over the phone etc.
New YorkGroup 1Gittelman et al., 1985Mannuzza et al., 1993Group 2Mannuzza et al., 1991Mannuzza et al., 1998Group 1 & 2Mannuzza et al., 2004
1970-1977 115 (Group 1) and 111 (Group 2) hyperactive boys (aged 6-12)
178 matched hypernormal non-psychiatric outpatient controls
All subjects had “medication and/or behavior therapy”
About 90% were followed after a mean interval of 16.1 and 17 years at mean ages 26, 24.1 och 23.5, by blind structured assessments and, for the first group, by official files.
BostonBiederman et al., 1992 (basic), 1996 (follow-up)
1992 basic1996 follow-up
140 referred or recruited boys with ADHD (aged 6-17)
120 unmatched control boys from out-patient services or recruited by advertisements
89% had a life-time history of treatment with psychostimulants, 44% during the follow-up period
91% were followed-up after 4 years by blind/semiblind new assessments
Los AngelesSatterfield et al., 1982
1970-1972 110 hyperactive boys between (aged 6-12)
75 matched payed public school controls, 13 non-ADHD brothers of cases
“most” or “all” subjects had CS medication 81% were followed up until age 25 through official records
WisconsinBarkley et al., 2004Fischer, 2002
1979-1980 158 consecutive hyperactive children (144 boys, 14 girls, aged 4-12)
81 matched non-hyperactive controls recruited among the subjects’ friends
22% vs 0% had treatment with stimulants during the high-school years
≥90% were followed up after a mean interval of 13.8 years at between 19-25 y o a through structured interviews and official records.
Developmental Trends StudyLoeber et al., 1987
1987 177 out-patient boys at three clinics, (aged 7-12), 75% of whom referred for disruptive behaviours
No controls Medication in an unknown proportionb but required to discontinue two days prior to assessments
About 90% remained in the study and were followed by blind structured assessments yearly until ages 18-19.
Population-based study
Rasmussen & Gillberg, 2000 1977 61 7-years old children (47 boys, 14 girls) with ADD with or without DCD (about 90%), most of whom met DSM-IV criteria for AD/HD, or with DCD (about 10%)
51 population-based controls (27 boys, 24 girls) matched for SES and age
No one had medication with psychostimulants 90% were followed up with blind structured assessments and official files at 22 years of age.
a Hypernormal meaning that controls have been selected on a number of criteria, such as not being
hyperactive, and are therefore not representative for the general population. b When stated that no information is provided, this is based on the main references as cited. Some of
these studies are published in a large number of papers and chapters and even if we have scrutinized
this literature to the best of our ability, some sources of information may have been missed.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
32
CHAPTER 2
(about 25%) between the latter two subtypes and minimal brain dysfunction (a
term that was abandoned in 1980 when ADD was introduced in the DSM, with a
considerable conceptual overlap between MBD and ADD). The patients with
minimal brain dysfunction consisted mainly of males with early developmental
difficulties. They were characterized by aggressive and hyperactive behavior,
academic difficulties during childhood, and antisocial acting out with drug/
alcohol abuse during adolescence (Andrulonis et al., 1981, 1982). These studies
showed that a significant subgroup of borderline patients have a “spectrum”
disorder on an organic brain dysfunction continuum, which includes symptoms
that have later been referred to the ADHD domain.
Table 2 Adult or follow-up outcomes of children initially identified with hyperactivity or related diagnoses vs. controls
StudyPersistence of AD/HD
Conduct Disorder
Antisocial personality disorder (cases vs. controls)
Criminality (various measures) Incarceration
Montreal 36% vs 2% had “at least one moderately or severely disabling symptom”
“about 10% … antisocial disturbed”
23% vs 2.4% Court appearances 18% vs 5%Any offence 68% vs 59%Non-theft convictions: 5% vs 0% (just 4% among those lost to follow-up)
None mentioned
New YorkGroup 1Group 2Group 1&2
8% vs 1% (group 1)4% vs 0% (group 2)
27-32% vs 8% 18% vs 2%(group 1)12% vs 3%(group 2)
Arrested 39% vs 20%, convicted 28% vs 11% aggressive crimes 6% vs 2% (group 1)No criminal record follow-up reported(group 2)
5% vs 0% (group 1)2% vs 0% (group 2)
Boston 58% vs 6% “full or subthreshold” ADHD, more common when combined with ODD/CD
23% vs.3% Not within range of follow-up
Not within range of follow-up Not within range of follow-up
Los Angeles Not assessed Not Assessed Not assessed Juvenile arrests: 46% vs 11%Felony arrests: 21% vs 1%Recidivism: 9% vs 0%
Institutionalized as adolescents 25% vs 1%Incarcerated as adults 12% vs 0%
Wisconsin 5% vs 0% 31% vs 11% developed CD at some stage
21% vs 4% Arrested ≥ 2 times 40% vs 12% None mentioned
Gothenburg Severe hyperacitivity/impulsivity 15% vs 2%Severe inattention 44% vs 7%Combination of both 9% vs 0%
6% vs 7% 18% vs 2% Any criminal conviction 19% vs 0% None mentioned

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
33
ADHD, PERSONALITY AND ITS DISORDERS
2
At least a decade later, looking for antecedents of personality disorders in
childhood, Rey and coworkers examined continuities between Axis I disorders in
adolescents and personality disorders in young adults. They found that the
adolescents with disruptive disorders were more likely at follow-up to have a
personality disorder on the dramatic/impulsive cluster, which includes both BPD
and ASPD, than those with emotional disorders. All disruptive disorders were
associated with a wide range of personality psychopathology in adulthood. Specific
associations were found between CD and ASPD and between ADHD (with
hyperactivity) and BPD. The authors suggested that disruptive disorders in
childhood might be re-conceptualized as disorders of personality rather than as
Table 2 Adult or follow-up outcomes of children initially identified with hyperactivity or related diagnoses vs. controls
StudyPersistence of AD/HD
Conduct Disorder
Antisocial personality disorder (cases vs. controls)
Criminality (various measures) Incarceration
Montreal 36% vs 2% had “at least one moderately or severely disabling symptom”
“about 10% … antisocial disturbed”
23% vs 2.4% Court appearances 18% vs 5%Any offence 68% vs 59%Non-theft convictions: 5% vs 0% (just 4% among those lost to follow-up)
None mentioned
New YorkGroup 1Group 2Group 1&2
8% vs 1% (group 1)4% vs 0% (group 2)
27-32% vs 8% 18% vs 2%(group 1)12% vs 3%(group 2)
Arrested 39% vs 20%, convicted 28% vs 11% aggressive crimes 6% vs 2% (group 1)No criminal record follow-up reported(group 2)
5% vs 0% (group 1)2% vs 0% (group 2)
Boston 58% vs 6% “full or subthreshold” ADHD, more common when combined with ODD/CD
23% vs.3% Not within range of follow-up
Not within range of follow-up Not within range of follow-up
Los Angeles Not assessed Not Assessed Not assessed Juvenile arrests: 46% vs 11%Felony arrests: 21% vs 1%Recidivism: 9% vs 0%
Institutionalized as adolescents 25% vs 1%Incarcerated as adults 12% vs 0%
Wisconsin 5% vs 0% 31% vs 11% developed CD at some stage
21% vs 4% Arrested ≥ 2 times 40% vs 12% None mentioned
Gothenburg Severe hyperacitivity/impulsivity 15% vs 2%Severe inattention 44% vs 7%Combination of both 9% vs 0%
6% vs 7% 18% vs 2% Any criminal conviction 19% vs 0% None mentioned

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
34
CHAPTER 2
Axis I diagnoses (Rey et al., 1995).Thus the studies of both Andrulonis and Rey
attempted to put BPD into a developmental context and suggested a significant
relationship between ADHD features and BPD.
Fossati and co-workers tried to overcome some limitations of these pioneer
studies by evaluating the presence of specific associations between retrospectively
assessed childhood ADHD symptoms and adult BPD in a controlled design. They
administered the Wender Utah Rating Scale (WURS), a self-report instrument, to
42 consecutive BPD subjects and four control groups: admitted subjects (1) with
any cluster B personality disorder diagnosis, (2) with any cluster A or cluster C
personality disorder diagnosis, (3) with no personality disorder diagnosis, and (4)
nonclinical volunteers. This study showed a significant relationship between the
presence and severity of childhood ADHD symptoms and adult BPD. No less than
60% of the BPD subjects had probably met criteria for ADHD in childhood, even
after controlling for ASPD (Fossati et al., 2002). Such figures have to be interpreted
as suggesting the etiological heterogeneity of both disorders, and it remains
unclear which characteristics are specifically related, possibly expressing the
same underlying susceptibility, and which are not.
The specificity of clinical ADHD characteristics in adults with BPD has also
been investigated using the self-report Attention Deficit Scale for Adults (ADSA).
The statements in the ADSA relate to a wider range of characteristics than those
found in the DSM-IV, including mood lability, temper, disorganization, and
impulsivity. Dowson and co-workers showed that seven of the nine scales of the
ADSA discriminated between ADHD and BPD, despite the overlap of clinical
features involved in the two syndromes. The seven scales showing significant
intergroup differences involved attention, organization, and persistence. Impaired
task and goal persistence were the main discriminators between those with ADHD
and those with BPD, with the ADHD group being the more impaired. Nonsignificant
differences were found for two scales that were related to impatience, examples of
aggression, taking undue risks, and failure to take the likely results of actions into
account (Dowson et al., 2004). These findings seem to be in line with earlier results,
but they also provide some indication that symptoms referring to the inattention
domain of ADHD are to be specially considered in the relationship between ADHD
and BPD. A limitation of this study may be that ADHD was not excluded from the
BPD group nor was BPD excluded from the ADHD group.
In contrast to these studies, Kooij and co-authors used semi-structured clinical
interviews in the assessment procedure in their study on the relationship between
ADHD and coexisting BPD and ASPD. Their results showed that, among 53 referred
ADHD patients, 11% presented with a subthreshold diagnosis and only 4% with a
full BPD diagnosis. The most frequent symptom overlap was found for affective
instability and inappropriate anger, symptoms that have been identified as

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
35
ADHD, PERSONALITY AND ITS DISORDERS
2
ADHD-associated features (Kooij et al., unpublished data). The authors explained
the difference between the prevalence of subthreshold and full diagnostic
occurrence of BPD by the use of a clinical interview to establish the ADHD
diagnosis, a more restrictive scoring system than relying on self-report scores only.
Data from ongoing research on the relationship between adult ADHD (i.e.
meeting ADHD criteria in childhood as well as in adulthood, also using semi
structured clinical interviews) and BPD in 103 clinically referred female adults
showed that 33% of a group of 63 patients with BPD also have ADHD and that 15%
of 40 adult ADHD female patients also meet criteria for BPD (Van Dijk et al.,
unpublished data). Trying to further clarify the relationship between ADHD and
BPD, the investigators used latent class analyses (LCA; McCutcheon, 1987) of the
ADHD and BPD symptoms. LCAis a statistical technique that generates hypotheses
and may thus supplement standard diagnostic categories. Four mutually exclusive
classes of patients were identified: one with only ADHD symptoms; one with BPD
symptoms and ADHD symptoms of hyperactivity; one with BPD symptoms and
ADHD symptoms of inattention, hyperactivity, and impulsivity; and one with BPD
symptoms and ADHD symptoms of inattention and hyperactivity. The hyperactive
symptoms were relatively high across all classes, indicating that this is an
unspecific symptom domain with poor differentiating value between ADHD and
BPD. A transition model, associating the adult classes with retrospective childhood
ADHD symptomatology, showed, in addition to the expected associations between
adult and childhood ADHD symptomatology, a remarkable probability that an
outcome characterized by both ADHD and BPD symptoms in adulthood might be
associated with a childhood without any significant ADHD symptomatology (i.e.
subclinical hyperactivity), whereas an adult outcome with predominantly BPD
symptoms could be traced back to combined ADHD symptoms in childhood. These
data would fit a model in which the ADHD subtypes are not viewed as discrete
categories that are permanent over time; they are also in line with the previously
discussed findings of heterotypic diagnoses at adult follow-up in the longitudinal
studies (Table 16.2) or in the Dunedin study, in which a follow-up at age 26 found
formerly disruptive children across all adult diagnostic categories without the
expected specificity (Kim-Cohen et al., 2003).
Although identifying a subgroup of patients with both ADHD and BPD may
lead to an alternative, more beneficial treatment, research on the consequences of
coexisting ADHD and borderline personality disorder is limited. Two case reports
have shown possible subjective and neurocognitive benefits from a psychostimu-
lant (methylphenidate) in two patients with BPD and ADHD (Hooberman & Stern,
1984; Van Reekum & Links, 1994). Schulz and co-workers used amphetamine to
investigate the hypothesis that patients with BPD are prone to psychosis following
ingestion of a dopamine agonist, but found that patients with a borderline

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
36
CHAPTER 2
diagnosis without comorbidity instead improved in their general clinical condition
(Schulz et al., 1988). Considering the lack of research in this area, studies of phar-
macotherapeutical alleviation of ADHD symptoms in patients presenting with
personality disorders are urgently needed.
Dimensional personality traits
As we have seen, in the DSM system, personality disorders are recorded on a
separate axis and, in accordance with the ICD system, are defined categorically.
Both principles are controversial and disputed by most experts because empirical
data lend no support for a delineation of personality disorders from other mental
disorders or for a categorical structure of personality traits (Livesley, 2001). To
overcome the limitations of the currently used diagnostic categories, Widiger has
proposed that dimensional models of personality may be helpful in addressing
problems of excessive co-occurrence, heterogeneity among persons with the same
diagnosis, and artifactual or epiphenomenal diagnostic distinctions (Widiger, 2005).
Categorical and dimensional perspectives on personality disorders may also be
seen as complementary, and each offers valuable insights (Pickles & Angold, 2003).
A variety of alternative dimensional models have been proposed to replace the
categorical DSM-IV personality disorders in future versions of the manual (for an
overview see Widiger & Simonsen, 2005).However, there is still considerable debate
about which dimensional system is most valid and useful (Verheul, 2005). In spite
of the apparent discrepancies among the competing models for describing
personality structure, they have remarkable convergence on a set of three to five
basic personality dimensions. The five-factor model (FFM; Widiger & Costa, 1994)
and the Temperament and Character Inventory (TCI; Cloninger, Swrakic, &
Przybeck, 1993) are organized explicitly with respect to five and seven higher
order factors, respectively, with each broad domain further differentiated into
more specific facets or subscales. These two models are the ones used most
frequently in studies on dimensional models in relation to ADHD in adults. In this
section we review the studies regarding empirical associations between ADHD
and several personality traits.
Cloninger’s modelCloninger’s biopsychosocial theory of personality is based on the assumption that
personality involves four temperament dimensions and three character
dimensions. The dimensions of temperament measure individual differences in
basic emotional drives and are Harm Avoidance (i.e. pessimistic and anxious versus
optimistic and risk-taking), Novelty Seeking (i.e. impulsive and irritable versus

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
37
ADHD, PERSONALITY AND ITS DISORDERS
2
rigid and stoical), Reward Dependence (i.e. sociable and warm versus aloof and
cold), and Persistence (i.e. persevering and ambitious versus easily discouraged and
lazy). The character dimensions measure individual differences in higher cognitive
processes that define a person’s style of mental self-government: the character
traits are described as Self-Directedness (i.e. responsible and resourceful versus
blaming and inept), Cooperativeness (i.e. helpful and principled versus hostile and
opportunistic), and Self-Transcendence (i.e. intuitive and insightful versus concrete
and conventional; Cloninger, 1987; Cloninger et al., 1993). A self-rating instrument,
the Temperament and Character Inventory (TCI; Cloninger et al., 1993), has been
developed to measure the model’s seven personality dimensions. Presence of a
personality disorder is indicated by presence of character immaturity (especially
by low Self- Directedness and/or Cooperativeness), whereas the type of disorder is
decided by the temperament configuration (Cloninger, 2000; Svrakic et al., 1993).
A few studies have investigated the TCI profiles in subjects with ADHD. Downey
and colleagues (1997) used the Tri Personality Questionnaire, a precursor to the
TCI, and found that ADHD subjects scored significantly higher than normal
subjects on the temperament scales of Novelty Seeking and Harm Avoidance.
A more recent study (Lynn et al., 2005) tested the hypothesis that Novelty Seeking
and ADHD are associated and that their association is due, in part, toDNA
variability at the DRD4 gene.When interpreting their results, it is important to
keep in mind that the subjects in the study were parents of ADHD affected sib
pairs. Not all of them had current ADHD or a lifetime history of ADHD, and it is
possible that the results cannot be generalized to other adults with ADHD. The
results partly confirmed the findings of Downey and co-workers, identifying a
strong role for Novelty Seeking as a predictive factor for ADHD diagnostic status.
However, this association was not accounted for by the presence of a risk allele at
DRD4. Consequently, it remains impossible to clarify whether Novelty Seeking
increases the risk for ADHD or whether the presence of ADHD influences the
development of a Novelty Seeking temperament or whether the two are merely
different conceptualizations of a common phenomenon. The authors also reported
the divergent finding that the temperament scale of Self-Transcendence was
actually associated more strongly with ADHD than was Harm Avoidance. Further,
they identified a significant role for the character dimension Cooperativeness,
consistent with the notion that ADHD symptoms in childhood may hamper the
maturation of character.
Another clinical study used the TCI to describe personality development and
disorders in relation to ADHD symptomatology and autism spectrum disorders
(ASD) among 240 subjects with neuropsychiatric disorders (of whom147 had
ADHD; Anckarsater et al., 2006).The assumption was that childhood-onset neuro-
psychiatric disorders would be reflected as “difficult temperaments,” deficits in

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
38
CHAPTER 2
character maturation, and personality disorders. The self-rated personality traits
in the sample differed dramatically from those reported by subjects in the general
population. Extremely low scores for Self-Directedness and Cooperativeness were
recorded among all subjects with neuropsychiatric disorders, again consistent
with the notion that these early problems form obstacles to character maturity. In
addition, ADHD was specifically associated with high Novelty Seeking and high
Harm Avoidance.
As these studies did not assess personality structure in subgroups of subjects
with ADHD but without personality disorders, it is difficult to pin specific personality
profiles to ADHD in itself. The cited ongoing study by Van Dijk and co-workers
using latent class analyses (McCutcheon, 1987) on the relationship between female
adult ADHD and BPD examined TCI profiles for the four latent classes of ADHD and
BPD symptoms. In this study, High Novelty Seeking was found in all classes except
for the class with symptoms of BPD and only the hyperactivity aspect of ADHD.
The highest Novelty Seeking temperament scores were found in that class of
patients with both symptoms of BPD and symptoms in all areas of ADHD. High
Harm Avoidance, low Cooperativeness, and low Self- Directedness were specifically
related to classes containing BPD symptoms.
An outspoken Novelty Seeking temperament suggests a vulnerability for the
development of ADHD and co-occurring BPD. Contrary to patients with combined
ADHD and BPD symptoms, patients with ADHD symptoms alone show normal
character development.
The Five-Factor ModelThe “Big Five” represents the hierarchical organization of five major dimensions of
normal adult personality and provides the most widely accepted description of
higher order personality traits. The five-factor model (FFM) includes the dimensions
of Neuroticism, Extraversion, Openness to Experience, Conscientiousness, and
Agreeableness. Each of these domains is composed of six subfactors called facets
(Costa & McCrae, 1992). As in the case with Cloninger’s temperament and character
dimensions, only a few studies have investigated associations between the Big Five
personality dimensions and ADHD.
Braaten and Rosen (1997) found that elevated self-reported DSM-III-R ADHD
symptoms in undergraduates correlated with high Extraversion and high Neuroticism.
The limitation here was the use of college students and assessment based on self-
reports only. Nigg and co-authors (Nigg, John, et al., 2002) subsequently obtained
larger and more diverse samples for the investigation of personality traits and ADHD
symptoms. They used three ADHD self-report instruments, trying to overcome the
limitation that the findings would be attributable to one particular approach of
assessing ADHD, as well as the NEO Five Factor Inventory (NEO FFI). They found

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
39
ADHD, PERSONALITY AND ITS DISORDERS
2
that ADHD symptoms were consistently related to low Conscientiousness, low
Agreeableness, and high Neuroticism. However, these correlations did not fully
explain the variation in ADHD symptoms. The data showed that attention problems
were related primarily to low Conscientiousness and high Neuroticism, and hyper-
activity-impulsivity was related to low Agreeableness. This study found no reliable
association with ADHD for Extraversion or Openness (Nigg, John, et al., 2002).
Another study addressing the relationship of ADHD symptoms with the FFM
came from Canada (Parker, Majeski, & Collin, 2004). This study used the Conners’
Adult ADHD Rating Scale (CAARS) and the NEO-FFI in a sample comprised of
psychology students. They used DSM-IV cut-off scores to categorize three groups:
the inattentive ADHD type, the hyperactive-impulsive ADHD type, and non-ADHD
controls. Contrary to the study of Nigg and co-workers, but in line with the work of
Braaten and Rosen, the Canada study found consistent associations between high
Extraversion and the hyperactive-impulsive ADHD symptoms, whereas inattentive
symptoms were not related to this personality dimension. High neuroticism was
instead found to be a significant predictor of both inattention and hyperactivity -
impulsivity symptomatology, and again, just as in the study by Nigg and co-workers,
the most powerful predictor for inattention scores was low Conscientiousness, and for
hyperactivity-impulsivity it was low Agreeableness. Both personality dimensions
were also significant predictors for the other symptom group and for total ADHD
scores.
Even considering that these studies relied on self-reported ADHD symptom
ratings, their findings nevertheless suggest substantial associations between ADHD
symptoms and four of the Big Five personality dimensions: high Neuroticism, high
Extraversion, low Conscientiousness, and low Agreeableness. However, Openness
appeared not to be related to ADHD symptomatology. The overall results from
research using the FFM overall seemless consistent and less specific than the TCI
results that associated ADHD with high Novelty Seeking and, when there was also
a personality disorder, with character immaturity.
Neurocognitive and brain domains
Its clinical presentation has suggested that ADHD is a neuropsychological disorder,
and attention and executive functions have become the focus of most theories
concerning its neuropsychological basis (Seidman et al., 2004). Both ASPD and BPD
also contain domains of emotional aberrations. Deficits in theory of mind – the
cognitive end result of both social understanding and emotional understanding
– have been shown across these categorical definitions (Sodian, Hulsken, &
Thoermer, 2003). However, the differentiation of ADHD and associated disorders

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
40
CHAPTER 2
on the neuropsychological level has proved much more difficult than first expected
(Nigg, 2000), and many a simplified model has failed to conform to empirical data
when put to the test. The executive and motivation systems of the brain may well
be involved in ADHD just as in various personality traits (Nigg, Butler, et al., 2002).
Executive functions have also been found to be less specific on the neuropsycho-
logical level than first assumed and seem to develop in close connection with
empathy and emotional processing (Pacherie, 1997; Perner, 1998), possibly because
self-restraint also boosts comprehension of others and emotional reactivity and
processing are necessary elements of self-restraint. Empathy is a highly complex
function based on nonlinear interactions among theory of mind, emotional
mirroring, executive functions, and situational determinants (Anckars¨ater &
Cloninger, 2007). It is therefore obvious that prior designations of specific brain
systems thought to be involved in either social functioning (especially the limbic
circuitry) or executive functions (especially the prefrontal cortex) have to be
reinterpreted in a wide “social brain,” encompassing interactions among widely
disparate systems.
Analogously, most attention in the psychiatric context has been given to the
systems using monoamines as neurotransmitters, and there is indeed every reason
to assume that monoamines are of central importance: almost all major psycho-
pharmaceuticals have been shown to exert their effects through modulations of
these systems. The complex phenotypes we have approached in this chapter,
however, probably relate to many other transmitter systems; for example,
modifications of dopamine activity may only be hoped to modify some very specific
parts of the problem constellations. In contrast, it is obvious that the pharmacolog-
ical angle in longitudinal research is weak and that drug response may form a key
to disentangling complex phenotypes. Preliminary evidence has also implied a
shared genetic origin for executive functions and personality disorders or
associated features (Coolidge, Thede, & Jang, 2004).
The early “effortful control” (regulation) system in young children is thought
to involve the same neural system as the executive processes related to ADHD,
combined type. A critical role of this system in the developing personality is
reflected in research showing that effortful control is positively related to the
development of conscience and negatively to the expression of aggression
(Kochanska, Murray, & Coy, 1997; Rothbart & Ahadi, 1994).The definition of
temperament as individual differences in constitutionally based (emotional,
motor, and attentional) reactivity and self-regulation (“effortful control”)may
allowus to consider both the initial state of individual differences and the early
development of emotional and attentional systems (Rothbart, 2004). Multiple
pathways in early development related to distinct kinds of temperamental or
cognitive vulnerability might form the basis for phenotypical definitions,

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
41
ADHD, PERSONALITY AND ITS DISORDERS
2
dimensional or categorical depending on the research models they are applied in,
but clearly defined in relation to specific contexts, developmental stages, and
challenges such as stimuli or tasks.
Ultimately, the pathways between early temperament and future personality
(and possible psychopathology) are likely to be complex and nonlinear, because
children’s development unfolds on the basis of partially genetic constitutional
factors through the context of social relationships, cognition, and experience.
Both continuity and change must eventually be understood in such contexts
(Rothbart, 2004), and it will be necessary for future research to account for all
these aspects to arrive at a better understanding of the role of early neurodevelop-
mental variants in shaping adult personality.
Summary and conclusion
In this chapter we have dealt with complex concepts and issues concerning the
relation of ADHD to personality disorders and traits. We make no pretense at
completeness, but we hope to have contributed to the discussion aiming at a better
understanding of ADHD in relation to personality.
Based on this literature review, we would like to propose the following distinctions
as providing a plain account of the risk for ASPD and criminality carried by ADHD.
Early-onset disruptive behavior disorder (corresponding to the combination of
ADHD, ODD, and CD, or hyperkinetic conduct disorder) carries a sharply increased
risk for later ASPD and aggressive criminality. The adult personality disorder consists
of destructive behavior patterns generally accompanied by deficient or aberrant
emotional processing of thought and reactions. This concept contains most of the
variation in what has been called “psychopathy,” which because of its moral
connotations is an unsuitable term in clinical practice. The disorder is associated
with an increased risk both for ”hands-on” criminal acts and the remaining
unique factor of psychopathy (referred to as the first factor of the PCL-R); that is,
the wicked way of seeking dominance over others through manipulation and
deceit. It remains an open question whether such undesired behavioral consequences
should be dealt with as mental disorders. Thorough clinical diagnoses of the
problem constellation in a developmental perspective are always warranted, not
least as a large proportion of children with early-onset disruptive behaviors also
have attention and learning problems, other forms of social interaction and
communication problems that sometimes correspond to the autism spectrum
definitions, and a wide range of psychiatric coexisting problems. The clinical
assessment forms the basis for possible treatment strategies. In the absence of
early-onset conduct problems, ADHD per se, inattentive or combined type, has not

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
42
CHAPTER 2
been linked to an increased risk for an adult antisocial development, and late-onset
(adolescent) conduct problems do not share the same developmental basis or
associations to other problem types as the early-onset form nor its grave prognosis.
With regard to associations between ADHD and BPD, systematic data are
meager. Overall, the reviewed studies mainly show symptom overlap between
ADHD and BPD in the disruptive hyperactivity-impulsivity domain, whereas
inattention characteristics are likely to differentiate among the problem types.
More, as well as more diverse, research is needed to better understand the
relation ship between ADHD and BPD, to clearly unravel their shared characteristics,
to propose possible pathways leading to a BPD outcome, and to improve the
understanding of possible truly unique aspects of the categories.
Then, we discussed ADHD in relation to personality traits, as defined by the
Big Five and Cloninger’s temperament and character model. ADHD as a clinical
disorder seems to express an extreme end of extroversion or novelty seeking, with
possible hampered character development or decreased conscientiousness. Harm
avoidance may interact in creating the risk for BPD among subjects with ADHD.
However, because few studies included subgroups with ADHD in which adult
personality disorders had been controlled for, it is difficult to draw specific
conclusions on the delineations and overlap among ADHD, personality disorders,
and personality traits.
Finally, we pointed out the critical role of early regulation and reactivity
systems in the development of temperamental or cognitive vulnerability. In
closing this chapter, we again want to stress the importance of the integration of
theories on psychopathology, temperament, and cognition, which represents a
promising future line of research.
AcknowledgmentsAgneta Brimse and Monika Montell are gratefully acknowledged for their expert
secretarial assistance. The study of longitudinal studies was carried out in close
collaboration with Bj¨orn Hofvander and Daniel Ossowski.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
43
ADHD, PERSONALITY AND ITS DISORDERS
2
References
American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders. 3rd ed.
Washington DC: American Psychiatric Association.
American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders. 3rd ed. rev.
Washington DC: American Psychiatric Association.
American Psychiatric Association. (1994). Diagnostic and Statistical manual of mental disorders. 4th ed.
Washington DC: American Psychiatric Association.
Anckars¨ater H, Cloninger CR. (2007).The genetics of empathy. In: Farrow T, Woodruff P, eds. Empathy in
Mental Illness and Health. New York: Cambridge University Press: 261–88.
Anckars¨ater H, Stahlberg O, Larson T, Hakansson C, Jutblad SB, Niklasson L, et al. (2006).The impact of
ADHD and autism spectrum disorders on temperament, character, and personality development. Am
J Psychiatry 163:1239–44.
Andrulonis PA, Glueck BC, Stroebel CF, Vogel NG. (1982). Borderline personality subcategories. J Nerv Ment
Dis 170:670–9.
Andrulonis PA, Glueck BC, Stroebel CF, Vogel NG, Shapiro AL, Aldridge DM. (1981). Organic brain dysfunction
and the borderline syndrome. Psychiatr Clin North Am 4:47–66.
Babinski LM, Hartsough CS, Lambert NM. (1999). Childhood conduct problems, hyperactivity-impulsivity,
and inattention as predictors of adult criminal activity. J Child Psychol Psychiatry 40:347–55.
Barkley RA, FischerM, Smallish L, Fletcher K. (2004). Young adult follow-up of hyperactive children:
antisocial activities and drug use. J Child Psychol Psychiatry 45:195–211.
Bergman LR, Magnusson D. (1986). Type A behavior: a longitudinal study from childhood to adulthood 20.
Psychosom Med 48:134–42.
Biederman J, Faraone SV, Keenan K, Benjamin J, Krifcher B, Moore C, et al. (1992). Further evidence for family-
genetic risk factors in attention deficit hyperactivity disorder. Patterns of comorbidity in probands
and relatives psychiatrically and pediatrically referred samples. Arch Gen Psychiatry 49: 728–38.
Biederman J, Faraone SV, Milberger S, Jetton JG, Chen L, Mick E, et al. (1996). Is childhood oppositional
defiant disorder a precursor to adolescent conduct disorder? Findings from a four-year follow-up
study of children with ADHD. J AmAcad Child Adolesc Psychiatry 35:1193–1204.
Biederman J, Mick E, Faraone SV, BurbackM. (2001). Patterns of remission and symptom decline in conduct
disorder: a four-year prospective study of an ADHD sample. J Am Acad Child Adolesc Psychiatry 40: 290–8.
Burt SA. (2009). Are there meaningful etiological differences within antisocial behavior? Results of a
meta-analysis. Clin Psychol Rev 29(2): 163–78.
Caspi A, Harrington H, Milne B, Amell JW, Theodore RF, Moffitt TE. (2003). Children’s behavioral styles at
age 3 are linked to their adult personality traits at age 26. J Pers 71:495–513.
Cleckley HM. (1951).The mask of sanity. Postgrad. Med 9:193–7.
Cloninger CR. (1987). A systematic method for clinical description and classification of personality variants.
A proposal. Arch Gen Psychiatry 44:573–88.
Cloninger CR. (2000). A practical way to diagnosis personality disorder: a proposal. J Pers Disord 14:99–108.
Cloninger CR, Svrakic DM, Przybeck TR. (1993). A psychobiological model of temperament and character.
Arch Gen Psychiatry 50:975–90.
Cooke DJ, Michie C. (2001). Refining the construct of psychopathy: towards a hierarchical model. Psychol
Assess 13:171–88.
Coolidge FL, Thede LL, Jang KL. (2004). Are personality disorders psychological manifestations of executive
function deficits? Bivariate heritability evidence from a twin study. Behav Genet 34:75–84.
Costa PT, Jr, McCrae RR. (1992). The Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory
(NEO-FFI) Professional Manual. Odessa, FL: Psychological Assessment Resources.
Downey KK, Stelson FW, Pomerleau OF, Giordani B. (1997). Adult attention deficit hyperactivity disorder:
psychological test profiles in a clinical population. J Nerv Ment Dis 185:32–8.
Dowson JH, McLean A, Bazanis E, Toone B, Young S, Robbins TW, et al. (2004).The specificity of clinical
characteristics in adults with attention-deficit/ hyperactivity disorder: a comparison with patients
with borderline personality disorder. Eur Psychiatry 19:72–8.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
44
CHAPTER 2
Faraone SV. (2005).The scientific foundation for understanding attention-deficit/hyperactivity disorder as a
valid psychiatric disorder. Eur Child Adolesc Psychiatry 14:1–10.
Farrington DP. (2000). Psychosocial predictors of adult antisocial personality and adult convictions. Behav
Sci Law 18:605–22.
FischerM, Barkley RA, Smallish L, Fletcher K. (2002). Young adult follow-up of hyperactive children:
self-reported psychiatric disorders, comorbidity, and the role of childhood conduct problems and
teen CD. J Abnorm Child Psychol 30:463–75.
Fossati A, Novella L, Donati D, DoniniM, Maffei C. (2002). History of childhood attention deficit/
hyperactivity disorder symptoms and borderline personality disorder: a controlled study. Compr
Psychiatry 43:369–77.
Frisell T, Lichtenstein P, L angstr¨om N. (2010). Violent crime runs in families: a total population study of
12.5 million individuals. Psychol Med 25:1–9.
Gittelman R, Mannuzza S, Shenker R, Bonagura N. (1985) Hyperactive boys almost grown up. Arch Gen
Psychiatry 42:937–47.
Goldman SJ, D’Angelo EJ, DeMaso DR. (1993). Psychopathology in the families of children and adolescents
with borderline personality disorder. Am J Psychiatry 150:1832–5.
Hare RD. (1980). A research scale for the assessment of psychopathy in criminal populations. Pers Individ Diff
1:111–19.
Hechtman L,Weiss, G. (1986). Controlled prospective fifteen year follow-up of hyperactives as adults:
non-medical drug and alcohol use and anti-social behavior. Can J Psychiatry 31(6):557–67.
Herrero ME, Hechtman L, Weiss G. (1994). Antisocial disorders in hyperactive subjects from childhood to
adulthood: predictive factors and characterization of subgroups. Am J Orthopsychiatry 64:510–21.
Hofvander B, Ossowski B, Lundstr¨om S, Anckars ater H. (2009). Continuity of aggressive antisocial behavior
from childhood to adulthood: the question of phenotype definition. Int J Law Psychiatry 32(4): 224–34.
Hooberman D, Stern TA. (1984). Treatment of attention deficit and borderline personality disorders with
psychostimulants: case report. J Clin Psychiatry 45:441–2.
Kim-Cohen J, Arseneault L, Caspi A, PoloThom asM, Taylor A, Moffitt TE. (2005). Validity of DSM-IV Conduct
Disorder in 41/2-5-year-old children: a longitudinal epidemiological study. Am J Psychiatry 162:1108–17.
Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. (2003). Prior juvenile diagnoses in
adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch
Gen Psychiatry 60:709–17.
Klinteberg B, Andersson T, Magnusson D, Stattin H. (1993). Hyperactive behavior in childhood as related to
subsequent alcohol problems and violent offending: a longitudinal study of male subjects. Pers Individ
Diff 15:381–8.
Kochanska G, Murray K, Coy KC. (1997). Inhibitory control as a contributor to conscience in childhood: from
toddler to early school age. Child Dev 68:263–77.
Lahey BB, Loeber R. (1997). ADHD and antisocial behavior. In: Stoff DM, Breiling J, Maser JD, eds. Handbook
of Antisocial Behavior. NewYork: Wiley& Sons: 243–54.
Lahey BB, Loeber R, Burke J, Rathouz PJ, McBurnett K. (2002).Waxing and waning in concert: dynamic
comorbidity of conduct disorder with other disruptive and emotional problems over 7 years among
clinic-referred boys. J Abnorm Psychol 111:556–67.
Lewinsohn PM, Rohde P, Seeley JR, Klein DN. (1997). Axis II psychopathology as a function of Axis I disorders
in childhood and adolescence. J AmAcad Child Adolesc Psychiatry 36:1752–9.
Lilienfeld S, Waldman ID. (1990).The relation between childhood attention-deficit hyperactivity disorder
and adult antisocial behavior re-examined: the problem of heterogeneity. Clin Psychol 10:699–725.
LivesleyWJ. (2001). Commentary on reconceptualizing personality disorder categories using trait
dimensions. J Pers 69:277–86.
Loeber R, Burke JD, Lahey BB. (2002).What are adolescent antecedents to antisocial personality disorder?
Crim Behav Ment Health 12:24–36.
Loeber R, Farrington DP, Stouthamer-LoeberM, Moffitt TE, Caspi A. (1998).The development of male
offending: key findings from the first decade of the Pittsburgh youth study. Stud Crime Prevent, 141–71

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
45
ADHD, PERSONALITY AND ITS DISORDERS
2
Loeber R, Green SM, Keenan K, Lahey BB. (1995).Which boys will fare worse? Early predictors of the onset of
conduct disorder in a six-year longitudinal study. J Am Acad Child Adolesc Psychiatry 34:499–509.
Loeber R, Green SM, Lahey BB, Frick PJ, McBurnett K. (2000). Findings on disruptive behavior disorders from
the first decade of the developmental trends study. Clin Child Fam Psychol Rev 3:37–60.
Lynam DR. (1996). Early identification of chronic offenders: who is the fledgling pyschopathy? Psychol Bull
120(2):209–34.
Lynn DE, Lubke G, Yang M, McCracken JT, McGough JJ, Ishii J, et al. (2005). Temperament and character
profiles and the dopamine D4 receptor gene in ADHD. Am J Psychiatry 162:906–13.
Mannuzza S, Klein RG, Abikoff H, Moulton JL, III. (2004). Significance of childhood conduct problems to
later development of conduct disorder among children with ADHD: a prospective follow-up study.
J AbnormChild Psychol 32:565–73.
Mannuzza S, Klein RG, Bessler A, Malloy P, LaPudalaM. (1993). Adult outcome of hyperactive boys.
Educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry 50:565–76.
Mannuzza S, Klein RG, Bessler A, Malloy P, LaPudalaM. (1998). Adult psychiatric status of hyperactive boys
grown up. Am J Psychiatry 155:493–8.
Mannuzza S, Klein RG, Bonagura N, Malloy P, Giampino TL, Addalli KA. (1991). Hyperactive boys almost
grown up. V. Replication of psychiatric status. Arch Gen Psychiatry 48:77–83.
McCutcheon AL. (1987). Latent Class Analyses. Newbury Park, CA: Sage.
McGough JJ, Barkley RA. (2004). Diagnostic controversies in adult attention deficit hyperactivity disorder.
Am J Psychiatry 161:1948–56.
Moffitt TE, Caspi A. (2001). Childhood predictors differentiate life-course persistent and adolescence
limited antisocial pathways among males and females. Dev Psychopathol 13:355–75.
Moffitt TE, Caspi A, Harrington H, Milne BJ. (2002). Males on the life-course-persistent and adolescence-
limited antisocial pathways: follow-up at age 26 years 12. Dev Psychopathol 14:179–207.
Nadder TS, Rutter M, Silberg JL, Maes HH, Eaves LJ. (2002). Genetic effects on the variation and covariation
of attention deficit-hyperactivity disorder (ADHD) and oppositional-defiant disorder/conduct disorder
(Odd/CD) symptomatologies across informant and occasion of measurement. Psychol Med 32:39–53.
Nigg JT. (2000). On inhibition/disinhibition in developmental psychopathology: views from cognitive and
personality psychology and a working inhibition taxonomy. Psychol Bull 126:220–46.
Nigg JT, Blaskey LG, Huang-Pollock CL, RappleyMD. (2002). Neuropsychological executive functions and
DSM-IV ADHD subtypes. J AmAcad Child Adolesc Psychiatry 4:59–66.
Nigg JT, Butler KM, Huang-Pollock CL, Henderson JM. (2002). Inhibitory processes inadults with persistent
childhood onset ADHD. J ConsultClin Psychol 70:153–7.
Nigg JT, John OP, Blaskey LG, Huang-Pollock CL, Willcutt EG, Hinshaw SP, et al.(2002). Big five dimensions
and ADHD symptoms: links between personality traitsand clinical symptoms. J Pers Soc Psychol 83:451–69.
Pacherie E. (1997). On being the product of one’s failed actions. In: Russel J, ed. ExecutiveDifficulties in Autism.
Oxford: Oxford University Press: 215–55.
Parker JDA, Majeski SA, Collin VT. (2004). ADHD symptoms and personality: relationshipswith the
five-factor model. Pers Individ Diff 36:977–87.
Perner J. (1998) The meta-intentional nature of executive functions and theory of mind. In:Carruthers P,
Boucher J, eds. Language andThought: Interdisciplinary Themes.Cambridge: Cambridge University Press:
270–83.
Pickles A, Angold A. (2003). Natural categories or fundamental dimensions: on carvingnature at the joints
and the rearticulation of psychopathology 3. Dev Psychopathol15:529–51.
Rassmussen P, Gillberg C. (2000). Natural outcome of ADHD with developmentalcoordination disorder at
age 22 years: A controlled, longitudinal, community-basedstudy. J Am Acad Child Adolescent Psychiatry
39(11):1424–31.
Rey JM, Morris-Yates A, SinghM, Andrews G, Stewart GW. (1995). Continuities betweenpsychiatric disorders
in adolescents and personality disorders in young adults. Am JPsychiatry 152:895–900.
Rhee SH,Willcutt EG, Hartman CA, Pennington BF, DeFries JC. (2008) Test of alternativehypotheses
explaining the comorbidity between Attention-Deficit/ HyperactivityDisorder and Conduct Disorder.
J AbnormChild Psychol 36:29–40.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
46
CHAPTER 2
Robbins, LN, Rutter M. (1990). Straight and Devious Pathways from Childhood toAdulthood. Cambridge: Cambridge
University Press.
Rothbart MK. (2004). Commentary: differentiated measures of temperament and multiplepathways to
childhood disorders. J Clin Child Adolesc Psychol 33:82–7.
Rothbart MK, Ahadi SA. (1994). Temperament and the development of personality. JAbnorm Psychol
103:55–66.
Sanislow CA, Grilo CM, McGlashan TH. (2000). Factor analysis of the DSM-III-R borderlinepersonality
disorder criteria in psychiatric inpatients. Am J Psychiatry 157:1629–33.
Satterfield JH, Hoppe CM, Schell, AM. (1982). A prospective study of delinquency in 110adolescent boys with
Attention Deficit Disorder and 88 normal adolescent boys. Am JPsychiatry 139:795–8.
Satterfield JH, Schell A. (1997). A prospective study of hyperactive boys with conductproblems and normal
boys: adolescent and adult criminality. J AmAcad Child AdolescPsychiatry 36:1726–35.
Schulz SC, Cornelius J, Schulz PM, Soloff PH. (1988).The amphetamine challenge test inpatients with
borderline disorder. Am J Psychiatry 145:809–14.
Seidman LJ, Doyle A, Fried R, Valera E, Crum K, Matthews L. (2004).Neuropsychological function in adults
with attention-deficit/hyperactivity disorder.Psychiatr Clin North Am 27:261–82.
Silberg J, Rutter M, Meyer J, Maes H, Hewitt J, Simonoff E, et al. (1996). Genetic andenvironmental influences
on the covariation between hyperactivity and conductdisturbance in juvenile twins. J Child Psychol
Psychiatry 37:803–16.
Soderstrom H, Nilsson T, Sjodin AK, Carlstedt A, Forsman A. (2005).The childhood-onset neuropsychiatric
background to adulthood psychopathic traits and personalitydisorders. Compr Psychiatry 46:111–16.
Svrakic DM, Whitehead C, Przybeck TR, Cloninger CR. (1993). Differential diagnosis ofpersonality disorders
by the seven-factor model of temperament and character. ArchGen Psychiatry 50:991–9.
Torgersen S, Kringlen E, Cramer V. (2001).The prevalence of personality disorders in acommunity sample.
Arch Gen Psychiatry 58:590–6.
Van Reekum R, Links PS. (1994). N of 1 study: methylphenidate in a patient with borderlinepersonality
disorder and attention deficit hyperactivity disorder. Can J Psychiatry39:186–7.
Verheul R. (2005). Clinical utility of dimensional models for personality pathology. J PersDisord 19: 283–302.
Weiss G, Hechtman L, Milroy T, Perlman T. (1985). Psychiatric status of hyperactives asadults: a controlled
prospective 15-year follow-up of 63 hyperactive children. JAmAcad Child Psychiatry 24: 211–20.
Widiger TA, Costa PT, Jr. (1994). Personality and personality disorders. J Abnorm Psychol103:78–91.
Widiger TA, Simonsen E. (2005). Alternative dimensional models of personality disorder:finding a common
ground. J Pers Disord 19:110–30.
World Health Organization (WHO). (1990). ICD-10 – International Statistical Classificationof Diseases and Related
Health Problems. Geneva: WHO.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
47
ADHD, PERSONALITY AND ITS DISORDERS
2

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Published as:
Van Dijk FE, Lappenschaar GAM, Verkes RJ, Kan CC & Buitelaar JK. (2011).
Life span attention deficit /hyperactivity disorder and borderline
personality disorder symptoms in female patients: a latent class approach.
Psychiatry research, 190 (2): 327-335.
Lifespan attention deficit/hyperactivity disorder and borderline personality
disorder symptoms in female patients: a latent class approach
3

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
50
CHAPTER 3
Abstract
Attention-deficit/hyperactivity disorder (ADHD) and borderline personality
disorder (BPD) are frequently comorbid. To contribute to a better understanding
of the associations regularly found between ADHD and BPD, on the one hand, and
the developmental pathways for these disorders, on the other hand, latent class
analyses (LCA) were undertaken to identify classes differing in profiles of childhood
symptoms of ADHD and adult symptoms of ADHD and BPD. Diagnostic interviews
with 103 female outpatients meeting the criteria for ADHD and/or BPD were used
to assess current DSM-IV symptoms; childhood symptoms of ADHD were assessed
in parent interviews. The latent classes were examined in relation to the DSM-IV
conceptualizations of ADHD and BPD. And relations between childhood and adult
classes were examined to hypothesize about developmental trajectories. LCA revealed
an optimal solution with four distinct symptom profiles: only ADHD symptoms;
BPD symptoms and only ADHD symptoms of hyperactivity; BPD symptoms and
ADHD symptoms of inattention and hyperactivity; BPD symptoms and ADHD
symptoms of inattention, hyperactivity and impulsivity. All patients with BPD
had some ADHD symptoms in both adulthood and childhood. Hyperactivity was
least discriminative of adult classes. Adult hyperactivity was not always preceded
by childhood hyperactivity; some cases of comorbid ADHD and BPD symptoms
were not preceded by significant childhood ADHD symptoms; and some cases of
predominantly BPD symptoms could be traced back to combined symptoms of
ADHD in childhood. The results underline the importance of taking ADHD
diagnoses into account with BPD. ADHD classification subtypes may not be
permanent over time, and different developmental pathways to adult ADHD and
BPD should therefore be investigated.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
51
LIFESPAN ADHD AND BPD SYMPTOMS IN WOMEN
3
Introduction
Attention deficit/hyperactivity disorder (ADHD), characterized by a persistent
pattern of inattentive and hyperactive-impulsive behavior and commonly known
as a developmental disorder starting in childhood, has been accepted as a valid and
reliable diagnosis in adulthood from both clinical and neurobiological perspectives
(Faraone, 2005). Up to 78% of adult patients with ADHD present with other DSM-IV
disorders (Biederman et al., 1993; Wilens et al., 2002; Kessler et al., 2006) while
relatively little attention has been paid to the associations of ADHD with adult
personality disorders. This is because disorders “usually first diagnosed in infancy,
childhood, or adolescence” — such as ADHD — are often not assessed in adulthood.
And conversely, Axis II of the DSM-IV can in principle be applied to determine the
presence of personality disorders — with the exception of the antisocial personality
disorder — at an early age, but this is typically not done until late adolescence.
There are nevertheless good reasons to assume that the personality traits or
individual differences in reaction patterns (i.e., temperament) that form the basis
for the development of adult traits are discernible during early child development
(Caspi et al., 2003).
Growing awareness of (1) the incidence of “childhood” disorders such as ADHD
in adulthood, (2) the presence of temperament differences already in infancy, and
(3) the manifestation of at least some Axis II personality disorders in adolescence
(Lewinsohn et al., 1997) thus calls for a cross-disciplinary re-examination of data
and definitions. In the present study, we therefore examined the relations between
adult ADHD and borderline personality disorder (BPD), which is the most common
personality disorder in clinical psychiatric settings. BPD is a complex and seriously
disabling mental disorder with an estimated incidence of 1% to 2% in the general
population (Torgersen et al., 2001). Almost 75% of the patients receiving therapy
for BPD is female (APA, 2000). A three-factor explanatory structure consisting of a
pervasive pattern of disturbed relations to other persons, affective or emotional
dysregulation, and behavioral impulsivity is commonly assumed (Sanislow et al.,
2000).
Viewed from a clinical perspective, patients with ADHD and BPD clearly share
symptoms of impulsivity. The expression of symptoms can vary, but a common
underlying trait such as impulsivity can create co-existence and/or obscure condi-
tion-specific symptoms. Specification of the relations between ADHD and BPD can
thus help refine diagnostic and therapeutic decision-making procedures but also
facilitate identification of childhood precursors to BPD. While the developmental
trajectories leading to BPD in adulthood are unclear, impulsivity appears to be one
of the earliest traits to emerge for those later diagnosed with BPD (Crowell et al.,
2009). We thus adopt a developmental model of psychopathology in which it is

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
52
CHAPTER 3
assumed that all psychiatric disorders are of a developmental nature and that the
manifestation of a particular disorder may change with the developmental stage
of the individual (Pennington, 2002).
Previous studies have indeed documented associations between symptoms of
ADHD in either childhood or adulthood and BPD (Davids & Gaspar, 2005; La Barbera
et al., 2009). In the early eighties, for example, it was shown that a significant
subgroup of with BPD had symptoms that were later referred to in the domain of
ADHD (Andrulonis et al., 1981; Andrulonis et al., 1982). A decade later, it was shown
that adolescents with disruptive disorders are more likely to have a personality
disorder from the dramatic/impulsive cluster, which includes BPD, at follow-up
when compared to adolescents with any emotional disorders. Specific associations
of ADHD with hyperactivity and BPD were also reported (Rey et al., 1995). More
recently, the results of a longitudinal study have again shown individuals
diagnosed with childhood ADHD to have an increased risk of personality disorders,
specifically the DSM-IV cluster B type of personality disorders in late adolescence
(Miller et al., 2008).
Research evaluating the presence of specific associations between retrospectively
assessed childhood ADHD symptoms and adult BPD in a controlled design has
revealed a significant relationship between the presence and severity of childhood
ADHD symptoms and adult BPD. At least 60% of the BPD subjects probably met the
criteria for ADHD in childhood (Fossati et al., 2002). In addition, research
investigating the prevalence of adult ADHD of the combined type in patients with
BPD showed a prevalence of 16.1% (Philipsen et al., 2008). Yet another very recent
study found 38.1% of BPD patients to be diagnosed with comorbid adult ADHD
(Ferrer et al., 2010). Such data can be taken to indicate the etiological heterogeneity
of both ADHD and BPD but does not indicate which characteristics are specifically
related and express the same underlying susceptibility or not.
In adults with BPD, the specificity of clinical ADHD characteristics has been
investigated and it has been shown that “impatience,” “aggressive behavior,”
“taking undue risks,” and “failure to take the likely results of actions into account”
are overlapping clinical features. Significant inter-group differences occurred for
“attention,” “organization,” and “persistence,” however (Dowson et al., 2004).
Furthermore, ADHD in male adults has been found to be associated with BPD
symptoms of impulsive aggression (Dowson & Blackwell, 2010). While these results
are in line with prior results, there is nevertheless still some indication that
symptoms referring to the inattention domain of ADHD should be considered in
the relationship between ADHD and BPD. ADHD subtype differences have not
been evaluated in prior studies of the associations between ADHD and BPD.
Moreover, in studies including patients with ADHD, adult personality disorders
have not been carefully controlled for.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
53
LIFESPAN ADHD AND BPD SYMPTOMS IN WOMEN
3
To contribute to a better understanding of the associations previously found
between ADHD and BPD, on the one hand, and the developmental pathways for
these disorders, on the other hand, analyses were undertaken to identify mutually
exclusive classes of subjects with homogeneous symptom profiles. Latent class
analyses (LCA) is a statistical technique used for exploratory and hypothesis-gener-
ating purposes (McCutcheon, 1987). Exploration of symptomatology using this
approach has the major advantage of not losing valuable information (i.e. in the
DSM-IV classification those who score just below the diagnostic threshold are
regarded as non-cases). To the best of our knowledge, there are currently no studies
performing LCA on ADHD and BPD symptoms.
The specific aims of the present research were as follows. To (1) classify female
patients with different profiles of childhood ADHD, adult ADHD, and symptoms
of BPD; (2) examine the latent classes in relation to the DSM-IV conceptualizations
of ADHD and BPD; and (3) explore the relations between the childhood and adult
classifications to identify possible developmental trajectories. This study also
provides the basis for its sequel, which examines the roles of temperament and
character in the differentiation of the classes of patients with similar ADHD / BPD
symptom profiles and the pathways from early temperament to future ADHD and/
or BPD (Van Dijk et al., 2011).
Methods
Participants and assessmentFemale patients were recruited from referrals to the outpatient ADHD program
or the outpatient BPD program of the Department of Psychiatry at the Radboud
University Nijmegen Medical Centre in the Netherlands. To be included in the
study, the patients thus had to meet the DSM-IV criteria for ADHD or BPD.
Patients were excluded in cases of clinically significant chronic medical conditions,
mental retardation, organic brain disorders or schizophrenia. Patients with other
comorbid psychiatric disorders were not excluded to ensure that the study sample
was as representative as possible of the population in clinical practice.
The patients underwent comprehensive clinical assessment, which included
psychiatric evaluation and both structured and semi-structured diagnostic interviews
conducted by trained psychologists or psychiatric trainees supervised by a senior
psychiatrist. The assessment was part of research projects approved by the local
Medical Ethical Committee. All patients signed an informed consent form prior to
participation.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
54
CHAPTER 3
The presence of current and childhood ADHD symptoms was assessed using a
Semi-Structured Interview for adult ADHD (Kooij, 2002). The authors have used
this semi-structured interview in previous studies of adult ADHD, and it has been
shown to be both reliable and valid (Kooij et al., 2001; Kooij et al., 2005; Kooij et al.,
2007). Collateral information on the occurrence and developmental history of
childhood symptoms was obtained from the parents or, when unavailable, an
older sibling. To gain further information on the exact DSM-IV criteria for current
and childhood ADHD, we used the Dutch translation of four ADHD DSM-IV Rating
Scales (i.e., patient, spouse, parent and investigator versions) (DuPaul et al., 1998).
To be fully diagnosed as having adult ADHD, the following criteria had to be met:
(1) the patient had to meet 6 of the 9 DSM-IV criteria for inattention and/or
hyperactivity/impulsivity in childhood and at least 5 of the 9 criteria in adulthood,
(2) a chronic course of symptoms of ADHD from childhood to adulthood had to be
the case, and (3) a moderate to severe level of impairment had to be attributed to
the symptoms of ADHD. A cut-off point of 5 out of the 9 criteria was set for the
adult diagnosis of ADHD as this is in keeping with the research literature and
epidemiological data using the same DSM-IV ADHD Rating Scales (Murphy &
Barkley, 1996; Biederman et al., 2000; Kooij et al., 2005).
The Structured Clinical Interview for DSM-IV Axis II Personality Disorders
(SCID-II) was used to determine the BPD classifications. (Weertman et al., 2000).
A classification was given only if no axis I disorder could account for the complaints
or dysfunctions. Other axis-I comorbidity was examined using the Structured
Clinical Interview for DSM-IV axis I (SCID-I) (Groenestijn et al., 1999).
The Global Assessment of Functioning Scale (GAF) from the DSM-IV was used
to assess the global social and professional functioning of the patient. In addition,
information on the social-economic status of the patient (i.e., living on income
from work or welfare) and the highest level of education completed by the patient
was collected.
Out of a total of 78 patients from the BPD program, 3 dropped out without
notification; 11 did not qualify as having BPD according to the DSM-IV; and 1 was
diagnosed with schizophrenia. Out of a total of 45 patients from the ADHD
program, 4 dropped out without notification and 1 said she could not complete the
assessment because it was too aggravating. The final sample thus consisted of 84%
of the original sample or a total of 103 female patients in the end: 40 from the
ADHD program and 63 from the BPD program. Of the ADHD patients, 6 (15%) were
diagnosed with a co-occurrent BPD. Of the BPD patients, 21 (33%) were diagnosed
with co-occurrent ADHD (i.e., ADHD in both childhood and adulthood). This
yielded a total of 27 patients with both ADHD and BPD. We were unable to attain
informant accounts of childhood symptoms of ADHD from 13 patients who all met
the criteria for BPD. Of these, 5 met the criteria for ADHD in adulthood but the

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
55
LIFESPAN ADHD AND BPD SYMPTOMS IN WOMEN
3
diagnosis could not be confirmed due to missing childhood data; the other 8 cases
did not meet the criteria for ADHD in adulthood, which led to the rejection of the
diagnosis of ADHD. This left a total of 37 patients with only BPD.
Statistical analysesLatent class analysis (LCA) (McCutcheon, 1987) was used to find the smallest
number of groups of individuals (i.e., classes) with similar patterns of symptoms
that could explain the associations observed among a set of variables. LCA describes
the probabilities of a set of observed categorical variables across groups of
individuals when the group membership of the individuals is unknown. Instead of
using predefined criteria for the presence or absence of a disorder, LCA uses ratings
of subjects on several symptoms. Calculations were made with Mplus version 4.1
(Muthén & Muthén, 2006). Mplus provides a number of decision parameters (22) of
which the Bayesian Information Criterium (BIC) and the Lo-Mendell-Rubin (LMR)
likelihood ratio tests are used in the exploratory phase of the analysis. The data are
analyzed with an increasing number of classes until there is no improvement in
any of the decision criteria (i.e., lower BIC values and more significant p-values
for the LMR indicate improvement over the previous model with one less class).
A small number of candidate models is thus identified for further analysis.
These models are investigated with the bootstrap likelihood ratio test (BLRT) to
determine the most likely number of classes. All analyses are run with a number
of different starting values to minimize the influence of local extremes. Given a
small sample size, the average number of individuals within a class should be
equal to at least the number of variables used in the model and the BLRT should be
superior to the LMR and BIC (Nylund et al., 2007).
The analyses were conducted in steps. To start with, the childhood and adult
symptoms were modeled separately to identify the different classes of patients (i.e.,
symptom profiles) for these different periods of life. For the childhood model, 18
ADHD variables were used, which meant that solutions containing more than 5
classes should be rejected for our sample size of 103. For the adult model, 18 ADHD
+ 9 BPD variables were used, which meant that solutions containing more than 4
classes should be rejected. Using SPSS version 14, the patient’s class membership
was then compared to the patient’s original group membership (i.e., DSM-IV
classification of ADHD only, BPD only or ADHD plus BPD). Regression in Mplus of
the adult classes on the childhood classes was finally undertaken to determine the
latent transition probabilities between adulthood and childhood.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
56
CHAPTER 3
Results
Adult classes of ADHD and BPD symptomsWe analyzed two through five latent classes of adult symptoms of ADHD and BPD.
The BIC values and corresponding number of free parameters were 3430 (53), 3233
(81), 3237 (109), and 3301 (137), respectively. The LMR values and corresponding
p-values were 1203 (< 0.001), 184 (0.220), 117 (0.167), and 75 (0.211), respectively. The
BIC suggested solutions with three or four classes as good candidates, whereas the
LMR values did not provide useful decision criteria. Given that the evaluation with
the BLRT values and corresponding p-values of 186 (< 0.001) and 118 (< 0.001)
showed the solution with four classes of symptoms to be significantly better than
the solutions with three or two classes, the solution with four classes was adopted.
Another reason to adopt the solution with four classes of symptoms was hypothesis
generation. The solution with three classes greatly overlapped the existing DSM-IV
classifications: one class reflected only ADHD symptomatology; one class reflected
symptoms of both ADHD and BPD; and one class reflected mainly symptoms of
BPD with some ADHD symptomatology. Working with these classes would not
have provided more specific or new information while it was nevertheless clear
that BPD symptoms did not appear alone (I.e., without ADHD symptomatology).
It was therefore decided to analyze the solution with four classes further. To be
more specific, we adopted the four profiles of adult symptoms of ADHD and BPD as
indicated in Figure 1.
In keeping with recent evidence that shows a three-factor structure for ADHD
(i.e., attention problems, hyperactivity problems, and impulsivity problems) to
better fit the adult symptom profile than the two-factor DSM-IV structure of
attention problems and hyperactivity/impulsivity problems (Span et al., 2002;
Barkley et al., 2007), the DSM-IV domain of hyperactivity/impulsivity was divided
into separate symptom clusters. In the end in our study, thus, Class 1 (29/103, 28%)
showed high probabilities for symptoms of inattention and hyperactivity,
intermediate probabilities for symptoms of impulsivity, and low probabilities for
BPD symptoms. Class 2 (20/103, 19%) showed low probabilities for symptoms of
inattention and impulsivity, intermediate probabilities for symptoms of hyper-
activity, and high probabilities for BPD symptoms. Class 3 (32/103, 31%) showed
high probabilities for both ADHD and BPD symptoms. Class 4 (22/103, 21%) showed
high probabilities for most but not all symptoms of inattention (i.e., scored low on
“fails to pay attention” and “difficulty listening”), showed intermediate to high
probabilities for symptoms of hyperactivity, high probabilities for BPD symptoms,
and low probabilities for symptoms of impulsivity.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
57
LIFESPAN ADHD AND BPD SYMPTOMS IN WOMEN
3
One class thus had symptoms of the combined type of ADHD, without
symptoms of BPD. The other three classes had high symptoms of BPD combined
with different symptoms of ADHD to different degrees. One class had symptoms of
the combined type of ADHD together with symptoms of BPD. Another had
symptoms of hyperactivity and inattention together with symptoms of BPD. And
the last class had only symptoms of hyperactivity together with symptoms of BPD.
Symptoms in the ADHD domain of hyperactivity showed the least variation across
the four classes and did not discriminate between the different classes, which is in
contrast to the symptoms of inattention and impulsivity (see Table 1). The data
thus show symptoms of ADHD to behave less consistently than symptoms of BPD
for this clinical population and symptoms of hyperactivity to have little value for
the discrimination of ADHD from BPD. Symptoms of BPD were also not found to
occur without at least some ADHD symptomatology; a completely comorbid
diagnosis of ADHD may not be the case but symptoms of ADHD in one or more
domains and to a greater or lesser extent were found to consistently co-occur with
symptoms of BPD.
Figure 1 Latent class probabilities for adult symptoms of ADHD and BPD in female patients with a diagnosis of ADHD, BPD, or both
0
10
20
30
40
50
60
70
80
90
100
Fail
s to
pay
att
enti
on t
o d
etai
ls
Dif
ficu
lty
sust
ain
ing
Dif
ficu
lty
care
full
y li
sten
ing
Dif
ficu
lty
foll
owin
g th
rou
gh o
f fi
nis
hin
g w
ork
Dif
ficu
lty
orga
niz
ing
task
s
Avo
ids
sust
ain
ing
men
tal
effo
rt
Lose
s th
ings
Easi
ly d
istr
acte
d
Forg
etfu
lnes
s
Fid
gest
wit
h h
and
s an
d f
eet
Oft
en l
eave
s se
at
Res
tles
snes
s m
otor
or
men
tal
acti
vity
Dif
ficu
lty
enga
gin
g in
lei
sure
Dri
ven
by
a m
otor
Talk
s ex
cess
ivel
y
Blu
rts
out
answ
ers
Dif
ficu
lty
awai
tin
g tu
rn
Inte
rru
pts
or
intr
ud
es
Avo
ids
aban
don
men
t
Un
stab
le a
nd
in
ten
se i
nte
rper
son
al r
elat
ion
ship
s
Ind
enti
ty d
istu
rban
ces
Pote
nti
ally
sel
f d
amag
ing
imp
uls
ivit
y
Self
mu
tila
tin
g or
su
icia
l be
hav
ior
Aff
ecti
ve i
nst
abil
ity
Ch
ron
ic f
eeli
ngs
of
emp
tin
ess
Dif
ficu
lty
con
trol
lin
g an
ger
Stre
ss-r
elat
ed p
aran
oia
or d
isso
ciat
ion
Perc
enta
ge
Class 1 (n=29) Class 2 (n=20) Class 3 (n=32) Class 4 (n=22)

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
58
CHAPTER 3
Childhood classes of ADHD symptomsWe analyzed two through five latent classes of childhood ADHD symptoms. The
BIC values and corresponding number of free parameters were 1860 (37), 1826 (56),
1851 (75), and 1903 (94), respectively. The LMR values and corresponding p-values
were 412 (0.002), 118 (0.005), 60 (0.129), and 33 (0.833), respectively. The BIC
suggested a three-class solution as the best model. Given that the LMR indicated
that this solution was significantly better than a two-class solution, which was
also supported by the BLRT value and corresponding p-value of 119 (0.000), the
solution with three classes was analyzed further.
Figure 2 shows the symptom profiles for the retrospective childhood measurement
of ADHD symptoms. Class 1(47/90, 52%) shows high probabilities for both inattention
Figure 2 Latent class probabilities for childhood history of symptoms of ADHD in adult female patients with a diagnosis of ADHD, BPD, or both
0
10
20
30
40
50
60
70
80
90
100
110
120
Fail
s to
pay
att
enti
on t
o d
etai
ls
Dif
ficu
lty
sust
ain
ing
Dif
ficu
lty
care
full
y li
sten
ing
Dif
ficu
lty
foll
owin
g th
rou
gh o
f fi
nis
hin
g w
ork
Dif
ficu
lty
orga
niz
ing
task
s
Avo
ids
sust
ain
ing
men
tal
effo
rt
Lose
s th
ings
Easi
ly d
istr
acte
d
Forg
etfu
lnes
s
Fid
gest
wit
h h
and
s an
d f
eet
Oft
en l
eave
s se
at
Res
tles
snes
s m
otor
or
men
tal
acti
vity
Dif
ficu
lty
enga
gin
g in
lei
sure
Dri
ven
by
a m
otor
Talk
s ex
cess
ivel
y
Blu
rts
out
answ
ers
Dif
ficu
lty
awai
tin
g tu
rn
Inte
rru
pts
or
intr
ud
es
Perc
enta
ge
Class 1 (n=47) Class 2 (n=23) Class 3 (n=20)

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
59
LIFESPAN ADHD AND BPD SYMPTOMS IN WOMEN
3
and hyperactivity/impulsivity symptoms in childhood; class 2 (23/90, 26%) shows
high probabilities for inattention and low probabilities for hyperactivity/impulsivity
symptoms in childhood and class 3 (20/90, 22%) shows almost no probabilities
for inattention symptoms and low probabilities for hyperactivity/impulsivity
symptoms in childhood. These results are consistent with DSM-IV field trials
among children, which confirm the validity of the DSM-IV combined ADHD
disorder and the Predominantly Inattentive ADHD disorder. Less support is
provided by the present data for the Predominantly Hyperactive-Impulsive type of
ADHD, which is included in the DSM-IV but occurs in almost only 4- to 6- year olds
(Lahey et al., 1994).
Adult Class membership compared to DSM-IV diagnosesThe relations between the adult class memberships and DSM-IV diagnoses for the
patients in our study are summarized in Figure 3. Almost all of the patients with
only a DSM-IV diagnosis of ADHD showed up in adult class 1 with high probabilities
for ADHD symptoms and low probabilities for BPD symptoms. The patients with
only a DSM-IV diagnosis of BPD were about equally distributed across classes 2, 3,
and 4 with high probabilities for BPD symptoms in all cases. Note that over
two-thirds of these patients with a diagnosis of only BPD were assigned to classes
3 and 4, which have high probabilities for ADHD symptoms. Most of the patients
with both a DSM-IV diagnosis of ADHD and BPD were assigned to classes 3 and 4
with high probabilities for all symptoms. At the level of symptoms, thus, symptoms
of ADHD were found to be less specific to the latent classes than symptoms of BPD
(see Figure 1); at the level of DSM-IV diagnoses, however, ADHD related more
specifically to the latent classes than BPD (see Figure 3).
Characteristics of the adult latent classes and DSM-IV Diagnostic groups The descriptive data for the DSM-IV diagnostic groups and the adult classes are
presented in Table 1. A more differentiated picture was found for the adult latent
classes than for the DSM-IV diagnostic groups. With regard to educational level, a
significant difference was found to occur between class 1 containing ADHD
symptoms and no BPD symptoms versus class 4 containing mostly symptoms of
inattention and symptoms of BPD. The patients in class 4 were less educated than
the patients in class 1. The patients in class 4 also had lower socio-economic levels
than the patients in the other three classes. The GAF score was highest for those
patients with only symptoms of ADHD (class 1).
Further inspection of the symptom profiles showed the patients with a DSM-IV
diagnosis of ADHD and the patients with a DSM-IV ADHD and comorbid BPD
diagnosis to not differ on the amount of hyperactivity and impulsivity symptoms.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
60
CHAPTER 3
The latent classes again showed a more differentiated picture (Table 1). Class 3 had
significantly more symptoms of hyperactivity and impulsivity than the other
three classes.
Latent transition probabilities between adult and childhood classes
In Figure 4, the latent transition probabilities between the adult and childhood
latent classes are presented together with the number of subjects. About 50% of the
patients in adult class 1— with high levels of inattention, intermediate levels of
hyperactivity and impulsivity, and very low levels of BPD symptoms — had a
childhood history of class 1 combined ADHD; the other 50% had a childhood
history of class 2 only inattention ADHD. Adult class 2 — with high levels of BPD
symptoms — had either a childhood history of class 1 combined ADHD or class 3
with low levels of ADHD symptoms. Most of the patients in adult class 3 — with
high probabilities for all ADHD and BPD symptoms — had a childhood history of
class 1 combined ADHD. Finally, adult class 4 — with BPD, inattention and hyper -
activity symptoms — showed an equal distribution across the three latent childhood
classes and thereby a diffuse pattern of transition from childhood to adulthood.
Figure 3 Adult latent class membership broken down by DSM-IV classifications
Class 1: combined ADHD symptoms. Class 2: BPD symptoms + hyperactivity. Class 3: BPD symptoms +
combined ADHD symptoms. Class 4: BPD symptoms + hyperactivity + inattention symptoms.
0
5
10
15
20
25
30
Class 1 Class 2 Class 3 Class 4
Nu
mb
er o
f p
atie
nts
DSM-IV ADHD
DSM-IV BPD
DSM-IV ADHD + BPD

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
61
LIFESPAN ADHD AND BPD SYMPTOMS IN WOMEN
3
Figure 4 Number of patients and latent transition probabilities in percentages for adult classes and childhood classes of female patients with attention deficit/hyperactivity disorder, borderline personality disorder, or both
Adult class 1: combined ADHD symptoms. Adult class 2: BPD symptoms + hyperactivity . Adult class 3:
BPD symptoms + combined ADHD symptoms. Adult class 4: BPD symptoms + hyperactivity + inattention
symptoms. Childhood class 1: combined ADHD symptoms. Childhood class 2: inattention symptoms.
Childhood class 3: mild hyperactivity + impulsive symptoms.
15 (52%)
14 (48%)
7 (47%)
8 (53%)
21 (66%)
7 (22%)
4 (28%)
5 (36%)
5 (36%)
4 (12%)
Adult class 1
Adult class 2
Adult class 3
Adult class 4
Child class 1
Child class 2
Child class 3

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
62
CHAPTER 3
Tab
le 1
Ch
arac
teri
stic
s of
fem
ale
pat
ien
ts c
lass
ified
acc
ord
ing
to D
SM-I
V a
nd
Lat
ent
Cla
ss A
nal
ysis
Ch
arac
teri
stic
DSM
-IV
LCA
AD
HD
(N
=34)
BPD
(N=3
7)C
om
bin
ed(N
=27)
1(N
=29)
2(N
=20)
3(N
=32)
4(N
=22)
N%
N%
N%
N%
N%
N%
N%
Edu
cati
on (<
BSc
)21
b,*,
c,*
6233
8923
8519
g,*
6617
8524
7521
96
Wel
fare
8 b,
**,c
,*24
2978
1556
7 e,
**,g
,**
2414
g,*
7015
g,**
4721
96
Mea
nSD
Mea
nSD
Mea
nSD
Mea
nSD
Mea
nSD
Mea
nSD
Mea
nSD
Age
(yea
rs)
35 b*
*,*
1231
732
935
1232
732
933
9
GA
F sc
ore
65 b,
**,c
,**
855
1059
765
e,**
,f,*
*,g,
**7
5611
599
559
IA7.
7 b,
**,c
,**
1.3
3.0
c,**
2.4
6.3
2.1
7.7
e,**
,f,*
*,g,
**1.
41.
3 f,
**,g
,**
1.4
6.4
2.1
5.4
1.7
H3.
3 b,
*1.
32.
6 c,
**1.
33.
60.
93.
0 e,
**,f
,**
1.2
2.1
f,**
1.0
4.1
g,**
0.7
2.5
1.1
I2.
2 b,
**1.
50.
8 c,
**1.
22.
41.
61.
9 e,
**,f
,**,
g,**
1.4
0.6
f,**
0.8
3.1 g
,**
1.1
0.2
0.4
Tota
l IA
+H/I
13.2
b,**
2.9
6.4
c,**
4.0
12.3
3.1
12.6
e,**
,g,*
*2.
74.
0 f,
**,g
,**
2.7
13.6
g,**
2.7
8.1
2.3
BPD
*1.
0 b,
**,c
**1.
26.
51.
46.
01.
00.
8 e,
**,f
,**,
g,**
1.1
6.5
1.3
5.6
1.7
6.3
1.5
0In
dep
end
ent
sam
ple
T-t
est
for
mu
ltip
le c
omp
aris
on o
f age
, GA
F, I
A, H
, I, t
otal
IA
+ H
/I a
nd
BPD
ou
tcom
e b
etw
een
DSM
-IV
su
btyp
es a
nd
bet
wee
n L
CA
cla
sses
; Fis
her
’s
exac
t te
st f
or m
ult
iple
com
par
ison
of
edu
cati
on a
nd
wel
fare
ou
tcom
e b
etw
een
DSM
-IV
su
btyp
es a
nd
bet
wee
n L
CA
cla
sses
. Abb
revi
atio
ns:
AD
HD
= a
tten
tion
-defi
cit/
hyp
erac
tivi
ty d
isor
der
; BPD
= b
ord
erli
ne
per
son
alit
y d
isor
der
; com
bin
ed =
bot
h A
DH
D a
nd
BPD
; GA
F =
Glo
bal
Ass
essm
ent o
f Fu
nct
ion
ing;
IA
= in
atte
nti
on s
ymp
tom
s;
H =
hyp
erac
tivi
ty s
ymp
tom
s; I
= i
mp
uls
ivit
y sy
mp
tom
s; B
PD*
= BP
D s
ympt
oms.
a Vs.
DSM
-IV
AD
HD
sub
type
s. b
Vs.
DSM
-IV
BPD
su
btyp
es. c V
s. D
SM-I
V c
ombi
ned
su
btyp
es.
d V
s. L
CA
cla
ss 1
. e V
s. L
CA
cla
ss 2
. f V
s. L
CA
cla
ss 3
. g V
s. L
CA
cla
ss 4
. * p
_0.0
5. *
* p≤
0.01
.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
63
LIFESPAN ADHD AND BPD SYMPTOMS IN WOMEN
3
Discussion
For both adult and childhood symptoms, latent classes representing qualitatively
different profiles were identified rather than simply differences in the clinical
severity of the symptoms as commonly found in latent class analyses of ADHD
symptoms with or without added comorbidities (Acosta et al., 2008).
The solution with four latent classes tells us more about the construct of BPD
than the construct of ADHD. Patients with a primary diagnosis of ADHD and no
BPD were all allocated to latent class 1 with indeed no symptoms of BPD. In
contrast, patients with a diagnosis of BPD were distributed across the three other
classes and all had some ADHD symptomatology. This heterogeneous picture is in
line with the results of other studies of BPD and its diagnostic comorbidity
(Zimmerman & Mattia, 1999; Shea et al., 2004) but also provides new insights
regarding the coexistence of ADHD and BPD. In clinical practice, ADHD may
frequently be missed in patients with a diagnosis of BPD and thus lead to
insufficient and possibly inadequate treatment.
ADHD symptoms of hyperactivity were found to be high for all of the latent
classes of patients, which indicate that hyperactivity has a poor diagnostic value
for the differentiation of ADHD and BPD. Hyperactivity appears to be characteristic
of not only most ADHD patients but also many patients with BPD. This may be due
to the indistinct, unspecific, and broad formulation of the DSM-IV criteria for
hyperactivity (e.g. “restless motor or mental activity” and “difficulty in engaging
leisure”), which boils down to the measurement of overall restlessness — possibly
confounded by stress or anxiety. Earlier results suggest that individuals with BPD
also exhibit inhibitory dysfunction (Swirsky-Sacchetti et al, 1993; Bazanis et al
2002; Possner et al, 2002; Nigg, 2005). To date, however, only one comparative study
has shown symptoms of BPD to still correlate with response inhibition after
control for comorbidity with ADHD (Nigg, 2005). In another comparative study, it
was concluded that, in contrast to ADHD, BPD is not characterized by a specific
attentional deficit (Lampe et al, 2007). In the present study, however, we found a
class of patients with BPD and also inattention problems. Further research is thus
needed to clarify the coexistence of attention and inhibition problems with BPD.
The three childhood classes of ADHD symptoms corresponded well with
known clinical findings and reflected the combined inattentive and hyperactive
impulsive type of ADHD, the strictly inattentive type, and the hyperactive
impulsive type (Lahey et al., 1994). Assuming that the four adult classes provided
information beyond our knowledge of the DSM-IV classifications, it is surprising
that the four classes all showed relatively high probabilities for symptoms of
hyperactivity. This suggests that the existence of adult hyperactivity does not
automatically imply the existence of childhood hyperactivity, which raises

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
64
CHAPTER 3
questions about the validity of the hyperactivity construct and the stability of the
construct of ADHD over time.
There were three adult classes that had high probabilities for symptoms of
ADHD but contained patients with only very few symptoms of hyperactivity and
impulsivity in childhood. In other words, having almost no symptoms of ADHD in
childhood does not automatically imply a low probability of such symptoms in
adulthood. An explanation for this may lie in the age of onset adopted for ADHD
in the present study, namely 12 years. There are recent indications that late onset
adult ADHD is valid and that the age of onset recommended by the DSM-IV, namely
7 years, might be too stringent. (Faraone et al., 2006a; Faraone et al., 2006b).
Furthermore, an adult class of patients with almost only BPD symptoms but a
history of combined ADHD symptoms was identified in the present study, which
suggests that ADHD can remit later in life (Faraone et al., 2006a).
Examination of the latent transition possibilities suggests several developmental
pathways. One possible pathway leads from combined inattention and hyperactive/
impulsive symptoms or mainly inattention symptoms in childhood to an adult
profile containing only symptoms of ADHD and not BPD. Another possible pathway
leads from a childhood profile with at least low levels of hyperactive/impulsive
symptoms but no inattention problems to an adult profile with symptoms of BPD.
Hyperactive/impulsive symptoms could thus play a mediating role in the
development of BPD along this pathway. The actual causal relations between
ADHD and BPD are still unclear, however. We should also bear in mind that (1) LCA
is mainly used for exploratory and hypothesis-generating purposes and (2) a
retrospective design, which is susceptible to recall bias, was used. To diminish the
possible effects of poor memory, we triangulated the self-report information with
regard to current and past symptomatology using other data sources (i.e., parents,
older siblings, spouses) before making a diagnosis. The present results are
nevertheless in line with the results of many longitudinal prospective studies of
the criteria for ADHD and related definitions.
There are some other possible limitations on the present study. The study
group consisted of patients at an academic medical centre and may therefore be
sensitive to referral bias. The results certainly cannot be generalized to nonreferred
samples. Furthermore, the number of subjects within the individual classes met
the minimal criteria but the sample size was still small for LCA and the sample
only included females. Given that it is mostly women who receive therapy for BPD
while the sex ratio for adult patients with ADHD is more equally divided, the
results of this study are probably more representative for the population with BPD.
The question of whether the results hold for males thus remains to be answered.
The results must be replicated and extended to larger independent samples.
Nonetheless, the use of a well-described and diagnosed sample showed — in

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
65
LIFESPAN ADHD AND BPD SYMPTOMS IN WOMEN
3
keeping with the results of other studies (Lahey et al., 2005) — that the DSM-IV
subtypes of ADHD cannot be viewed as discrete, nominal categories that are
relatively permanent over time.
In closing, we would like to mention some clinical implications of the present
results and directions for future research. A first implication is that in cases of a
diagnosis of BPD, ADHD should also always be considered. This is because BPD has
been found to frequently occur with symptoms of ADHD; over one third of patients
diagnosed with BPD also receive a co-occurring ADHD diagnosis. It is plausible
that unrecognized ADHD can worsen the course of BPD and treatment outcome.
Conversely, the detection of BPD in cases of ADHD can also be of importance for
the selection and outcome of treatment. A second implication is that ADHD should
not be differentiated from BPD on the basis of symptoms of hyperactivity.
Hyperactivity has little discriminative value for these disorders. The present
results thus challenge us to further unravel the relations between ADHD and BPD,
identify their unique and shared characteristics, and illuminate the possible
pathways to adult ADHD — either with or without comorbid BPD. The latent classes
identified in this research should be validated with the addition of external
variables. The next step in our research is therefore to analyze the associations of
a number of factors to the combination of ADHD and BPD: temperament and
character features (Van Dijk et al., 2011), neurocognitive measures, and genetic
data. In light of the present results, our main hypothesis for the future will be that
impulsivity continues to be a shared feature of ADHD and BPD and to possibly play
a mediating role in the development of adult BPD not only at the level of symptoms
but also at the level of personality traits and neurocognitive outcome. The
specificity of inattention symptoms in adult ADHD and BPD remains to be seen,
however.
AcknowledgementsRose Collard, Marjan Knippenberg, and Marleen Bastiaanse, are gratefully
acknowledged for their expert research assistance. Pieter van den Broek is
gratefully acknowledged for his close collaboration on the data collection.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
66
CHAPTER 3
References
Acosta, M.T., Castellanos, F.X., Bolton, K.L., Balog, J.Z., Eagen, P, Nee L.,2008. Latent class subtyping of atten-
tion-deficit/hyperactivity disorder and comorbid conditions. Journal of the American Academy of
Child and Adolescent Psychiatry 47, 797-807.
American Psychiatric Association, 1994. Diagnostic and Statistical Manual of Mental Disorders, fourth ed.
APA, Washington, D.C.
Andrulonis, P.A., Glueck, B.C., Stroebel, C.F., Vogel, N.G., Shapiro, A.L., Aldridge, D.M., 1981. Organic brain
dysfunction and the borderline syndrome. Psychiatric Clinics of North America 4, 47-66.
Andrulonis P.A., Glueck B.C., Stroebel C.F., Vogel N.G., 1982. Borderline personality subcategories. Journal
of Nervous and Mental Disease 170, 670-9.
Barkley, R.A., Murphy, K.R., Fischer, M., 2007. The Science of ADHD in Adults: Clinic- Referred Adults and
children Grown Up. Guilford, New York.
Bazanis, E., Rogers, R. D., Dowson, J. H., Taylor, P., Meux, C., Staley, C., Nevinson- Andrews, D., Taylor, C.,
Robbins, T. W., Sahakian, B. J., 2002. Neurocognitive deficits in decision-making and planning of
patients with DSM-III-R borderline personality disorder. Psychological Medicine 32, 1395–1405.
Biederman, J., Faraone, S.V., Spencer, T., Wilens, T., Norman, D., Lapey, K.A., 1993. Patterns of psychiatric
comorbidity, cognition and psychosocial functioning in adults with Attention Deficit Hyperactivity
Disorder. American Journal of Psychiatry 150, 1792-8.
Biederman, J., Mick, E., Faraone, S.V., 2000. Age-dependent decline of symptoms of attention deficit
hyperactivity disorder: impact of remission definition and symptom type. American Journal of
Psychiatry 157, 816-8.
Caspi A, Harrington H, Milne B, Amell JW, Theodore RF, Moffitt TE., 2003. Children’s behavioral styles at
age 3 are linked to their adult personality traits at age 26. Journal of Personality 71, 495–513.
Crowell, S.E., Beauchaine, T.P., Linehan, M.M., 2009. A biosocial development model of borderline
personality: Elaborating and extending Linehan’s theory. Psychological Bulletin 135,495-510.
Davids, E., Gaspar M., 2005. Attention deficit hyperactivity disorder and borderline personality disorder.
Progress in Neuro-Psychopharmacology and Biological Psychiatry 29, 865-977.
Dowson, J.H., McLean, A., Bazanis, E., Toone, B., Young, S., Robbins, T.W., 2004. The specificity of clinical
characteristics in adults with attention-deficit/hyperactivity disorder: a comparison with patients
with borderline personality disorder. European Psychiatry 19, 72-8.
DuPaul, G.J., Power TJ, Anastopoulos, A.D., Reid, R., 1998. ADHD Rating Scale-IV. Checklists, Norms and
Clinical Interpretation. The Guilford press, New York.
Faraone, S.V., 2005. The scientific foundation for understanding attention- deficit/hyperactivity disorder as
a valid psychiatric disorder. European Child & Adolescent Psychiatry 14, 1-10.
Faraone, S.V., Biederman, J., Spencer, T., Mick, E., Murray, K., Petty, C., 2006a. Diagnosing adult attention
deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid? American Journal of
Psychiatry 163, 1720-9.
Faraone, S.V., Biederman, J., Doyle, A., Murray, K., Petty, C., Adamson, J.J., 2006b. Neuropsychological studies
of late onset and subthreshold diagnoses of adult attention-deficit/hyperactivity disorder. Biological
Psychiatry 15,1081-7.
Ferrer, M., Andion, O., Matali, J., Valero, S., Navarro, J.A., Ramos-Quiroga, J.A., Torrubia, R., Casas, M., 2010.
Comorbid attention-deficit/hyperactivity disorder in borderline patients defines an impulsive
subtype of borderline personality disorder. Journal of Personality Disorders 24, 812-822.
Fossati, A., Novella, L., Donati, D., Donini, M., Maffei, C., 2002. History of childhood attention deficit/
hyperactivity disorder symptoms and borderline personality disorder: a controlled study. Comprehensive
Psychiatry 43, 369-77.
Groenestijn, M.A.C., Akkerhuis, G.W., Kupka, R.W., Schneider, N., Nolen, W.A., 1999. Structured Clinical
Interview for DSM-IV Axis I Disorders. Swets & Zeitlinger BV, Lisse, The Netherlands.
Kessler, R.C., Adler, L., Barkley, R., Biederman, J., Conners, C.K., Demler, O., 2006. The prevalence and
correlates of adult ADHD in the United States: results from the National Comorbidity Survey
Replication. American Journal of Psychiatry 163, 716- 23.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
67
LIFESPAN ADHD AND BPD SYMPTOMS IN WOMEN
3
Kooij, J.J., Aeckerlin, L.P., Buitelaar, J.K., 2001. Functioning, comorbidity and treatment of 141 adults with
attention deficit hyperactivity disorder (ADHD) at a psychiatric outpatient department. Nederlands
Tijdschrift voor Geneeskunde 145, 1498-501.
Kooij, J.J.S., 2002. ADHD bij volwassenen. Inleiding in diagnostiek en behandeling [ADHD in adults.
Introduction in diagnostics and treatment]. Swets & Zeitlinger, Lisse.
Kooij, J.J., Buitelaar, J.K., van den Oord, E.J., Furer, J.W., Rijnders, C.A., Hodiamont, P.P., 2005. Internal and
external validity of attention-deficit hyperactivity disorder in a population-based sample of adults.
Psychological Medicine 35, 817-27.
Kooij, J.S., Boonstra, A.M., Vermeulen, S.H., Heister, A.G., Burger, H., Buitelaar, J.K., 2007. Response to meth-
ylphenidate in adults with ADHD is associated with a polymorphism
in SLC6A3 (DAT1). American Journal of Medical Genetics
Part B: Neuropsychiatric Genetics 147B, 201–208.
La Barbera, D., Sideli, L., Mistretta, C., Sartorio, C., Grillo, G., 2009. Attention deficit/hyperactivity disorder
and borderline personality disorder: Differential diagnosis and comorbidity from childhood to
adulthood. Italian Journal of Psychopathology 15, 250-268.
Lahey, B.B., Applegate, B., McBurnett, K., Biederman, J., Greenhill, L., Hynd, G.W., 1994. DSM-IV field trials
for attention deficit hyperactivity disorder in children and adolescents. American Journal of
Psychiatry 151, 1673-85.
Lahey, B.B., Pelham, W.E., Loney, J., Lee, S.S., Willcutt, E., 2005. Instability of the DSM-IV Subtypes of ADHD
from preschool through elementary school. Archives of General Psychiatry 62, 896-902.
Lampe, K., Konrad K., Kroener, S., Fast, K., Kunert, H.J., Herpertz, S.C., 2007. Neuropsychological and
behavioural disinhibition in adult ADHD compared to borderline personality disorder. Psychological
Medicine 37, 1717-1729.
Lewinsohn PM, Rohde P, Seeley JR, Klein DN., 1997. Axis II psychopathology as a function of Axis I disorders
in childhood and adolescence. Journal of the American Academy of Child & Adolescent Psychiatry 36,
1752–9.
McCutcheon, A.L., 1987. Latent Class Analysis. Sage, Newbury Park, CA.
Miller, C.J., Flory, J.D., Miller, S.R., Harty, S.C., Newcorn, J.H., Halperin, J.M., 2008. Childhood attention-defi-
cit/hyperactivity disorder and the emergence of personality disorders in adolescence: A prospective
follow-up study. Journal of Clinical Psychiatry 69, 1477-1484.
Murphy, K., Barkley, R.A., 1996. Prevalence of DSM-IV symptoms of ADHD in adult licensed drivers:
Implications for clinical diagnosis. Journal of Attention Disorders 1, 147-61.
Muthén, L,K., Muthén, B.O., 2006. Mplus user’s guide. Statistical analysis with latent variables (4th ed.;
version 4.1). Muthén & Muthén, Los Angeles.
Nigg, J.T., Silk, K.R., Stavro G., Miller, T., 2005. Disinhibition and borderline personality disorder.
Developmental Psychopathology 17, 1129-1149.
Nylund, K,L., Asparouhov, T., Muthén, B., 2007. Deciding on the number of classes in latent class analysis
and growth mixture modeling: a Monte Carlo simulation study. Structural Equation Modeling: A
Multidisciplinary Journal 14, 535-69.
Pennington, B.F. ,2002. The development of psychopathology: Nature and nurture. New York: Guilford
Press.
Philipsen, A., Limberger, M.F., Lieb, K., Feige, B., Kleindienst, N., Ebner-Priemer, U., 2008. Attention-deficit
hyperactivity disorder as a potentially aggravating factor in borderline personality disorder. British
Journal of Psychiatry 192, 118-23.
Posner, M. I., Rothbart, M. K., Vizueta, N., Levy, K. N., Evans, D. E., Thomas, K. M., Clarkin, J. F., 2002.
Attentional mechanisms of borderline personality disorder. Proceedings of the National Academy of
Sciences of the United States of America 99, 16366–16370.
Rey, J.M., Morris-Yates, A., Singh, M., Andrews, G., Stewart, G.W., 1995. Continuities between psychiatric
disorders in adolescents and personality disorders in young adults. American Journal of Psychiatry
152, 895-900.
Sanislow CA, Grilo CM, McGlashan TH., 2000. Factor analysis of the DSM-III-R borderline personality
disorder criteria in psychiatric inpatients. American Journal of Psychiatry 157, 1629–33.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
68
CHAPTER 3
Span, S.A., Earleywine, M., Strybel, T.Z., 2002. Confirming the factor structure of attention deficit
hyperactivity disorder symptoms in adult, nonclinical samples. Journal of Psychopathology and
Behavioral Assessment 24, 129-36.
Shea, M.T., Stout, R.L., Yen, S., Pagano, M.E., Skodol, A.E., Morey, L.C., 2004. Associations in the course of
personality disorders and Axis I disorders over time. Journal of Abnormal Psychology 113, 499-508.
Swirsky-Sacchetti, T., Gorton, G., Samuel, S., Sobel, R., Genetta-Wadley, A., Burleigh, B.,1993. Neuropsycho-
logical function in borderline personality disorder. Journal of Clinical Psychology 49, 385–396.
Torgersen S, Kringlen E, Cramer V., 2001.The prevalence of personality disorders in a community sample.
Archives of General Psychiatry 58, 590–6.
Van Dijk, F.E., Lappenschaar, M., Kan, C.C., Verkes, R.J., Buitelaar, J.K., 2011. Symptomatic overlap between
attention-deficit/hyperactivity disorder and borderline disorder in women: the role of temperament
and character traits. Comprehensive Psychiatry, DOI: 10.1016/j.comppsych.2011.02.007
Weertman, A., Arntz, A., Kerkhofs, M.L.M., 2000. Structured Clinical Interview for DSM-IV Axis II
Personality Disorders. Swets & Zeitlinger BV, Lisse, the Netherlands.
Wilens, T.E., Biederman, J., Spencer, T.J., 2002. Attention deficit/hyperactivity disorder across the lifespan.
Annual Review of Medicine 53, 113-31.
Zimmerman, M., Mattia, J.I., 1999. Axis I diagnostic comorbidity and borderline personality disorder.
Comprehensive Psychiatry 40, 245-52.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
69
LIFESPAN ADHD AND BPD SYMPTOMS IN WOMEN
3

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Published as:
Van Dijk FE, Lappenschaar GAM, Verkes RJ, Kan CC & Buitelaar JK. (2012)
Symptomatic overlap between attention deficit/hyperactivity disorder
and borderline personality disorder: The role of temperament and character traits.
Comprehensive psychiatry, 53(1): 39-48.
Symptomatic overlap between attention-deficit/hyperactivity disorder
and borderline personality disorder in women: the role of temperament
and character traits
4

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
72
CHAPTER 4
Abstract
Objective: There is substantial symptomatic overlap between Attention-Deficit/
Hyperactivity Disorder (ADHD) and borderline personality disorder (BPD) in adults,
but the nature of the relationship between these disorders needs further
clarification. The role of temperament and character traits in the differentiation
of classes of patients with similar ADHD and BPD symptom profiles was examined
and possible pathways between early temperament and future ADHD and/or BPD
were hypothesized.
Method: Structured diagnostic interviews were conducted in 103 female patients
to assess current DSM-IV symptoms of ADHD and BPD, and parent interviews were
used to assess ADHD symptoms in childhood. Classes of subjects with homogeneous
symptom profiles were identified using latent class analysis (LCA). Temperament
and character traits were assessed using Cloninger’s Temperament and Character
Inventory; scores were then compared across the latent classes.
Results: LCA revealed four mutually exclusive classes of patients: one with only
ADHD symptoms; one with BPD symptoms and ADHD symptoms of hyperactivity;
one with BPD symptoms and ADHD symptoms of inattention, hyperactivity, and
impulsivity; and one with BPD symptoms and ADHD symptoms of inattention and
hyperactivity. High Novelty Seeking was found in all classes except for the class
with symptoms of BPD and only the hyperactivity aspect of ADHD. The highest
Novelty Seeking temperament scores were found in that class of patients with
both symptoms of BPD and symptoms in all areas of ADHD. High Harm Avoidance,
low Cooperativeness, and low Self-Directedness were specifically related to classes
containing BPD symptoms.
Conclusions: Classes of ADHD and BPD symptoms are associated with specific
temperament and character configurations. Novelty Seeking was associated with
the inattention symptoms of ADHD. An outspoken Novelty Seeking temperament
suggests a vulnerability for the development of ADHD and co-occurring BPD.
Contrary to patients with combined ADHD and BPD symptoms, patients with only
symptoms of ADHD showed normal character development and thus an absence of
a personality disorder. Assessment of temperament and character traits can
improve our understanding of the complex relationship between ADHD and BPD.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
73
TEMPERAMENT AND CHARACTER IN FEMALE ADHD AND BPD
4
Introduction
Research has shown significant co-occurrence of DSM-IV defined attention-deficit/
hyperactivity disorder (ADHD) and borderline personality disorder (BPD) in adults
[1-6]. In our previous latent class analyses (LCA) [7], groups of women with differing
profiles of childhood symptoms of ADHD, adult symptoms of ADHD, and adult
symptoms of BPD showed BPD to be accompanied by adult symptoms of ADHD but
the hyperactivity symptoms of ADHD to be least discriminative. Adult hyperactivity
was not always preceded by childhood hyperactivity; some cases of comorbid
ADHD and BPD symptoms were not preceded by significant childhood ADHD
symptoms; and some cases of predominantly BPD symptoms could be traced back
to combined symptoms of ADHD in childhood [8]. These results prompted us to
further our work on the relationships between ADHD and BPD but from a more
developmental perspective.
To gain greater insight into the different possible pathways leading to ADHD
with or without BPD, the roles of temperament and personality traits in the
co-occurrence of ADHD and BPD were examined. Associations with temperament
and personality may provide clues to the structure and outcome of ADHD and
thereby etiological theories [9 -12]. ADHD is characterized by three domains of
behavioral problems (i.e., inattention, hyperactivity, and impulsivity) and, for this
reason, ADHD particularly lends itself to an examination of the roles of temperament
and personality in its occurrence. Although the inattention, hyperactivity and
impulsivity symptom domains cluster together to constitute ADHD as a syndrome,
the different domains of symptoms may nevertheless have partially distinct
etiological determinants. The pathways for the different domains of symptoms for
ADHD may, moreover, overlap with the BPD problems that frequently accompany
ADHD. Temperament and personality may thus shape the course of ADHD and
help clarify the nature of the relations between adult ADHD and BPD.
Temperament and character dimensionsIn the present research, we draw upon Cloninger’s theory of personality because it
addresses the genetic and neurobiological bases of personality in interaction with
the environment and learning [13]. In this theory, it is assumed that personality
can be typified in terms of four temperament dimensions and three character
dimensions.
The temperament dimensions of personality manifest themselves early in life,
are assumed to be independently heritable, reflect individual differences in basic
emotional drives, and are defined in terms of differing responses to novelty, harm,
reward, and tasks requiring persistence [14]. The temperament dimensions of
personality include Novelty Seeking (i.e., impulsive and irritable versus rigid and

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
74
CHAPTER 4
stoical), Harm Avoidance (i.e., pessimistic and anxious versus optimistic and
risk-taking), Reward Dependence (i.e., sociable and warm versus aloof and cold),
and Persistence (i.e., persevering and ambitious versus easily discouraged and
indolent).
The character dimensions of personality are hypothesized to mature in adulthood
via conceptual or insight-based learning and to reflect individual differences in
those higher cognitive processes that define a person’s style of mental self-government.
The character dimensions of personality include Self-Directedness (i.e., responsible
and resourceful versus blaming and inept), Cooperativeness (i.e., helpful and
principled versus hostile and opportunistic), and Self-Transcendence (i.e., intuitive
and insightful versus concrete and conventional) [15,16].
The seven dimensions of personality are measured using the Temperament
and Character Inventory (TCI), which is a self-rating instrument [16]. Each of the
seven temperament and character traits is multifaceted, consisting of several facets
or lower order components. Twenty five facets altogether (12 facets of temperament
and 13 facets of character) make up the TCI. From a clinical perspective, the
presence of a personality disorder is indicated by character immaturity (i.e., low
Self-Directedness and/or Cooperativeness scores); the type of personality disorder
is indicated by the configuration of temperament scores [17,18]. Studies have shown
the character dimensions of Self-Directedness and Cooperativeness to discriminate
between patients with or without a diagnosed personality disorder and different
patterns of temperament scores to correlate significantly with different personality
disorders [14,19,20].
Previous research on temperament and character in ADHD and BPD Previous studies report significant correlations between BPD and high Novelty
Seeking and Harm Avoidance, on the one hand, and low Self-Directedness and low
Cooperativeness, on the other hand [19-21]. One study extended this research to
take gender and comorbidity into account [22]. Women with BPD showed high
levels of Harm Avoidance but not Novelty Seeking with very low levels of Self
Directedness.
Few studies have investigated the TCI profiles of adults with ADHD, but the
available results show a similar set of associations as for BPD. Adult ADHD subjects
score significantly higher than normal subjects on the temperament dimensions
of Novelty Seeking and Harm Avoidance [23-25]. Also compared to the general
population, much lower scores on the character dimensions of Self-Directedness
and Cooperativeness are reported. It is therefore suggested that these findings are
consistent with the notion that early problems form obstacles for later character
maturation and may predict a high rate of clinically significant personality
disorder. The study by Anckarsater et al is of particular interest within this context

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
75
TEMPERAMENT AND CHARACTER IN FEMALE ADHD AND BPD
4
[25] as they measured TCI traits and symptoms of personality disorder in a group
of outpatients with ADHD. ADHD was associated with low scores for Self-Directedness
and Cooperativeness but high scores for Harm Avoidance and Novelty Seeking; the
group of outpatients with ADHD also had high rates of BPD (37%). In light of the
fact that the personality disorders were described in this study using both the TCI
and the Structured Clinical Interview for DSM-IV Personality Disorders, the authors
conclude that the results confirm the assumption that neuropsychiatric disorders
with a childhood onset reflect a difficult underlying temperament, deficits in
character maturation, and personality disorders. They also conclude that a “typical
ADHD temperament” corresponds to an explosive/borderline type of personality
with high Novelty Seeking and Harm Avoidance in combination with low Reward
Dependence.
These results thus appear to show ADHD and BPD to share a number of
temperament and character traits. In these earlier studies, however, neither the
comorbid presence of ADHD in the BPD samples nor the comorbid presence of BPD
in the ADHD samples were controlled for.
Aims of the present studyAmong the aims of the present study was examination of the role of temperament
and character traits in the differentiation of groups of ADHD and BPD patients
with differing degrees of ADHD and BPD symptoms. In order to do this, latent
classes of individuals with similar symptom profiles were used rather than DSM-IV
subgroups. The advantage of using latent classes as opposed to actual DSM-IV
subgroups is that the latent classes are phenomenologically homogeneous groups
(i.e., groups composed of individuals with clearly similar symptom profiles);
subgroups formed on the basis of the DSM-IV, in contrast, tend to be less
homogeneous as an ADHD classification without a BPD classification, for example,
does not imply a total absence of BPD symptoms.
Given that the different temperament dimensions of personality are supposed
to reflect individual differences in basic emotional drives, clear differences in the
TCI profiles of the latent classes of individuals were expected to be found. Given
that BPD is characterized by a greater instability of emotion regulation than
ADHD, the latent classes with mainly BPD symptomatology were expected to show
comparatively high levels of Harm Avoidance (first hypothesis). Given that ADHD
and BPD are both characterized by impulsive behavior, high Novelty Seeking
scores were expected to be found for all of the latent classes of ADHD and BPD with
those classes with both BPD and ADHD symptomatology showing the highest
scores (second hypothesis). In keeping with Cloninger’s assumption that low
character scores are indicative of personality disorders and that ADHD is not a
personality disorder, lower Self-Directedness and Cooperativeness scores were

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
76
CHAPTER 4
expected to be found for the latent classes of individuals with BPD symptomatology
than for the latent classes of individuals with only ADHD symptomatology (third
hypothesis).
Method
Subjects and assessmentParticipants were consecutively recruited female patients referred to the ou t-
patient ADHD program or outpatient BPD program at the Department of Psychiatry,
Radboud University Nijmegen Medical Centre, The Netherlands. The patients were
recruited during a period of approximately 3 years and had to meet the DSM-IV
criteria for ADHD or BPD to be included in the study. Patients with clinically
significant chronic medical conditions, mental retardation, organic brain disorders,
or schizophrenia were excluded from the study. Patients with other comorbid
psychiatric disorders were not excluded in order to make the sample as
representative of the actual clinical population as possible. Diagnostic assessment
was part of the standard clinical diagnostic procedures and the part related to the
present ADHD research projects was approved by the local Medical Ethical
Committee. All patients signed an informed consent form prior to participation.
Out of a total of 45 patients recruited from the ADHD program, 5 were
excluded: 4 dropped out without notification and 1 considered the procedure too
stressful. Out of a total of 78 patients recruited from the BPD program, 15 were
excluded: 3 dropped out without notification, 11 did not meet the DSM-IV criteria
for BPD, and 1 was diagnosed with schizophrenia. The final sample thus included
103 patients (or 84% of the recruited patients): 40 from the ADHD treatment
program and 63 from the BPD treatment program. Six (or 15%) of the ADHD
patients had a comorbid diagnosis of BPD, leaving 34 patients in this group with
ADHD alone (mean age = 35, SD = 12). Of the 63 BPD patients, 21 (or 33%) had a
comorbid diagnosis of ADHD (i.e., ADHD in childhood and adulthood), which left
42 patients in this group with what appeared to be BPD alone. We were unable to
attain informant accounts of childhood symptoms of ADHD for 13 of the 42
patients meeting the criteria for BPD. Of these 13, 5 met the criteria for ADHD in
adulthood; the other 8 cases did not meet the criteria for ADHD in adulthood,
which meant rejection of a possible diagnosis of ADHD. This left a total of 37
patients with a diagnosis of BPD alone (mean age = 31, SD=7). A total of 27 patients
had a clear diagnosis of both ADHD and BPD (mean age = 32, SD = 9).
Patients underwent comprehensive clinical assessment. This included psychiatric
evaluation and both structured and semi-structured diagnostic interviews, which
were conducted by trained psychologists or psychiatric trainees under the

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
77
TEMPERAMENT AND CHARACTER IN FEMALE ADHD AND BPD
4
supervision of a senior psychiatrist. The interviewers were blind to all prior
clinical diagnoses.
The presence of ADHD symptoms in childhood and adulthood (i.e., current)
was assessed using a Semi-Structured Interview for ADHD [26]. This interview has
been used in previous studies of adult ADHD [27-29] and shown to be both reliable
and valid. Confirmation of the developmental history and childhood occurrence
of ADHD symptoms was obtained from the parents or, when unavailable, an older
sibling of the patient. In addition, the Dutch versions of the ADHD-DSM-IV Rating
Scales [30] were completed by patient, spouse, parent, and investigator to gather
information on the exact DSM-IV criteria for ADHD in childhood and adulthood.
The following was required to be the case for assignment of a full diagnosis of
adult ADHD: (1) at least 6 of the 9 DSM-IV criteria for inattention and/or
hyperactivity/impulsivity had to be met for diagnosis of childhood ADHD and at
least 5 of the 9 criteria for diagnosis of adult ADHD; (2) a chronic course of persistent
ADHD symptoms from childhood to adulthood had to be reported; and (3) a
moderate to severe level of impairment that can be attributed to the symptoms of
ADHD had to be experienced. The cut-off point of 5 out of the 9 criteria for diagnosis
of adult ADHD is based upon the literature and epidemiological data using the
same DSM-IV ADHD Rating Scale [28,31,32].
The Structured Clinical Interview for DSM-IV Axis II Personality Disorders
(SCID-II) was used to determine the presence of BPD [33]. A BPD diagnosis was only
given when no Axis I syndrome (i.e., clinical disorder) could account for the
patient’s complaints or dysfunctioning. Axis-I comorbidity was assessed using the
Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) [33].
The Dutch version of Cloninger’s Temperament and Character Inventory (TCI)
was used to measure the temperament and character dimensions of personality.
The TCI has been shown to have good psychometric qualities on the basis of 1034
healthy individuals from the general population [35,36].
Statistical analysesIn previous work [8], latent class analysis (LCA) [7] was used to identify mutually
exclusive classes of ADHD and BPD patients with homogeneous symptom profiles.
Using Mplus version 4.1 [37], BPD symptoms in addition to childhood and adulthood
symptoms of ADHD were used to create symptom profiles for these periods. In the
present work, the scores of the patients on the TCI scales and subscales were
compared across the four latent classes of patients with adult diagnoses of ADHD
or BPD and homogeneous symptom profiles. The raw TCI subscale scores were
converted into gender corrected T-values using the Dutch/Flemish population
norms [36]. Given that part of the data was not normally distributed — as indicated
by Detrended Normal Q-Q plots and the Shapiro-Wilks test — the non-parametric

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
78
CHAPTER 4
Mann-Whitney U rank sum test for independent samples was adopted. The T-values
for the temperament and character dimensions of personality were compared to
an expected population mean of 50 (SD=10). All tests were two-tailed and the
p-value was set at .05. These calculations were done using SPSS (version 16.0).
Results
In Figure 1, an overview of the occurrence of adult ADHD and BPD symptoms for
the latent classes of patients is presented. Class 1(29/103 = 28%) shows ADHD
symptoms but no symptoms of BPD. The other three latent classes show BPD
symptoms in addition to symptoms of ADHD. Class 2 (20/103 = 19%) shows high
levels of BPD symptoms and moderate to high levels for the hyperactivity symptoms
of ADHD. Class 3 (32/103 = 31%) shows high levels of BPD symptoms and high levels
of symptoms for the inattention, hyperactivity, and impulsivity aspects of ADHD
(i.e., all aspects). Class 4 (22/103 = 21%) shows high levels of BPD symptoms and high
Figure 1 Latent class probabilities of adulthood ADHD and BPD symptoms in 103 female patients with ADHD, BPD, or both
0
10
20
30
40
50
60
70
80
90
100
Fail
s to
pay
att
enti
on t
o d
etai
ls
Dif
ficu
lty
sust
ain
ing
Dif
ficu
lty
care
full
y li
sten
ing
Dif
ficu
lty
foll
owin
g th
rou
gh o
f fi
nis
hin
g w
ork
Dif
ficu
lty
orga
niz
ing
task
s
Avo
ids
sust
ain
ing
men
tal
effo
rt
Lose
s th
ings
Easi
ly d
istr
acte
d
Forg
etfu
lnes
s
Fid
gest
wit
h h
and
s an
d f
eet
Oft
en l
eave
s se
at
Res
tles
snes
s m
otor
or
men
tal
acti
vity
Dif
ficu
lty
enga
gin
g in
lei
sure
Dri
ven
by
a m
otor
Talk
s ex
cess
ivel
y
Blu
rts
out
answ
ers
Dif
ficu
lty
awai
tin
g tu
rn
Inte
rru
pts
or
intr
ud
es
Avo
ids
aban
don
men
t
Un
stab
le a
nd
in
ten
se i
nte
rper
son
al r
elat
ion
ship
s
Ind
enti
ty d
istu
rban
ces
Pote
nti
ally
sel
f d
amag
ing
imp
uls
ivit
y
Self
mu
tila
tin
g or
su
icia
l be
hav
ior
Aff
ecti
ve i
nst
abil
ity
Ch
ron
ic f
eeli
ngs
of
emp
tin
ess
Dif
ficu
lty
con
trol
lin
g an
ger
Stre
ss-r
elat
ed p
aran
oia
or d
isso
ciat
ion
Perc
enta
ge
Class 1 (n=29) Class 2 (n=20) Class 3 (n=32) Class 4 (n=22)

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
79
TEMPERAMENT AND CHARACTER IN FEMALE ADHD AND BPD
4
levels for the inattention and hyperactivity aspects of ADHD. In Figure 2, the TCI
profiles for the four latent classes of patients are presented. The scores are
T-corrected means with 50 thus representing the expected population mean.
When the corrected TCI temperament scores for the latent classes of patients were
compared to the expected norm and across the different classes (Table 1), Novelty
Seeking showed significantly higher scores for classes 1, 3, and 4 relative to the
norm population. Only class 2, which was composed of patients with symptoms of
BPD and only symptoms of ADHD hyperactivity, produced average Novelty Seeking
scores when compared to the norm. Comparison of the latent classes of patients
showed Novelty Seeking in class 3, which involved high levels of both BPD and
ADHD symptoms in all areas, to be highest and significantly different from
Novelty Seeking in the other latent classes. The subscales of Novelty Seeking show
Figure 2 Temperament and Character Inventory profile in female adult classes of ADHD and BPD symptoms
Scores are given as T-corrected means. NS indicates Novelty Seeking; HA, Harm Avoidance; RD, Reward
Dependence; P, persistence; SD, Self-directedness; CO, Cooperativeness; ST, Self-Transcendence. Class 1:
ADHD inattention, hyperactivity, and impulsivity symptoms; class 2: BPD symptoms + ADHD hyperactivity
symptoms; class 3: BPD symptoms + ADHD inattention, hyperactivity, and impulsivity symptoms; class 4:
BPD symptoms + ADHD inattention and hyperactivity symptoms.
75
70
65
60
55
50
45
40
35
30
25NS HA RD P SD CO ST
T-sc
ore
Temperament & Character scales
Class 1 : 28,2%
Class 2 : 19,4%
Class 3 : 31,1%
Class 4 : 21,4%

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
80
CHAPTER 4
Tab
le 1
T-c
orre
cted
mea
ns
(an
d S
D) f
or t
emp
eram
ent
and
ch
arac
ter
dim
ensi
ons
of p
erso
nal
ity
in l
aten
t cl
asse
s of
10
3 fe
mal
e p
atie
nts
wit
h A
DH
D, B
PD, o
r b
oth
Cla
ss 1
(n
= 2
9)C
lass
2
(n =
20)
Cla
ss 3
(n
= 3
2)C
lass
4
(n =
22)
1 vs
21
vs 3
1 vs
42
vs 3
2 vs
43
vs 4
Mea
n (S
D)
Mea
n (S
D)
Mea
n (S
D)
Mea
n (S
D)
P
Nov
elty
See
kin
g60
(9.5
)a 5
5.7
(10.
9)
66.7
(7.5
)a59
.7 (1
1)a
NS
.005
NS
<.00
1N
S.0
18
Exp
lora
tory
exc
itab
ilit
y55
.3 (1
0.7)
48.3
(11.
4)51
.9 (9
.6)
47.8
(7.7
).0
39N
S.0
05N
SN
SN
S
Imp
uls
iven
ess
57.4
(10.
7)a
53.0
(11.
2)65
.3 (6
.0) a
59.1
(8.3
) aN
S.0
04N
S<.
001
NS
.005
Extr
avag
ance
57.0
(8.6
) a54
.2 (9
.5)
59.7
(9.9
) a59
.8 (9
.6) a
NS
NS
NS
.017
.030
NS
Dis
ord
erli
nes
s55
.4 (8
.5)b
60.3
(8.6
) a66
.1 (9
.6) a
58.1
(12.
4) a
NS
<.00
1N
S.0
29N
S.0
14
Har
m A
void
ance
54.4
(10.
9)59
.2 (1
1.9)
b61
.9 (9
.1) a
64.7
(5.1
) aN
S.0
09.0
01N
SN
SN
S
An
tici
pat
ory
wor
ry54
.6 (1
1.6)
57.6
(10.
3) b
63.1
(9.3
) a63
.1 (7
.5) a
NS
.003
.009
NS
NS
NS
Fear
of
un
cert
ain
ty49
.9 (1
2.2)
53.2
(12.
9)50
.2 (1
1)52
.7 (8
.6)
NS
NS
NS
NS
NS
NS
Shyn
ess
50.5
(7.3
)56
.3 (8
.1) b
55.6
(7.5
) a56
.9 (6
.3) a
.012
.011
.002
NS
NS
NS
Fati
gabi
lity
an
d a
sth
enia
57.4
(12.
5) b
59.2
(11.
8) b
64.7
(9.1
) a69
.3 (6
.3) a
NS
.022
<.00
1N
S.0
03.0
39
Rew
ard
Dep
end
ence
52.3
(9.8
)44
.6 (9
.4)
44.2
(10.
8) b
47.4
(8.8
).0
1.0
04.0
47N
SN
SN
S
Sen
tim
enta
lity
49.2
(9.5
)45
.0 (8
.6)
45.1
(10.
6)50
.4 (7
.8)
NS
NS
NS
NS
NS
NS
Att
ach
men
t53
.2 (9
.6)
46.2
(12.
9)47
.9 (1
0.7)
45.9
(10.
5)N
SN
S.0
29N
SN
SN
S
Dep
end
ence
53.2
(9.5
)49
.2 (9
.2)
44.9
(11.
7)49
.8 (1
1)N
S.0
05N
SN
SN
SN
S
Pers
iste
nce
51.9
(9.8
)53
.5 (7
.9)
51.3
(11)
49.9
(7.4
)N
SN
SN
SN
SN
SN
S
Self
-dir
ecte
dn
ess
44 (1
0.8)
b33
.9 (8
.8) a
29 (1
2.5)
a28
.5 (8
.4) a
.002
<.00
1<.
001
.044
NS
NS
Res
pon
sibi
lity
48.4
(10.
4)39
.8 (9
.2) a
34.4
(10.
9) a
36.6
(11.
9) a
.007
<.00
1.0
01.0
31N
SN
S
Purp
osef
uln
ess
43.7
(13.
7)38
.2 (1
0.8)
a34
.5 (1
3.3)
a36
.0 (1
0.6)
aN
S.0
13.0
27N
SN
SN
S
Res
ourc
efu
lnes
s44
.9 (1
3.1)
38.5
(13)
a38
.3 (1
3.7)
a30
.9 (8
) aN
S.0
48<.
001
NS
NS
NS
Self
-acc
epta
nce
44.8
(9.3
)b37
.6 (1
0.7)
a32
.4 (1
2.5)
a35
.2 (1
2.2)
a.0
22<.
001
.005
NS
NS
NS
Con
gru
ent
seco
nd
nat
ure
46.8
(8.6
)40
.2 (8
.7) a
38.7
(9.7
) a35
.8 (7
.1) a
.016
.002
<.00
1N
SN
SN
S
Coo
per
ativ
enes
s51
.8 (7
.4)
36.3
(11.
6) a
30.1
(16.
7) a
35.1
(15.
1) a
<.00
1<.
001
<.00
1N
SN
SN
S
Soci
al a
ccep
tan
ce49
.7 (1
1.5)
42.9
(12.
5)27
.6 (2
2.0)
a33
.7 (1
6.4)
a.0
25<.
001
<.00
1.0
20.0
48N
S
Emp
ath
y47
.2 (1
1.5)
41.2
(11.
8) b
36.0
(12.
9) a
38.4
(11.
6) a
NS
.001
.009
NS
NS
NS
Hel
pfu
lnes
s49
.4 (7
.4)
36.9
(10)
a39
.3 (1
5) a
40.0
(13.
8) b
<.00
1.0
03.0
06N
SN
SN
S
Com
pas
sion
54.2
(5.5
) b39
.3 (1
8)32
.8 (1
3.9)
a38
.6 (1
6.9)
b.0
10b.
001
.001
NS
NS
NS
Pure
hea
rted
nes
s53
.7 (9
.5)
42.3
(8.6
) a44
.6 (1
1.4)
a46
.4 (1
0.2)
<.00
1.0
01.0
11N
SN
SN
S
Self
-tran
scen
den
ce50
.8 (8
.9)
47 (8
.7)
50.8
(10.
1)52
.9 (9
.5)
NS
NS
NS
NS
.045
NS
Self
-forg
etfu
lnes
s55
.4 (1
1.6)
46.4
(9.8
)55
.1 (1
2.2)
53.6
(10.
6).0
07N
SN
S.0
09.0
16N
S
Tran
sper
son
al id
enti
fica
tion
45.2
(8.1
) b43
.9 (9
.2) b
46.2
(9)
47.6
(9.2
)N
SN
SN
SN
SN
SN
S
Spir
itu
al a
ccep
tan
ce51
.2 (8
.1)
50.8
(8.7
)50
.9 (1
0.5)
55.0
(8.9
)N
SN
SN
SN
SN
SN
S
Cla
ss 1
: A
DH
D i
nat
ten
tion
, h
yper
acti
vity
, an
d i
mp
uls
ivit
y sy
mp
tom
s; c
lass
2:
BPD
sym
pto
ms
+ A
DH
D h
yper
acti
vity
sym
pto
ms;
cla
ss 3
: B
PD s
ymp
tom
s +
AD
HD
inat
ten
tion
, hyp
erac
tivi
ty, a
nd
im
pu
lsiv
ity
sym
pto
ms;
cla
ss 4
: BPD
sym
pto
ms
+ A
DH
D i
nat
ten
tion
an
d h
yper
acti
vity
sym
pto
ms.
Man
n-W
hit
ney
U r
ank
sum
tes
t fo
r
ind
epen
den
t sa
mp
les
was
ad
opte
d f
or c
omp
aris
on o
f te
mp
eram
ent
and
ch
arac
ter
scal
es b
etw
een
late
nt
clas
ses.
α w
as s
et a
t .0
5.a D
iffe
ren
ce w
ith
nor
m g
rou
p (T
-cor
rect
ed m
ean
± S
D, 5
0 ±
10) i
s si
gnifi
can
t at
th
e .0
01 le
vel (
2-t
aile
d).
b Dif
fere
nce
wit
h n
orm
gro
up
(T-c
orre
cted
mea
n ±
SD
, 50
± 10
) is
sign
ifica
nt
at t
he
.01
leve
l (2
-tai
led)
.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
81
TEMPERAMENT AND CHARACTER IN FEMALE ADHD AND BPD
4
Tab
le 1
T-c
orre
cted
mea
ns
(an
d S
D) f
or t
emp
eram
ent
and
ch
arac
ter
dim
ensi
ons
of p
erso
nal
ity
in l
aten
t cl
asse
s of
10
3 fe
mal
e p
atie
nts
wit
h A
DH
D, B
PD, o
r b
oth
Cla
ss 1
(n
= 2
9)C
lass
2
(n =
20)
Cla
ss 3
(n
= 3
2)C
lass
4
(n =
22)
1 vs
21
vs 3
1 vs
42
vs 3
2 vs
43
vs 4
Mea
n (S
D)
Mea
n (S
D)
Mea
n (S
D)
Mea
n (S
D)
P
Nov
elty
See
kin
g60
(9.5
)a 5
5.7
(10.
9)
66.7
(7.5
)a59
.7 (1
1)a
NS
.005
NS
<.00
1N
S.0
18
Exp
lora
tory
exc
itab
ilit
y55
.3 (1
0.7)
48.3
(11.
4)51
.9 (9
.6)
47.8
(7.7
).0
39N
S.0
05N
SN
SN
S
Imp
uls
iven
ess
57.4
(10.
7)a
53.0
(11.
2)65
.3 (6
.0) a
59.1
(8.3
) aN
S.0
04N
S<.
001
NS
.005
Extr
avag
ance
57.0
(8.6
) a54
.2 (9
.5)
59.7
(9.9
) a59
.8 (9
.6) a
NS
NS
NS
.017
.030
NS
Dis
ord
erli
nes
s55
.4 (8
.5)b
60.3
(8.6
) a66
.1 (9
.6) a
58.1
(12.
4) a
NS
<.00
1N
S.0
29N
S.0
14
Har
m A
void
ance
54.4
(10.
9)59
.2 (1
1.9)
b61
.9 (9
.1) a
64.7
(5.1
) aN
S.0
09.0
01N
SN
SN
S
An
tici
pat
ory
wor
ry54
.6 (1
1.6)
57.6
(10.
3) b
63.1
(9.3
) a63
.1 (7
.5) a
NS
.003
.009
NS
NS
NS
Fear
of
un
cert
ain
ty49
.9 (1
2.2)
53.2
(12.
9)50
.2 (1
1)52
.7 (8
.6)
NS
NS
NS
NS
NS
NS
Shyn
ess
50.5
(7.3
)56
.3 (8
.1) b
55.6
(7.5
) a56
.9 (6
.3) a
.012
.011
.002
NS
NS
NS
Fati
gabi
lity
an
d a
sth
enia
57.4
(12.
5) b
59.2
(11.
8) b
64.7
(9.1
) a69
.3 (6
.3) a
NS
.022
<.00
1N
S.0
03.0
39
Rew
ard
Dep
end
ence
52.3
(9.8
)44
.6 (9
.4)
44.2
(10.
8) b
47.4
(8.8
).0
1.0
04.0
47N
SN
SN
S
Sen
tim
enta
lity
49.2
(9.5
)45
.0 (8
.6)
45.1
(10.
6)50
.4 (7
.8)
NS
NS
NS
NS
NS
NS
Att
ach
men
t53
.2 (9
.6)
46.2
(12.
9)47
.9 (1
0.7)
45.9
(10.
5)N
SN
S.0
29N
SN
SN
S
Dep
end
ence
53.2
(9.5
)49
.2 (9
.2)
44.9
(11.
7)49
.8 (1
1)N
S.0
05N
SN
SN
SN
S
Pers
iste
nce
51.9
(9.8
)53
.5 (7
.9)
51.3
(11)
49.9
(7.4
)N
SN
SN
SN
SN
SN
S
Self
-dir
ecte
dn
ess
44 (1
0.8)
b33
.9 (8
.8) a
29 (1
2.5)
a28
.5 (8
.4) a
.002
<.00
1<.
001
.044
NS
NS
Res
pon
sibi
lity
48.4
(10.
4)39
.8 (9
.2) a
34.4
(10.
9) a
36.6
(11.
9) a
.007
<.00
1.0
01.0
31N
SN
S
Purp
osef
uln
ess
43.7
(13.
7)38
.2 (1
0.8)
a34
.5 (1
3.3)
a36
.0 (1
0.6)
aN
S.0
13.0
27N
SN
SN
S
Res
ourc
efu
lnes
s44
.9 (1
3.1)
38.5
(13)
a38
.3 (1
3.7)
a30
.9 (8
) aN
S.0
48<.
001
NS
NS
NS
Self
-acc
epta
nce
44.8
(9.3
)b37
.6 (1
0.7)
a32
.4 (1
2.5)
a35
.2 (1
2.2)
a.0
22<.
001
.005
NS
NS
NS
Con
gru
ent
seco
nd
nat
ure
46.8
(8.6
)40
.2 (8
.7) a
38.7
(9.7
) a35
.8 (7
.1) a
.016
.002
<.00
1N
SN
SN
S
Coo
per
ativ
enes
s51
.8 (7
.4)
36.3
(11.
6) a
30.1
(16.
7) a
35.1
(15.
1) a
<.00
1<.
001
<.00
1N
SN
SN
S
Soci
al a
ccep
tan
ce49
.7 (1
1.5)
42.9
(12.
5)27
.6 (2
2.0)
a33
.7 (1
6.4)
a.0
25<.
001
<.00
1.0
20.0
48N
S
Emp
ath
y47
.2 (1
1.5)
41.2
(11.
8) b
36.0
(12.
9) a
38.4
(11.
6) a
NS
.001
.009
NS
NS
NS
Hel
pfu
lnes
s49
.4 (7
.4)
36.9
(10)
a39
.3 (1
5) a
40.0
(13.
8) b
<.00
1.0
03.0
06N
SN
SN
S
Com
pas
sion
54.2
(5.5
) b39
.3 (1
8)32
.8 (1
3.9)
a38
.6 (1
6.9)
b.0
10b.
001
.001
NS
NS
NS
Pure
hea
rted
nes
s53
.7 (9
.5)
42.3
(8.6
) a44
.6 (1
1.4)
a46
.4 (1
0.2)
<.00
1.0
01.0
11N
SN
SN
S
Self
-tran
scen
den
ce50
.8 (8
.9)
47 (8
.7)
50.8
(10.
1)52
.9 (9
.5)
NS
NS
NS
NS
.045
NS
Self
-forg
etfu
lnes
s55
.4 (1
1.6)
46.4
(9.8
)55
.1 (1
2.2)
53.6
(10.
6).0
07N
SN
S.0
09.0
16N
S
Tran
sper
son
al id
enti
fica
tion
45.2
(8.1
) b43
.9 (9
.2) b
46.2
(9)
47.6
(9.2
)N
SN
SN
SN
SN
SN
S
Spir
itu
al a
ccep
tan
ce51
.2 (8
.1)
50.8
(8.7
)50
.9 (1
0.5)
55.0
(8.9
)N
SN
SN
SN
SN
SN
S
Cla
ss 1
: A
DH
D i
nat
ten
tion
, h
yper
acti
vity
, an
d i
mp
uls
ivit
y sy
mp
tom
s; c
lass
2:
BPD
sym
pto
ms
+ A
DH
D h
yper
acti
vity
sym
pto
ms;
cla
ss 3
: B
PD s
ymp
tom
s +
AD
HD
inat
ten
tion
, hyp
erac
tivi
ty, a
nd
im
pu
lsiv
ity
sym
pto
ms;
cla
ss 4
: BPD
sym
pto
ms
+ A
DH
D i
nat
ten
tion
an
d h
yper
acti
vity
sym
pto
ms.
Man
n-W
hit
ney
U r
ank
sum
tes
t fo
r
ind
epen
den
t sa
mp
les
was
ad
opte
d f
or c
omp
aris
on o
f te
mp
eram
ent
and
ch
arac
ter
scal
es b
etw
een
late
nt
clas
ses.
α w
as s
et a
t .0
5.a D
iffe
ren
ce w
ith
nor
m g
rou
p (T
-cor
rect
ed m
ean
± S
D, 5
0 ±
10) i
s si
gnifi
can
t at
th
e .0
01 le
vel (
2-t
aile
d).
b Dif
fere
nce
wit
h n
orm
gro
up
(T-c
orre
cted
mea
n ±
SD
, 50
± 10
) is
sign
ifica
nt
at t
he
.01
leve
l (2
-tai
led)
.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
82
CHAPTER 4
this difference to be mainly due to the high scores on Impulsivity and Disorderliness
for class 3. In line with the total Novelty Seeking score on which class 2 scored
average compared to the norm, class 2 also scored average on Impulsivity and
Extravagance but above average on Disorderliness.
Significantly higher scores relative to the norm population were also found
for Harm Avoidance for classes 2, 3, and 4; class 1, which involved only symptoms
of ADHD hyperactivity, was an exception. Comparison of the latent classes of
patients showed Harm Avoidance to be highest in the latent classes with high
levels of BPD symptoms together with high levels of symptoms in all areas of
ADHD (class 3) and together with high levels of ADHD symptoms in the areas of
Inattention and Hyperactivity (class 4). The subscales of Harm Avoidance showed a
similar pattern: classes 2, 3 and 4 showed scores significantly above the normal
range with classes 3 and 4 also in particular with respect to class 1.
For the Reward Dependence aspect of temperament, a significantly lower score
than normal was found for class 3. Comparison of the latent classes showed Reward
Dependence to be significantly lower in classes 2, 3 and 4, which have the most
symptoms of ADHD in conjunction with BPD, than in class 1 with only symptoms
of ADHD. The RD subscales showed scores equal to the norm for all classes
Comparison of the classes revealed differences between classes 1 and 3 and classes
1 and 4 on the Attachment and Dependence subscales; class 1 scored significantly
higher on these subscales. All four of the latent classes showed normal scores for
the Persistence aspect of temperament.
With regard to the character dimensions of personality, significantly lower
Self-Directedness scores relative to the norm were found in all of the latent classes.
Comparison of the latent classes themselves showed the scores in class 1 with only
symptoms of ADHD to be significantly higher than the scores in the other three
classes, which all involve symptoms of both BPD and ADHD. The same pattern was
found for all 5 subscales of Self Directedness.
For Cooperativeness, significantly higher scores were found relative to the
norm for all of the latent classes with the exception of class 1 (i.e., the class with
only symptoms of ADHD). Comparison of the latent classes themselves showed
classes 2, 3, and 4 to not differ significantly from each other but to have significantly
higher Cooperativeness scores than class 1. The Cooperativeness subscales show a
similar pattern with the class 1 scores in the normal range and the scores for the
other classes below the normal range. The scores for the Self-Transcendence aspect
of character were average for all of the latent classes.
Overall, the present results show a high Novelty Seeking temperament in all
of the latent classes with the exception of that class with mostly BPD symptoms
(i.e., class 2). The highest Novelty Seeking temperament scores were found in that
class of patients with both symptoms of BPD and symptoms in all areas of ADHD

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
83
TEMPERAMENT AND CHARACTER IN FEMALE ADHD AND BPD
4
(i.e., class 3). The class of patients with only ADHD symptoms (i.e., class 1) scored
normal on Harm Avoidance while the other three classes of patients with BPD
symptoms in addition to symptoms of ADHD scored significantly higher than
normal on Harm Avoidance. With regard to the character dimensions of personality,
scores that were particularly lower than normal were found for Self-Directedness
and Cooperativeness in those classes of patients with BPD symptoms.
Discussion
In the present research, the TCI results for previously identified latent classes of
patients with similar ADHD and BPD symptom profiles were examined to identify
shared and unique personality characteristics. This was done to also gain greater
insight into the possible pathways from early temperament, in particular, to
future ADHD and/or BPD outcome. Specifically, we expected high scores on Novelty
Seeking for all classes of patients and perhaps even higher scores for those patients
with symptoms of both ADHD and BPD (i.e., classes 2, 3, and 4). We also expected
particularly high Harm Avoidance and low Cooperativeness for the class of patients
with mostly BPD symptomatology (i.e., class 2).
With the exception of the class of patients with mostly symptoms of BPD and
only ADHD symptoms of hyperactivity (i.e., class 2 patients), all of the patients
scored significantly above average on Novelty Seeking. Contrary to most previous
studies that associate a high Novelty Seeking temperament with BPD, it can
therefore be suggested that an above-average Novelty Seeking temperament is
most strongly linked to ADHD and less strongly linked to BPD. When the scores on
the subscales of Novelty Seeking were analyzed, we also found the patients in class
2 to show average scores on Impulsivity and Extravagance but above average scores
on Disorderliness, which indicates quick temperedness.
The highest Novelty Seeking scores were found for the class of patients with
symptoms of BPD and symptoms in all areas of ADHD (i.e., class 3 patients). These
patients not only scored highest compared to the expected population mean but
also compared to the other latent classes of patients. The question, thus, is why the
patients with the least ADHD symptoms (i.e., class 2) show only average scores for
Novelty Seeking (i.e., Impulsivity) while the highest Novelty Seeking scores are
found for those patients with the most symptoms of ADHD in combination with
symptoms of BPD (i.e., class 3). Regarding the first part of this question, we would
like to point out that the class 2 of patients was characterized by an absence of
problems in the ADHD area of inattention while inattention scores (i.e., this aspect
of ADHD) and Novelty Seeking scores (i.e., this aspect of temperament) were found
to be related for the other classes of patients. A temperament tendency towards

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
84
CHAPTER 4
impulsivity in response to novel stimuli (i.e., high Novelty Seeking) may thus be
strongly influenced by inattention problems. Regarding the second part of the
question, it is conceivable that a temperament predisposition for very high Novelty
Seeking can lead to the development of BPD in addition to ADHD. Having an
outspoken Novelty Seeking temperament and thus a predisposition to actively
respond to novel stimuli may well foster risky behavior on the part of the
individual, and this may — in turn — alter the course of the individual’s personality
development and thereby lead to the development of BPD at times. That is, insight
into the Novelty Seeking dimension of personality can shed light upon the relation
between ADHD and BPD as comorbid disorders.
As expected, we found the patients with BPD symptoms (i.e., those in classes
2,3, and 4) to score significantly higher than normal on Harm Avoidance with no
differences between these classes whereas those patients with only symptoms of
ADHD scored within the normal range. This finding appears to contradict previous
work in which ADHD was found to be associated with high Harm Avoidance [23-25]
but, as already mentioned, previous research may have been biased because there
was no control for comorbid personality disorders like BPD. We suspect that high
Harm Avoidance may be specifically linked to BPD, as demonstrated in previous
studies, but not to ADHD. And the present data suggests that ADHD patients
without symptoms of BPD are indeed less predisposed to be nervous, tense, and
insecure than ADHD patients with symptoms of BPD. That is, the present findings
are perfectly in line with the characterization of BPD in terms of emotional
instability.
Finally, the patients with symptoms of ADHD but no symptoms of BPD scored
significantly higher on the character dimensions Self-Directedness and Coopera-
tiveness than the other patients and, in fact, showed normal character development.
All of the patients with symptoms of BPD, in contrast, showed Self-Directedness
and Cooperativeness scores that point in the direction of deviant character
development. These results confirm Cloninger’s assumption that low scores on the
character scales of his inventory indicate a personality disorder. They are also in
line with other evidence showing low Self-Directedness and Cooperativeness
scores to be associated with BPD [19-22]. While ADHD thus relates to temperament
and thereby personality, it should not be conceptualized as a personality disorder.
This is an important finding with clear clinical implications. Using the TCI, it is
possible to differentiate ADHD accompanied by a mature character versus ADHD
accompanied by a personality disorder. It goes without saying that such
information is important for the indication and outcome of treatment.
A limitation in the present research is that a relatively small sample of only
female subjects was used. The sample was acceptable for LCA but limited to female
ADHD and BPD populations. The research should thus be extended and replicated

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
85
TEMPERAMENT AND CHARACTER IN FEMALE ADHD AND BPD
4
with larger and more varied samples. A definite strength of the present study is
nevertheless that it used a well-defined and carefully diagnosed sample; clinical
interviews with a number of parties and not just patient self-reports were also
employed.
To summarize, the female patients with similar patterns of ADHD and BPD
symptoms (i.e. the four classes) in the present study showed different temperament
and character traits. It is therefore suggested that the temperament trait of high
Novelty Seeking is linked to ADHD and, more specifically, to the inattention
domain of ADHD while the temperament trait of high Harm Avoidance and the
character traits of low Self-Directedness and low Cooperativeness appear to be
linked to BPD. An outspoken Novelty Seeking temperament may nevertheless
predispose the individual to develop a comorbid BPD although this is only part of
a more complicated picture.
Novelty Seeking — perhaps in combination with Harm Avoidance — may well
play a role in the etiology of BPD but, as for most mental disorders, no single factor
can explain the emergence and development of BPD. Multiple risk factors,
biological, psychological, and social, play a role in the etiology of mental disorders
and certainly BPD [38]. It is well-known, for example, that sexual and physical
abuse can contribute to the occurrence of borderline symptoms and that such
abuse often occurs within the context of a disturbed family environment [39,40].
However, the co-occurrence of these factors makes it difficult to distinguish the
effects of the abuse from the effects of the family environment. The personality
characteristics of parents may also contribute genetically, environmentally, and
interactively to the development of personality pathology. In future research, all
of these factors must be taken into consideration in order to better understand the
role of early differences in personality in the shaping of adult personality and the
occurrence of such psychiatric disorders as ADHD and BPD. In the present study,
the focus was on the biological factor of personality (i.e. temperament) and a valid
manner of exploring the co-occurrence of ADHD and BPD in adulthood was shown
to help us to map the heterogeneous course of these overlapping syndromes.
AcknowledgmentsRose Collard, research nurse, Marjan Knippenberg, MSc, and Marleen Bastiaanse,
MSc, are gratefully acknowledged for their expert research assistance. Pieter van
de Broek is gratefully acknowledged for his close collaboration on the data
collection.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
86
CHAPTER 4
References
[1] Andrulonis PA, Glueck BC, Stroebel CF, Vogel NG, Shapiro AL, Aldridge DM. Organic brain dysfunction
and the borderline syndrome. Psychiatr Clin North Am 1981 Apr;4(1):47-66.
[2] Andrulonis PA, Glueck BC, Stroebel CF, Vogel NG. Borderline personality subcategories. J Nerv Ment
Dis 1982 Nov;170(11):670-9.
[3] Dowson JH, McLean A, Bazanis E, Toone B, Young S, Robbins TW, et al. The specificity of clinical char-
acteristics in adults with attention-deficit/hyperactivity disorder: a comparison with patients with
borderline personality disorder. Eur Psychiatry 2004 Apr;19(2):72-8.
[4] Fossati A, Novella L, Donati D, Donini M, Maffei C. History of childhood attention deficit/hyperactivity
disorder symptoms and borderline personality disorder: a controlled study. Compr Psychiatry 2002
Sep;43(5):369-77.
[5] Philipsen A, Limberger MF, Lieb K, Feige B, Kleindienst N, Ebner-Priemer U, et al. Attention-deficit
hyperactivity disorder as a potentially aggravating factor in borderline personality disorder. Br J
Psychiatry 2008 Feb;192(2):118-23.
[6] Rey JM, Morris-Yates A, Singh M, Andrews G, Stewart GW. Continuities between psychiatric disorders
in adolescents and personality disorders in young adults. Am J Psychiatry 1995 Jun;152(6):895-900.
[7] McCutcheon A.L. Latent Class Analysis. Newbury Park: CA: Sage; 1987.
[8] Van Dijk FE, Lappenschaar GAM, Kan CC, Van den Broek PJ, Verkes R.J., Buitelaar JK. Lifespan
attention deficit/hyperactivity disorder and borderline personality disorder symptoms in female
patients: a latent class approach. Under Review 2011.
[9] White JD. Personality, temperament, and ADHD: a review of the literature. Personality and Individual
Differences 1999;27:589-98.
[10] Martel MM, Nigg JT, von EA. How do trait dimensions map onto ADHD symptom domains? J Abnorm
Child Psychol 2009 Apr;37(3):337-48.
[11] Nigg JT. Temperament and developmental psychopathology. J Child Psychol Psychiatry 2006
Mar;47(3-4):395-422.
[12] Sonuga-Barke EJ. Causal models of attention-deficit/hyperactivity disorder: from common simple
deficits to multiple developmental pathways. Biol Psychiatry 2005 Jun 1;57(11):1231-8.
[13] Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character.
Arch Gen Psychiatry 1993 Dec;50(12):975-90.
[14] Cloninger CR. A systematic method for clinical description and classification of personality variants.
A proposal. Arch Gen Psychiatry 1987 Jun;44(6):573-88.
[15] Cloninger CR. A systematic method for clinical description and classification of personality variants.
A proposal. Arch Gen Psychiatry 1987 Jun;44(6):573-88.
[16] Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character.
Arch Gen Psychiatry 1993 Dec;50(12):975-90.
[17] Cloninger CR. A practical way to diagnosis personality disorder: a proposal. J Personal Disord
2000;14(2):99-108.
[18] Svrakic DM, Whitehead C, Przybeck TR, Cloninger CR. Differential diagnosis of personality disorders
by the seven-factor model of temperament and character. Arch Gen Psychiatry 1993 Dec;50(12):991-9.
[19] de la Rie SM, Duijsens IJ, Cloninger CR. Temperament, character, and personality disorders. J Pers
Disord 1998;12(4):362-72.
[20] Svrakic DM, Whitehead C, Przybeck TR, Cloninger CR. Differential diagnosis of personality disorders
by the seven-factor model of temperament and character. Arch Gen Psychiatry 1993 Dec;50(12):991-9.
[21] Fossati A, Donati D, Donini M, Novella L, Bagnato M, Maffei C. Temperament, character, and
attachment patterns in borderline personality disorder. J Pers Disord 2001 Oct;15(5):390-402.
[22] Barnow S, Herpertz SC, Spitzer C, Stopsack M, Preuss UW, Grabe HJ, Kessler C, Freyberger HJ.
Temperament and character in patients with borderline personality disorder taking gender and
comorbidity into account. Psychopathology 2007;40:369- 379.
[23] Downey KK, Stelson FW, Pomerleau OF, Giordani B. Adult attention deficit hyperactivity disorder:
psychological test profiles in a clinical population. J Nerv Ment Dis 1997 Jan;185(1):32-8.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
87
TEMPERAMENT AND CHARACTER IN FEMALE ADHD AND BPD
4
[24] Lynn DE, Lubke G, Yang M, McCracken JT, McGough JJ, Ishii J, et al. Temperament and character
profiles and the dopamine D4 receptor gene in ADHD. Am J Psychiatry 2005 May;162(5):906-13.
[25] Anckarsater H, Stahlberg O, Larson T, Hakansson C, Jutblad SB, Niklasson L, et al. The impact of
ADHD and autism spectrum disorders on temperament, character, and personality development.
Am J Psychiatry 2006 Jul;163(7):1239-44.
[26] Kooij JJS. ADHD bij volwassenen. Inleiding in diagnostiek en behandeling. Lisse: Swets & Zeitlinger;
2002.
[27] Kooij JJ, Aeckerlin LP, Buitelaar JK. [Functioning, comorbidity and treatment of 141 adults with
attention deficit hyperactivity disorder (ADHD) at a psychiatric outpatient department. Ned Tijdschr
Geneeskd 2001 Aug 4;145(31):1498-501.
[28] Kooij JJ, Buitelaar JK, van den Oord EJ, Furer JW, Rijnders CA, Hodiamont PP. Internal and external
validity of attention-deficit hyperactivity disorder in a population- based sample of adults. Psychol
Med 2005 Jun;35(6):817-27.
[29] Kooij JS, Boonstra AM, Vermeulen SH, Heister AG, Burger H, Buitelaar JK, et al. Response to methyl-
phenidate in adults with ADHD is associated with a polymorphism in SLC6A3 (DAT1). Am J Med
Genet B Neuropsychiatr Genet 2007 Oct 22.
[30] DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. ADHD Rating Scale-IV. Checklists, Norms and Clinical
Interpretation. New York: The Guilford press; 1998.
[31] Murphy K, Barkley RA. Prevalence of DSM-IV symptoms of ADHD in adult licensed drivers:
Implications for clinical diagnosis. Journal of Attention Disorders 1996;1(3):147-61.
[32] Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity
disorder: impact of remission definition and symptom type. Am J Psychiatry 2000 May;157(5):816-8.
[33] Weertman A, Arntz A, Kerkhofs MLM. Structured Clinical Interview for DSM-IV Axis II Personality
Disorders. Lisse, the Netherlands: Swets & Zeitlinger BV; 2000.
[34] Groenestijn MAC, Akkerhuis GW, Kupka RW, Schneider N, Nolen WA. Structured Clinical Interview
for DSM-IV Axis I Disorders. Lisse, the Netherlands: Swets & Zeitlinger BV; 1999.
[35] Cloninger CR. A practical way to diagnosis personality disorder: a proposal. J Personal Disord
2000;14(2):99-108.
[36] Duijsens IJ, Spinhoven Ph. Handleiding van de Nederlandse Temperament en Karakter Vragenlijst.
Leiderdorp: Datec; 2000.
[37] Muthén LK, Muthén BO. Mplus user’s guide. Statistical analysis with latent variables (4th ed.; version
4.1). Los Angeles: Muthén & Muthén; 2006.
[38] Paris J. Borderline personality disorder. CMAJ 2005 Jun 7;172(12):1579-83.
[39] Bandelow B, Krause J, Wedekind D, Broocks A, Hajak G, Ruther E. Early traumatic life events, parental
attitudes, family history, and birth risk factors in patients with borderline personality disorder and
healthy controls. Psychiatry Res 2005 Apr 15;134(2):169-79.
[40] Bradley R, Jenei J, Westen D. Etiology of borderline personality disorder: disentangling the
contributions of intercorrelated antecedents. J Nerv Ment Dis 2005 Jan;193(1):24-31.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Published as:
Van Dijk FE, Schellekens AFA, Van den Broek P, Kan CC, Verkes RJ & Buitelaar JK. (2014)
Do cognitive measures of response inhibition differentiate between
Attention Deficit/Hyperactivity Disorder and Borderline Personality Disorder?
Psychiatry Research, 215(3):733-9.
Do cognitive measures of response inhibition differentiate between
attention deficit/hyperactivity disorder and borderline personality disorder?
5

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
90
CHAPTER 5
Abstract
This study examined whether cognitive measures of response inhibition derived
from the AX-CPT are able to differentiate between adult attention deficit/hyper -
activity disorder (ADHD), borderline personality disorder (BPD), and healthy
controls (HC). Current DSM-IV-TR symptoms of ADHD and BPD were assessed by
structured diagnostic interviews, and parent developmental interviews were used
to assess childhood ADHD symptoms. Patients (14 ADHD, 12 BPD, 7 ADHD and BPD,
and 37 HC) performed the AXCPT. Seventy percent of AX-CPT trials were target
(AX) trials, creating a bias to respond with a target response to X probes in the
nontarget (AY, BX, BY) trials. On BX trials, context, i.e. the non-‘A’ letter, must be
used to inhibit this prepotent response tendency. On AY trials context actually
causes individuals to false alarm. The effects of ADHD and BPD on AX-CPT outcome
were tested using two-way ANOVA. BPD was associated with higher percentage of
errors across the task and more errors and slower responses on BX trials, whereas
ADHD was associated with slower responses on AY trials. The findings suggest
response inhibition problems to be present in both ADHD and BPD, and patients
with BPD to be particularly impaired due to poor context processing.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
91
RESPONSE INHIBITION IN ADHD AND BPD
5
Introduction
Previous research has shown significant co-occurrence of DSMIV-TR defined
borderline personality disorder (BPD) and attention deficit hyperactivity disorder
(ADHD) in adults with the use of self-report questionnaires or structured psychiatric
interviews. Up to 60% of BPD patients met criteria for ADHD in childhood and up
to 38% of BPD patients showed a co-occurring adult ADHD diagnosis. Impulsivity
symptoms and traits are important overlapping features (Andrulonis et al., 1981,
1982; Rey et al., 1995; Fossati et al., 2002; Dowson et al., 2004a; Philipsen et al., 2008;
Ferrer et al., 2010; van Dijk et al., 2011, 2012). This behavioral overlap influences
diagnostic outcome and indications for treatment. It is therefore important to
clarify whether the shared symptoms are pointing to the same underlying
cognitive processes or whether BPD and ADHD can be differentiated at the level
of cognitive processes.
It is suggested that impulsive behavior, broadly defined as the tendency to act
prematurely without foresight, is not a unitary construct, but rather consists of
several independent dimensions involving various forms of impaired cognitive
control. Impulsivity could incorporate behavior that has not adequately sampled
sensory evidence (“reflection impulsivity”), a failure of motor or response inhibition
(“impulsive action”), a tendency to accept small immediate or likely rewards versus
large delayed or unlikely ones (“impulsive choice”) and risky behavior, in the
context of decision making (Evenden, 1999).
Reviews (Woods et al., 2002; Hervey et al., 2004; Seidman et al., 2004; Boonstra
et al., 2005; Schoechlin and Engel, 2005) and several more recent single studies
(Fischer et al., 2005; Nigg et al., 2005b; Faraone et al., 2006; Biederman et al., 2007;
Stavro et al., 2007; Boonstra et al., 2010) are clear in showing that adults with
ADHD have deficits in executive functioning in general and response inhibition
(i.e. the behavioral phenomena of “impulsive action”) in particular. In fact,
inhibitory dysfunction is regarded as underpinning one of a number of dissociable
and different pathways to ADHD (Nigg et al., 2005c; Sonuga-Barke et al., 2010).
However, it remains unclear if inhibition deficiencies are specific for ADHD,
especially with regard to BPD. Non-ADHD clinical control groups with mood and
anxiety disorders appeared to perform better on response inhibition tasks than
adults with ADHD (Barkley et al., 2001; Epstein et al., 2001; Murphy et al., 2001),
but patients with schizophrenia perform equally worse as patients with ADHD
(Ross et al., 2000).
The results of neuropsychological studies of patients with BPD are mixed but
mostly indicate that individuals with BPD also exhibit inhibitory dysfunction.
Problems with an impulsive response style with difficulty delaying, a preference
for immediate gratification, and impairments that reflect the inhibition of

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
92
CHAPTER 5
ongoing responses are frequently found in mostly female patients with BPD when
compared to healthy controls (Leyton et al., 2001; Bazanis et al., 2002; Dinn et al.,
2004; Nigg et al., 2005a; de Bruijn et al., 2006; Grootens et al., 2008b; Rentrop et al.,
2008; McCloskey et al., 2009; Volker et al., 2009; Lawrence et al., 2010).
Deficient inhibitory control in its broadest sense may thus underlie both
ADHD and BPD. However, it is currently unclear to what extent BPD is associated
with response inhibition problems independently of the frequently co-occurring
ADHD. To date, we found four studies comparing patients with ADHD and BPD
in terms of neuropsychological overlap and differences.
The first one, although not focusing on response inhibition in particular,
compared adults with ADHD, BPD and healthy controls (each group N¼19). No
significant group differences were found for spatial working memory and spatial
recognition memory, but the mean deliberation time for the decision-making task
was significantly longer in the BPD than in the other groups, and with a significant
difference between the BPD and ADHD group. The authors concluded that subjects
with ADHD and BPD may have dissociable patterns of neuropsychological
impairments (Dowson et al., 2004b).
Another study did focus on response inhibition in particular and measured
stop signal reaction times in 105 adults with ADHD (of whom 20% with co-occurring
BPD) and 90 controls (Nigg et al., 2005a). The results provided evidence that problems in
response inhibition are specific to BPD symptoms even when symptoms of other
personality disorders, lifetime depression, anxiety, and posttraumatic symptoms
are controlled for. However, this effect could still be due to the overlap of BPD and
ADHD symptoms. When ADHD symptoms were entered as a predictor, response
inhibition ceased to be significantly associated with BPD symptoms, probably due
to the high correlation of ADHD and BPD in the sample. The authors emphasize
the importance of clarifying whether BPD per se is related to problems of response
inhibition.
A third study compared four groups of participants (22 ADHD, 21 BPD, 20
ADHD with BPD and 20 Healthy Controls) on various inhibitory functions. ADHD
patients performed significantly worse on tasks that measure the ability to
interrupt an already ongoing response, but showed no significant deficits in the
capacity to suppress prepotent responses as tested with the error rate of a go/no go
test. In all inhibitory tasks, ADHD subjects showed generally longer RTs than
controls. Patients with ADHD and BPD did not differ significantly from those with
pure ADHD on any cognitive task and the BPD group achieved better results than
the ADHD group in most tasks. The authors conclude that impaired inhibition is a
core feature in adults with ADHD, but not in adults with BPD, and that ADHD and
BPD have no common attention or inhibitory deficits (Lampe et al., 2007).

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
93
RESPONSE INHIBITION IN ADHD AND BPD
5
The most recent study explored the role of stress in different components of
impulsivity, including response inhibition, in four groups of participants (15 BPD,
15 BPD with ADHD, 15 ADHD and 15 healthy controls) (Krause-Utz et al., 2013). The
results showed impaired response inhibition as measured with the Immediate and
Delayed Memory Task (IMT/DMT) in patients with both BPD and ADHD, but not in
those with BPD but without ADHD.
In summary, these studies seem to contradict the probable shared response
inhibition problems between ADHD and BPD as well as the previous findings of
inhibitory dysfunction in BPD. Given these inconsistencies might be explained in
part by heterogeneity in the inclusion and exclusion criteria, the issue of response
inhibition in BPD and ADHD needs further investigation.
Continuous performance tasks (CPT’s) are among the most used tasks to assess
impulsive action. CPT’s are based on the paradigm that a global prepotency of
response is created that must occasionally be overridden by voluntary control
(Rosvold and Delgado, 1956). Research on this paradigm has been relatively
voluminous, in both the experimental and the clinical literature (Riccio and
Reynolds, 2001; Riccio et al., 2002). Several studies have associated ADHD with
impaired CPT performance but comparison with clinical samples is scarce (Woods
et al., 2002; Hervey et al., 2004). We found four studies reporting specifically on
CPT performance in BPD of which the results are ambiguous. One study showed
slightly but not significantly more errors in female BPD patients compared to
healthy controls but not to individuals with depression (Volker et al., 2009). Yet two
other studies found significantly more errors and more inattentiveness on the CPT
indices in patients with BPD compared with non-psychiatric controls (Rubio et al.,
2007; Ruocco et al., 2012). The most recent study investigated response inhibition
and working memory together with elementary cognitive processes in BPD
and healthy controls (Hagenhoff et al., 2013). As in other tasks, they found no
impairments of response inhibition in the AX-CPT results. Moreover they found
faster responses along with comparable accuracy, suggesting a superiority of faster
cognitive processing in BPD. Correctly, the authors mention that it has to be
investigated whether this alteration might shift into a disadvantage when task
characteristics favor impulsive responding. Also, faster motor reactions may be an
indication of response inhibition deficit (Conners, 2000).
In the present study we aim to examine whether cognitive measures of
response inhibition derived from an Expectancy AX version of the Continuous
Performance Task (AX-CPT) are able to differentiate between ADHD, BPD, and
healthy controls. An advantage of using the AX-CPT is that it takes into account
that response inhibition also depends on context processing, i.e. the representation,
maintenance and updating of context in prefrontal networks (Braver et al., 2009).
From this perspective, inhibition is the processing of task-relevant information to

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
94
CHAPTER 5
provide the top down support needed to allow secondary responses to compete
effectively with distracting information. In the AX-CPT task, contextual information,
conceptualized as any task relevant information that is internally represented, is
required to drive or inhibit responses to a target stimulus (Braver and Barch, 2002).
In the Expectancy AX-CPT, AX trials comprise a large portion (70%) of the overall
task which creates a strong expectancy and tendency toward responding with the
target button. Participants ability to inhibit this prepotent tendency is particularly
evident on the small portion (10%) of the remaining trials in which the cue letter
A is followed by a probe letter other than X (i.e. an AY trial). Errors occur if
participants respond when they are required to inhibit their response and high
error rate points to difficulties with response inhibition.
On another portion (10%) of the non-target trials, a cue letter other than A is
followed by the probe letter X (i.e. a BX trial). Note that on BX trials, the internal
representation of context should improve performance, by inhibiting an
inappropriate response bias. However, on AY trials, representation of context
should impair performance, by creating an inappropriate expectancy bias.
Thus, if context representations are intact, AY performance should be worse
than BX performance (both in errors and or RT). Conversely, if context representa-
tions are impaired, BX performance should be worse than AY performance.
Performance on AX target trials should also be poorer if context processing is
impaired, since determination of targets is dependent upon the context provided
by the cue. However, AX performance should not be as impaired as BX performance,
since on AX trials, the response bias works in subjects favor, by increasing the
tendency to make the correct target response. Finally, a third type of nontarget
trial, BY, provides a useful internal control, since in these trials the influence of
context on performance should be relatively small (given that both the cue and the
probe always map to a nontarget response) (Servan-Schreiber et al., 1996; Cohen et
al., 1999; Barch et al., 2004; Bodner et al., 2012). The expectancy variant of the AX
CPT paradigm has the potential to produce a double dissociation in performance:
individuals with a context-processing deficit would show impaired performance
on BX trials, whereas those with intact context-processing would perform worse
on AY trials (MacDonald, 2008).
We aim to examine whether cognitive measures of response inhibition derived
from an Expectancy AX version of the Continuous Performance Task (AX-CPT) are
able to differentiate between ADHD, BPD, and healthy controls. We anticipate
finding response inhibition problems in BPD independent of ADHD. Further, given
that BPD is a personality disorder encompassing deficits in social and emotional
functioning that are broader than just impulse control, we expect BPD to be
associated with problems in context processing.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
95
RESPONSE INHIBITION IN ADHD AND BPD
5
Method
SubjectsParticipants were consecutively recruited patients referred to the in- and
outpatient ADHD program or BPD program at the Department of Psychiatry of
the Radboud University Nijmegen Medical Centre, the population of the GGZ
Oost Brabant (sites Oss and Veghel) and Spatie Mental Health Centre (Apeldoorn) in
The Netherlands. The patients were recruited during a period of approximately
2 years and had to meet the DSM-IV criteria for ADHD or BPD to be included in the
study. Patients were excluded if they met DSM-IV-TR criteria for depressive disorder,
bipolar disorder, schizophrenia, schizoaffective disorder, schizophreniform disorder,
delusional disorder, other psychotic disorders, schizoid or schizotypal personality
disorder, (history of) alcohol- or substance dependence, and if they had first degree
relatives with DSM-IV axis I schizophrenia, or schizophreniform disorder. Patients
with a history of trauma capitis, visual and auditory disorders, neurological
disorders, and if they had first-degree relatives with any relevant neurological or
psychiatric disorders were also excluded. Diagnostic assessment was part of the
standard clinical diagnostic procedures.
The healthy volunteers were recruited by means of advertisements in local
newspapers. The volunteers had a negative history for psychiatric disorders and
were matched with the patient groups on sex, age and education. All subjects were
paid 10 euro per hour for their participation. The present study was conducted in
accordance with the declaration of Helsinki. Approval of this study was obtained
from the local ethics committee. All participants signed an informed consent
form prior to participation. A total of 78 subjects, aged 18 to 50, participated in the
study on the basis of informed consent and having been diagnosed according to
the DSM-IV-TR system with ADHD (N=19) or BPD (N=17), or being healthy controls
(HC) (N=42). All diagnoses were established after a systematic and comprehensive
psychiatric assessment had been performed. This included a psychiatric evaluation
and both structured and semi-structured diagnostic interviews, which were
conducted by trained psychologists or psychiatric trainees under the supervision
of a senior
psychiatrist.
The presence of ADHD symptoms in childhood and adulthood (i.e. current)
was assessed using a Semi-Structured Interview for ADHD (Kooij, 2002). This
interview has been used in previous studies of adult ADHD (Kooij et al., 2001, 2005)
and shown to be both reliable and valid. Confirmation of the developmental
history and childhood occurrence of ADHD symptoms was obtained from the
parents or, when unavailable, an older sibling of the patient. In addition, the Dutch
versions of the ADHD-DSM-IV Rating Scales (DuPaul et al., 1998) were completed by

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
96
CHAPTER 5
patient, spouse, parent, and investigator to gather information on the exact
DSM-IV criteria for ADHD in childhood and adulthood. The following was required
to be the case for assignment of a full diagnosis of adult ADHD: (1) at least 6 of the
9 DSM-IV criteria for inattention and/or hyperactivity/impulsivity had to be met
for diagnosis of childhood ADHD and at least 5 of the 9 criteria for diagnosis of
adult ADHD; (2) a chronic course of persistent ADHD symptoms from childhood to
adulthood had to be reported; and (3) a moderate to severe level of impairment
that can be attributed to the symptoms of ADHD had to be experienced. The cut-off
point of 5 out of the 9 criteria for diagnosis of adult ADHD is based upon the
literature and epidemiological data using the same DSM-IV ADHD Rating Scale
(Kooij et al., 2005) and in accordance with the current ADHD definition in DSM-5.
The Structured Clinical Interview for DSM-IV Axis II Personality Disorders
(SCID-II) was used to determine the presence of BPD (Weertman et al., 2000). A BPD
diagnosis was only given when no Axis I syndrome (i.e. clinical disorder) could
account for the patients complaints or dysfunctioning. Axis-I comorbidity was
assessed using the Structured Clinical Interview for DSM-IV Axis I Disorders
(SCIDI) (Groenestijn et al., 1999). Since we were especially interested in the differ-
entiation of the overlapping impulsivity symptoms in ADHD and BPD, we included
only those patients with impulsivity symptoms as specified in the DSM-IV for
ADHD (i.e. satisfying criteria for ADHD predominantly hyperactive/impulsive type
or ADHD combined type) and/or BPD (i.e. satisfying criterion 4 (impulsivity) of the
BPD section in the SCID-II). All patients had an estimated average or above average
intelligence based on clinical judgment and educational level. Educational level
was determined using a three level classification, (level 1: primary school or less,
level 2: secondary school, level 3: higher education or university) based on the
Dutch education system. Healthy controls were screened using the Dutch version
of the M.I.N.I. Plus structured interview (Sheehan et al., 1998) and ADHD self-report
rating scale.
Participants completed the neuropsychological testing after the instruction
not to use alcohol more than 3 units/day (one unit stands for the so called “standard
drink” in the Netherlands, which contains 12 ml or 10 g of alcohol) during the
week before the experimental measures, not to use alcohol within 24 h before
measurement, not to use cannabis or other illicit drugs within the week before
measurement, not to use any psychotropic medication, other than oxazepam,
during the 5 days before measurement, not to use oxazepam within 12 h before
measurement and not to smoke within 3 h before measurement. Patients using
methylphenidate were not allowed to use it on the day of the experiment.
Of the total sample of 78 participants, 8 participants (3 BPD and 5 HC) were
detected as obvious outliers far outside the 95% confidence interval. They made
systematically too many errors of all kind. We suspect either miscomprehension of

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
97
RESPONSE INHIBITION IN ADHD AND BPD
5
the task or lack of motivation for the task. Unfortunately, we do not know the
actual cause of these outliers. We removed these cases in order to get the most
honest estimate of population parameters possible. The final sample consisted of
70 participants: 14 Patients with ADHD (mean age=41.9 years; male: female ratio 7:7),
12 patients with BPD (mean age=27.3 years; male: female ratio 0:12), 7 patients
with both ADHD and BPD (mean age=35 years; male: female ratio 3:4), and 37
healthy controls (mean age=31.1 years; male: female ratio 11:26). The small sample
size indicates that the present study should be considered as a pilot study.
AX-CPT taskAn Expectancy AX-CPT task (Fig. 1) was programmed in Delpi to run on an
WindowsXP system. Further, the program used “PerformanceCounter” with
which time differences smaller than microseconds can be measured and very
accurate inter-stimuli intervals can be produced. The measurements results of the
program are up to 1 ms precise because it synchronizes stimuli and reaction times
with the viewing screen and because the responses were measured with a special
button box that can pass on a change in the status of the buttons every millisecond.
As in typical AX-CPT tasks, participants were presented with cue probe pairs.
Single letters were consecutively shown in white on a black screen. Participants sat
in front of the response button box and were instructed to respond as quickly and
accurately as possible by giving a target response (press right button on the
button-box) after the probe ‘X’ in combination with the cue ‘A’, or a nontarget
response (press left) after any other combination of letters. Seventy percent were
target trials (Braver et al., 2001) (83 AX trials, 12 AY trials, 12 BX trials and 12 BY
trials). The letters were presented for 350 ms, with a 1200 ms interstimulus
interval. To increase task difficulty, two distracters letters were presented in red
between cue and probe. By increasing task difficulty the number of errors is
higher, and consequently the task could be shortened. This was done in order to
minimize the burden for the participants and increase their compliance to
complete the task correctly.
Following explanation of the task instructions, participants were administered
practice trials. During the practice trials all letter combinations were used.
Participants performed 10 trials. The trial session was repeated until the
participant understood the task and was able to perform the trial session with a
maximum of 1 mistake. Performance during the practice trials was closely
monitored by the examiner and if necessary additional prompting was given so to
ensure full understanding of the task before initiation of the 120 experimental
trials. Participants performed the AX-CPT for 10 min. Response time and error rate
(i.e. pressing the target button where this should have been the non-target button
or vice versa) were recorded.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
98
CHAPTER 5
Statistical analysesFor each subject, mean reaction time (RT) and mean error rate (i.e. percentage of
pressing the target button where this should have been the non-target button or
vice versa) across all trial types were computed (Table 1). Moreover, data were
analyzed separately for the AY and BX trial types. A two way ANOVA (ADHD (two
levels)_BPD (two levels)) was used to examine the effects of disorder on these AX
CPT outcome measurements. F, p, and ηp² values are reported. Data were analyzed
using SPSS version 20. Alpha level was set at.05.
Results
Irrespective of the presence/absence of ADHD, there was a significant main effect
of BPD on overall error rate (F(1,66)=6.935, p=0.011, ηp²=0.064), BX error rate
(F(1,66)=5.288, p=0.025, ηp²=0.074), and RT on BX trials (F(1,66)=4075, p=0.048,
ηp²=0.058). There was one main effect of ADHD on RT on AY trials (F(1,66)=7485,
p=0.008, ηp²=0.102). There were no significant interaction effects found on our
main outcome measurements. However, post-hoc analyses of the AX error rate,
which was very high in the patients with BPD (Table 1), showed significant
interaction effects between ADHD and BPD (F(1,66)=4.518, p=0.037, ηp²=0.064).
Figure 1 AX-CPT task parameters and timing
A E C X A K S G
G K T X L D U T
AX AY
120 Trials: AX-70%, AY 10%, BX 10%, BY 10%.
Instruction: Your target responseis an ‘X’, but only when it follows an ‘A’. Response: press right button - target; press left button - nontarget.
Letters were presented for 350 msec with an 1200 msec interstimulus interval.
BX BY

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
99
RESPONSE INHIBITION IN ADHD AND BPD
5
Discussion
Previous studies indicated behavioral overlap of impulsivity problems between
adult ADHD and BPD. Research focusing on the neurocognitive or neuropsychological
basis of this behavioral overlap is however scarce and contradictory and has not
convincingly established whether or not BPD is related to response inhibition
deficits independently of ADHD. In order to contribute to this question we
examined the effects of ADHD and BPD on AX-CPT outcome. In line with the
behavioral overlap of impulsivity symptoms, we hypothesized that both patients
groups would show impaired response inhibition. Further, we were interested in
whether performance on the specific BX and AY trial types of the AX-CPT is equally
problematic or could pinpoint to differences and a more specific interpretation of
response inhibition problems in our patient groups. In particular, we hypothesized
that BPD is associated with problems in context processing (i.e. reflected in
abnormal scores on BX trials).
The results showed that patients with BPD have the highest overall error rate
in comparison to the other groups. This difference is especially large in the AX
trials. Interestingly, statistical analysis showed that this effect interacts with
ADHD in a way that patients with both BPD and ADHD perform better than the
patients with only BPD. Patients with BPD also performed worse on the BX trials.
Table 1 AX-CPT performance of patients with ADHD, BPD, ADHD and BPD, and healthy controls
ADHD(N=14)
BPD(N=12)
ADHD+ BPD(N=7)
HC(N=37)
Overall Error-rate % (SD) 9.44 (8.66) 16.94 (13.89) 11.58 (9.81) 5.56 (6.83)
AX 9.08 (9.99) 18.91 (18.35) 9.8 (12.36) 4.74 (7.78)
AY 14.29 (14.41) 11.68 (10.51) 14.29 (11.5) 13.36 (13.3)
BX 16.78 (12.75) 20.32 (32.11) 29.77 (33.61) 7.81 (11.49)
BY 0 (0) 4.87 (12.54) 2.38 (6.3) 1.12 (2.89)
Mean RT msec (SD) 426,57 (93,15) 430.05 (132,79) 428.11 (135.36) 343.1 (56.54)
RT AX 419.19(106.67) 419.71 (141.99) 438.09 (142.82) 340.60 (49.93)
RT AY 549.91 (114.7) 447.74 (55.85) 509.32 (122.33) 455.75 (100.5)
RT BX 390.01(170.35) 512.58 (274.8) 396.95 (265.32) 302.63 (140.81)
RT BY 390.11 (133.5) 400.42 (190.74) 309.90 (134.90) 288.13 (95.12)
CPT, continuous performance task; ADHD, attention deficit/hyperactivity disorder; BPD, borderline
personality disorder; HC, healthy controls; RT, reaction time; values are given in means (S.D.).

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
100
CHAPTER 5
They made more errors and were significantly slower than the other participants.
Regarding the error rate we observed an additive effect of BPD and ADHD. Patients
with both disorders made more errors on the BX trials than patients with only
BPD. The ADHD patients showed significantly slow RTs on the AY trials, but this
did not result in a significantly worse error rate.
In sum, patients with BPD performed worse on the overall error rate, BX error
rate and BX RT. In contrast, patients with ADHD performed slow on the AY trials.
Thus, as predicted, both patient groups indeed showed deficiencies in response
inhibition, but these inhibition deficiencies seem more widespread and pervasive
in BPD than in ADHD. In fact, we found only one main effect for ADHD. Moreover,
BPD patients showed response inhibition problems independently of ADHD. The
adults with BPD were particular impaired on the AX and BX trials, whereas the
adults with ADHD seem to have needed significantly more time to perform
adequately on the AY trials.
This finding that patients with BPD performed significantly worse than
patients with ADHD on several indices is somewhat counterintuitive and not in
line with previous work that did not find convincing evidence of response
inhibition deficits in BPD. In fact, previous work reporting on AX-CPT outcome in
BPD patients showed no response inhibitions deficits at all (Hagenhoff et al., 2013).
However, contrary to this previous work, the current study used an expectancy
variant of the AX-CPT, thus favoring impulsive responding and making the task
more demanding.
Another advantage of the used expectancy variant of the AXCPT paradigm is
its potential to produce a double dissociation in performance: individuals with a
context-processing deficit would show impaired performance on BX trials, whereas
those with intact context-processing would perform worse on AY trials (MacDonald,
2008). Thus, with regard to the context-processing theory the higher error rate and
RTs on the BX trials suggest impaired context processing in our BPD patients. In
addition, the increased AX error rate can also be interpreted as a failure to
maintain the A cue until the X probe appeared (Barch et al., 2004). Poor performance
in this condition can arise from problems with maintenance and/or recall of
information from working memory, both aspects of context processing (Bodner et
al., 2012). This interpretation is quite interesting since this is in keeping with
previous work that has identified working memory deficits in BPD (Dinn et al.,
2004; Dowson et al., 2004b).
Further, that BX performance was relatively spared in our ADHD patients
suggests that here context representations were used as a mechanism to inhibit
target responding. This raises questions about the relatively intact maintenance
and/or recall of information from working memory in our ADHD patients.
Although previous studies have mostly confirmed impaired working memory

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
101
RESPONSE INHIBITION IN ADHD AND BPD
5
performance in adults with ADHD (for example: (Dowson et al., 2004b; Boonstra et
al., 2005), it is unclear whether inhibitory control and working memory
impairments represent distinct deficits in ADHD or dual manifestations of a
common pathologic mechanism (i.e. an integral executive phenotype) (Castellanos
and Tannock, 2002). Our results might imply that response inhibition and working
memory are not necessarily two associated processes in adult ADHD. Two previous
studies correlated working memory and response inhibition in adult ADHD
patients with contradictory and unclear results (Clark et al., 2007; Schecklmann et
al., 2012). Future research should therefore examine the relationship between
these core deficits in larger groups of patients with ADHD.
It is also interesting to note that impaired context processing is particularly
demonstrated as a specific impairment in patients with schizophrenia, schizo-
affective disorder and schizotypal personality disorder (McClure et al., 2008),
while other psychiatric disorders like bipolar disorder and major depression have
not exhibited the same impaired context processing (Holmes et al., 2005; Brambilla
et al., 2007). This raises the question of possible shared response inhibition vulner-
abilities between BPD and schizophrenia spectrum disorders. One previous study
focused on this issue and examined whether BPD patients have inhibition deficits,
as measured with an anti-saccade eye task, similar to patients with schizophrenia.
The results suggested that inhibition deficits may be characteristic among BPD
patients with psychotic like symptoms, but do not reflect the whole group of BPD
patients (Grootens et al., 2008a). Of course, we cannot draw any conclusion from
our sample with regard to possible shared response inhibition deficits between
BPD and the schizophrenia spectrum. We lack evidence of severity and frequency
psychotic like symptoms in our BPD patients, nor do we have any evidence that
psychotic like symptoms in BPD and psychotic symptoms in schizophrenia share
the underlying cognitive mechanisms. However, we would like to argue that
because our BPD patients showed clear deficits in context processing and this is
particularly been known to be seen case in schizophrenia spectrum disorders,
psychotic like symptoms should be taken into account in future research on
response inhibition and context processing in BPD. Although the prevalence of
major psychotic disorders is low, transient psychotic like symptoms in response to
stress do occur in about 40% of BPD patients (Zanarini et al., 1990).
The current study included well diagnosed patients and matched controls,
and controlled for the presence of comorbidities and use of medication.
Interpretation of its findings must however be considered in relation to several
methodological limitations. First, the present sample size was small, indicating a
pilot study. This makes it difficult to draw general conclusions about the effects of
ADHD and BPD on cognitive control processes. For this reason, our findings cannot
be generalized to broader groups of patients. Future studies with larger sample

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
102
CHAPTER 5
sizes are needed to confirm the effect of ADHD and BPD on context processing and
response inhibition. Second, our results may not necessarily generalize to patients
with the inattentive type of ADHD who do not have high levels of impulsivity, and
BPD patients without impulsivity. Third, although the sample included men and
females, and participants of different ages, we did not have the power to analyze
gender or age effects. Nor did we control for possible effects of the different
recruitment centers, because of our small sample size.
Some considerations must also be made with regard to use of nicotine and
medication before testing. Participants were not allowed to smoke within 3 h
before measurement. This could have led to some nicotine induced attentional
improvement in both the control and patient groups (Conners et al., 1996). On the
other hand, longer periods of non-smoking prior to testing could cause tension
and anxiety which than could also interfere with the results. Patients using meth-
ylphenidate were not allowed to use it on the day of the experiment. Since the
average half-life of oral methylphenidate is reported to be 2 to 3 h (Wargin et al.,
1983; Volkow et al., 1998), the interruption of one day should be enough to prevent
the pharmacokinetics to be a confounding variable. There is however a risk of
rebound effects that could have had a negative influence on the task performance.
In conclusion, the present study suggests that response inhibition deficits are
related to BPD independently of ADHD. Moreover, contrary to patients with ADHD,
BPD patients may suffer from more widespread inhibition deficiencies and a
specific impairment in context processing. Given the limitations, future research
should attempt to replicate and expand our findings. Understanding the different
cognitive processes that lead to shared clinical symptoms of impulsivity in ADHD
and BPD could lead to more specific treatments.
AcknowledgementsThe authors are grateful to the interns who did assist in collecting data for this
study.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
103
RESPONSE INHIBITION IN ADHD AND BPD
5
References
Andrulonis, P.A., Glueck, B.C., Stroebel, C.F., Vogel, N.G., 1982. Borderline personality subcategories. The
Journal of Nervous and Mental Disease 170, 670–679.
Andrulonis, P.A., Glueck, B.C., Stroebel, C.F., Vogel, N.G., Shapiro, A.L., Aldridge, D.M., 1981. Organic brain
dysfunction and the borderline syndrome. The Psychiatric Clinics of North America 4, 47–66.
Barch, D.M., Mitropoulou, V., Harvey, P.D., New, A.S., Silverman, J.M., Siever, L.J., 2004. Context-processing
deficits in schizotypal personality disorder. Journal of Abnormal Psychology 113, 556–568.
Barkley, R.A., Murphy, K.R., Bush, T., 2001. Time perception and reproduction in young adults with
attention deficit hyperactivity disorder. Neuropsychology 15, 351–360.
Bazanis, E., Rogers, R.D., Dowson, J.H., Taylor, P., Meux, C., Staley, C., Nevinson-Andrews, D., Taylor, C.,
Robbins, T.W., Sahakian, B.J., 2002. Neurocognitive deficits in decision-making and planning of
patients with DSM-III-R borderline personality disorder. Psychological Medicine 32, 1395–1405.
Biederman, J., Petty, C.R., Fried, R., Doyle, A.E., Spencer, T., Seidman, L.J., Gross, L., Poetzl, K., Faraone, S.V.,
2007. Stability of executive function deficits into young adult years: a prospective longitudinal
follow-up study of grown up males with ADHD. Acta Psychiatrica Scandinavica 116, 129–136.
Bodner, K.E., Beversdorf, D.Q., Saklayen, S.S., Christ, S.E., 2012. Noradrenergic moderation of working
memory impairments in adults with autism spectrum disorder. Journal of the International Neuro-
psychological Society 18, 556–564.
Boonstra, A.M., Kooij, J.J., Oosterlaan, J., Sergeant, J.A., Buitelaar, J.K., 2010. To act or not to act, thats the
problem: primarily inhibition difficulties in adult ADHD. Neuropsychology 24, 209–221.
Boonstra, A.M., Oosterlaan, J., Sergeant, J.A., Buitelaar, J.K., 2005. Executive functioning in adult ADHD: a
meta-analytic review. Psychological Medicine 35, 1097–1108.
Brambilla, P., Macdonald 3rd, A.W., Sassi, R.B., Johnson, M.K., Mallinger, A.G., Carter, C.S., Soares, J.C., 2007.
Context processing performance in bipolar disorder patients. Bipolar Disorders 9, 230–237.
Braver, T.S., Barch, D.M., 2002. A theory of cognitive control, aging cognition, and neuromodulation.
Neuroscience and Biobehavioral Reviews 26, 809–817.
Braver, T.S., Barch, D.M., Gray, J.R., Molfese, D.L., Snyder, A., 2001. Anterior cingulate cortex and response
conflict: effects of frequency, inhibition and errors. Cerebral Cortex 11, 825–836.
Braver, T.S., Paxton, J.L., Locke, H.S., Barch, D.M., 2009. Flexible neural mechanisms of cognitive control
within human prefrontal cortex. Proceedings of the National Academy of Sciences of the United
States of America 106, 7351–7356.
Castellanos, F.X., Tannock, R., 2002. Neuroscience of attention-deficit/hyperactivity disorder: the search for
endophenotypes. Nature Reviews. Neuroscience 3, 617–628.
Clark, L., Blackwell, A.D., Aron, A.R., Turner, D.C., Dowson, J., Robbins, T.W., Sahakian, B.J., 2007. Association
between response inhibition and working memory in adult ADHD: a link to right frontal cortex
pathology? Biological Psychiatry 61, 1395–1401.
Cohen, J.D., Barch, D.M., Carter, C., Servan-Schreiber, D., 1999. Context-processing deficits in schizophrenia:
converging evidence from three theoretically motivated cognitive tasks. Journal of Abnormal
Psychology 108, 120–133.
Conners, C.K., 2000. Conners0 Continuous Performance Test II: Computer Program for Windows Technical
Guide and Software Manual. Multi-Health Systems, Toronto, Canada.
Conners, C.K., Levin, E.D., Sparrow, E., Hinton, S.C., Erhardt, D., Meck,W.H., Rose, J.E., March, J., 1996.
Nicotine and attention in adult attention deficit hyperactivity disorder (ADHD). Psychopharmacology
Bulletin 32, 67–73.
de Bruijn, E.R., Grootens, K.P., Verkes, R.J., Buchholz, V., Hummelen, J.W., Hulstijn, W., 2006. Neural
correlates of impulsive responding in borderline personality disorder: ERP evidence for reduced
action monitoring. Journal of Psychiatric Research 40, 428–437.
Dinn, W.M., Harris, C.L., Aycicegi, A., Greene, P.B., Kirkley, S.M., Reilly, C., 2004. Neurocognitive function in
borderline personality disorder. Progress in Neuro-Psychopharmacology & Biological Psychiatry 28,
329–341.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
104
CHAPTER 5
Dowson, J.H., McLean, A., Bazanis, E., Toone, B., Young, S., Robbins, T.W., Sahakian, B., 2004a. The specificity
of clinical characteristics in adults with attentiondeficit/hyperactivity disorder: a comparison with
patients with borderline personality disorder. European Psychiatry 19, 72–78.
Dowson, J.H., McLean, A., Bazanis, E., Toone, B., Young, S., Robbins, T.W., Sahakian, B.J., 2004b. Impaired
spatial working memory in adults with attention-deficit/ hyperactivity disorder: comparisons with
performance in adults with borderline personality disorder and in control subjects. Acta Psychiatrica
Scandinavica 110, 45–54.
DuPaul, GJ, Anastopoulos, P.T., Reid R., AD, 1998. ADHD Rating Scale-IV: Checklists, Norms,and Clinical
Interpretation. The Guilford Press, New York.
Epstein, J.N., Johnson, D.E., Varia, I.M., Conners, C.K., 2001. Neuropsychological assessment of response
inhibition in adults with ADHD. Journal of Clinical and Experimental Neuropsychology 23, 362–371.
Evenden, J.L., 1999. Varieties of impulsivity. Psychopharmacology 146, 348–361.
Faraone, S.V., Biederman, J., Doyle, A., Murray, K., Petty, C., Adamson, J.J., Seidman, L., 2006. Neuropsycho-
logical studies of late onset and subthreshold diagnoses of adult attention-deficit/hyperactivity
disorder. Biological Psychiatry 60, 1081–1087.
Ferrer, M., Andion, O., Matali, J., Valero, S., Navarro, J.A., Ramos-Quiroga, J.A., Torrubia, R., Casas, M., 2010.
Comorbid attention-deficit/hyperactivity disorder in borderline patients defines an impulsive
subtype of borderline personality disorder. Journal of Personality Disorders 24, 812–822.
Fischer, M., Barkley, R.A., Smallish, L., Fletcher, K., 2005. Executive functioning in hyperactive children as
young adults: attention, inhibition, response perseveration, and the impact of comorbidity.
Developmental Neuropsychology 27, 107–133.
Fossati, A., Novella, L., Donati, D., Donini, M., Maffei, C., 2002. History of childhood attention deficit/
hyperactivity disorder symptoms and borderline personality disorder: a controlled study.
Comprehensive Psychiatry 43, 369–377.
Groenestijn, M.A.C., Akkerhuis, G.W., Kupka, R.W., Schneider, N., Nolen, W.A., 1999. Structured Clinical
Interview for DSM-IV Axis I Disorders. Swets & Zeitlinger BV, Lisse, the Netherlands.
Grootens, K.P., van Luijtelaar, G., Buitelaar, J.K., van der Laan, A., Hummelen, J.W., Verkes, R.J., 2008a.
Inhibition errors in borderline personality disorder with psychotic-like symptoms. Progress in Neu-
ro-Psychopharmacology & Biological Psychiatry 32, 267–273.
Grootens, K.P., van Luijtelaar, G., Miller, C.A., Smits, T., Hummelen, J.W., Buitelaar, J.K., Verkes, R.J., 2008b.
Increased p50 gating but intact prepulse inhibition in borderline personality disorder. The Journal of
Neuropsychiatry and Clinical Neurosciences 20, 348–356.
Hagenhoff, M., Franzen, N., Koppe, G., Baer, N., Scheibel, N., Sammer, G., Gallhofer, B., Lis, S., 2013. Executive
functions in borderline personality disorder. Psychiatry Research 210, 224–231.
Hervey, A.S., Epstein, J.N., Curry, J.F., 2004. Neuropsychology of adults with attention- deficit/hyperactivity
disorder: a meta-analytic review. Neuropsychology, 18, 485–503.
Holmes, A.J., MacDonald 3rd, A., Carter, C.S., Barch, D.M., Andrew Stenger, V., Cohen, J.D., 2005. Prefrontal
functioning during context processing in schizophrenia and major depression: an event-related fMRI
study. Schizophrenia Research 76, 199–206.
Kooij, J.J., 2002. ADHD bij Volwassenen. Inleiding in de Diagnostiek en Behandeling [ADHD in Adults.
Introduction in Diagnostics and Treatment]. Swets & Zeitlinger BV, Lisse, the Netherlands.
Kooij, J.J., Aeckerlin, L.P., Buitelaar, J.K., 2001. Functioning, comorbidity and treatment of 141 adults with
attention deficit hyperactivity disorder (ADHD) at a psychiatric outpatient department. Nederlands
Tijdscrift Voor Geneeskunde, 145, 1498–1501.
Kooij, J.J., Buitelaar, J.K., van den Oord, E.J., Furer, J.W., Rijnders, C.A., Hodiamont, P.P., 2005. Internal and
external validity of attention-deficit hyperactivity disorder in a population-based sample of adults.
Psychological Medicine 35, 817–827.
Krause-Utz, A., Sobanski, E., Alm, B., Valerius, G., Kleindienst, N., Bohus, M., Schmahl, C., 2013. Impulsivity
in relation to stress in patients with borderline personality disorder with and without co-occurring
attention-deficit/hyperactivity disorder: an exploratory study. The Journal of Nervous and Mental
Disease 201, 116–123.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
105
RESPONSE INHIBITION IN ADHD AND BPD
5
Lampe, K., Konrad, K., Kroener, S., Fast, K., Kunert, H.J., Herpertz, S.C., 2007. Neuropsychological and
behavioural disinhibition in adult ADHD compared to
borderline personality disorder. Psychological Medicine 37, 1717–1729.
Lawrence, K.A., Allen, J.S., Chanen, A.M., 2010. Impulsivity in borderline personality disorder: reward-based
decision-making and its relationship to emotional distress. Journal of Personality disorders 24,
786–799.
Leyton, M., Okazawa, H., Diksic, M., Paris, J., Rosa, P., Mzengeza, S., Young, S.N., Blier, P., Benkelfat, C., 2001.
Brain Regional alpha-[11C]methyl-L-tryptophan trapping in impulsive subjects with borderline
personality disorder. The American Journal of Psychiatry 158, 775–782.
MacDonald 3rd, A.W., 2008. Building a clinically relevant cognitive task: case study of the AX paradigm.
Schizophrenia Bulletin 34, 619–628.
McCloskey, M.S., New, A.S., Siever, L.J., Goodman, M., Koenigsberg, H.W., Flory, J.D., Coccaro, E.F., 2009.
Evaluation of behavioral impulsivity and aggression tasks as endophenotypes for borderline
personality disorder. Journal of Psychiatric, Research 43, 1036–1048.
McClure, M.M., Barch, D.M., Flory, J.D., Harvey, P.D., Siever, L.J., 2008. Context processing in schizotypal
personality disorder: evidence of specificity of impairment to the schizophrenia spectrum. Journal of
Abnormal Psychology, 117, 342–354.
Murphy, K.R., Barkley, R.A., Bush, T., 2001. Executive functioning and olfactory identification in young
adults with attention deficit-hyperactivity disorder. Neuropsychology 15, 211–220.
Nigg, J.T., Silk, K.R., Stavro, G., Miller, T., 2005a. Disinhibition and borderline personality disorder.
Development and Psychopathology 17, 1129–1149.
Nigg, J.T., Stavro, G., Ettenhofer, M., Hambrick, D.Z., Miller, T., Henderson, J.M., 2005b. Executive functions
and ADHD in adults: evidence for selective effects on ADHD symptom domains. Journal of Abnormal
Psychology 114, 706–717.
Nigg, J.T., Willcutt, E.G., Doyle, A.E., Sonuga-Barke, E.J., 2005c. Causal heterogeneity in attention-deficit/
hyperactivity disorder: do we need neuropsychologically impaired subtypes? Biological Psychiatry
57, 1224–1230.
Philipsen, A., Limberger, M.F., Lieb, K., Feige, B., Kleindienst, N., Ebner-Priemer, U., Barth, J., Schmahl, C.,
Bohus, M., 2008. Attention-deficit hyperactivity disorder as a potentially aggravating factor in
borderline personality disorder. The British Journal of Psychiatry 192, 118–123.
Rentrop, M., Backenstrass, M., Jaentsch, B., Kaiser, S., Roth, A., Unger, J., Weisbrod, M., Renneberg, B., 2008.
Response inhibition in borderline personality disorder: performance in a Go/Nogo task. Psychopa-
thology 41, 50–57.
Rey, J.M., Morris-Yates, A., Singh, M., Andrews, G., Stewart, G.W., 1995. Continuities between psychiatric
disorders in adolescents and personality disorders in young adults. The American Journal of
Psychiatry 152, 895–900.
Riccio, C.A., Reynolds, C.R., 2001. Continuous performance tests are sensitive to ADHD in adults but lack
specificity. A review and critique for differential diagnosis. Annals of the New York Academy of
Sciences 931, 113–139.
Riccio, C.A., Reynolds, C.R., Lowe, P., Moore, J.J., 2002. The continuous performance test: a window on the
neural substrates for attention? Archives of Clinical Neuropsychology: The Official Journal of the
National Academy of Neuropsychologists 17, 235–272.
Ross, R.G., Harris, J.G., Olincy, A., Radant, A., 2000. Eye movement task measures inhibition and spatial
working memory in adults with schizophrenia, ADHD, and a normal comparison group. Psychiatry
Research 95, 35–42.
Rosvold, H.E., Delgado, J.M., 1956. The effect on delayed-alternation test performance of stimulating or
destroying electrically structures within the frontal lobes of the monkeys brain. Journal of
Comparative and Physiological Psychology 49, 365–372.
Rubio, G., Jimenez, M., Rodriguez-Jimenez, R., Martinez, I., Iribarren, M.M., Jimenez-Arriero, M.A., Ponce,
G., Avila, C., 2007. Varieties of impulsivity in males with alcohol dependence: the role of Cluster-B
personality disorder. Alcoholism, Clinical and Experimental Research 31, 1826–1832.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
106
CHAPTER 5
Ruocco, A.C., Laporte, L., Russell, J., Guttman, H., Paris, J., 2012. Response inhibition deficits in unaffected
first-degree relatives of patients with borderline personality disorder. Neuropsychology 26, 473–482.
Schecklmann, M., Ehlis, A.C., Plichta, M.M., Dresler, T., Heine, M., Boreatti-Hummer, A., Romanos, M., Jacob,
C., Pauli, P., Fallgatter, A.J., 2012. Working memory and response inhibition as one integral phenotype
of adult ADHD? A behavioral and imaging correlational investigation, Journal of Attention Disorders.
Schoechlin, C., Engel, R.R., 2005. Neuropsychological performance in adult attention-deficit hyperactivity
disorder: meta-analysis of empirical data. Archives of Clinical Neuropsychology 20, 727–744.
Seidman, L.J., Doyle, A., Fried, R., Valera, E., Crum, K., Matthews, L., 2004. Neuropsychological function in
adults with attention-deficit/hyperactivity disorder. The Psychiatric Clinics of North America 27,
261–282.
Servan-Schreiber, D., Cohen, J.D., Steingard, S., 1996. Schizophrenic deficits in the processing of context.
A test of a theoretical model. Archives of General Psychiatry 53, 1105–1112.
Sheehan, D.V., Lecrubier, Y., Sheehan, K.H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., Dunbar,
G.C., 1998. The mini-international neuropsychiatric Interview (M.I.N.I.): the development and
validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of
Clinical Psychiatry 59 (Suppl. 20), 22–33. (quiz 34-57).
Sonuga-Barke, E., Bitsakou, P., Thompson, M., 2010. Beyond the dual pathway model: evidence for the
dissociation of timing, inhibitory, and delay-related impairments in attention-deficit/hyperactivity
disorder. Journal of the American Academy of Child and Adolescent Psychiatry 49, 345–355.
Stavro, G.M., Ettenhofer, M.L., Nigg, J.T., 2007. Executive functions and adaptive functioning in young adult
attention-deficit/hyperactivity disorder. Journal of the International Neuropsychological Society 13,
324–334.
van Dijk, F., Lappenschaar, M., Kan, C., Verkes, R.J., Buitelaar, J., 2011. Lifespan attention deficit/hyperactivity
disorder and borderline personality disorder symptoms in female patients: a latent class approach.
Psychiatry Research, 190, 327–334.
van Dijk, F.E., Lappenschaar, M., Kan, C.C., Verkes, R.J., Buitelaar, J.K., 2012. Symptomatic overlap between
attention-deficit/hyperactivity disorder and borderline personality disorder in women: the role of
temperament and character traits. Comprehensive Psychiatry 53, 39–47.
Volker, K.A., Spitzer, C., Limberg, A., Grabe, H.J., Freyberger, H.J., Barnow, S., 2009. Executive dysfunctions
in female patients with borderline personality disorder with regard to impulsiveness and depression.
Psychotherapie, Psychosomatik, Medizinische Psychologie 59, 264–272.
Volkow, N.D., Wang, G.J., Fowler, J.S., Gatley, S.J., Logan, J., Ding, Y.S., Hitzemann, R., Pappas, N., 1998.
Dopamine transporter occupancies in the human brain induced by therapeutic doses of oral methyl-
phenidate. The American Journal of Psychiatry 155, 1325–1331.
Weertman, A., Arntz, A., Kerkhofs, M.L.M., 2000. Structured Clinical Interview for DSM-IV Axis II
Personality Disorders. Swets & Zeitliner BV, Lisse, the Netherlands.
Wargin, W., Patrick, K., Kilts, C., Gualtieri, C.T., Ellington, K., Mueller, R.A., Kraemer, G., Breese, G.R., 1983.
Pharmacokinetics of methylphenidate in man, rat and monkey. Journal of Pharmacology and
Experimental Therapeutics 226, 382–386.
Woods, S.P., Lovejoy, D.W., Ball, J.D., 2002. Neuropsychological characteristics of adults with ADHD: a
comprehensive review of initial studies. The Clinical Neuropsychologist 16, 12–34.
Zanarini, M.C., Gunderson, J.G., Frankenburg, F.R., 1990. Cognitive features of borderline personality
disorder. The American Journal of Psychiatry 147, 57–63

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
107
RESPONSE INHIBITION IN ADHD AND BPD
5

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Under review as:
Van Dijk FE, Mostert, Onnink, Dammers, Arias Vasquez, Kan, Verkes, Hoogman,
Franke, Buitelaar. (2016). Five Factor Model personality traits relate to adult attention-
deficit/hyperactivity disorder but not to their distinct neurocognitive profiles.
Five Factor Model personality traits relate to adult attention-deficit/
hyperactivity disorder but not to their distinct neurocognitive profiles
6

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
110
CHAPTER 6
Abstract
Objective: To investigate whether personality traits are related to neurocognitive
profiles in adults with ADHD.
Method: Neuropsychological performance and Five Factor Model (FFM) personality
traits were measured in adults with ADHD (n= 133) and healthy controls (n= 132).
Three neuropsychological profiles, derived from previous community detection
analyses, were investigated for personality trait differences.
Results: Irrespective of cognitive profile, participants with ADHD showed
significantly higher Neuroticism and lower Extraversion, Agreeableness, and Con-
scientiousness than healthy controls. Only the FFM personality factor Openness
differed significantly between the three profiles. Higher Openness was more
common in those with aberrant attention and inhibition than those with increased
delay discounting and atypical working memory / verbal fluency.
Conclusion: The results suggest that the personality trait Openness, but not any
other FFM factor, is linked to neurocognitive profiles in ADHD. ADHD symptoms
rather than profiles of cognitive impairment may have a determining influence on
personality trait outcome.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
111
FFM TRAITS RELATE TO ADHD BUT NOT TO THEIR COGNITIVE PROFILES
6
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a common neuropsychiatric
disorder that is characterized by symptoms of inattention, hyperactivity, and
impulsivity. ADHD often persists into adulthood (Faraone 2015). Current research
does not support a single core (neuro)cognitive deficit of ADHD, but rather
demonstrate that both childhood and adult ADHD are characterized by strong
heterogeneity in cognitive underperformance with multiple cognitive pathways
(Sonuga-Barke, Bitsakou et al. 2010; de Zeeuw, Weusten et al. 2012; Fair, Bathula et
al. 2012; Coghill, Seth et al. 2014; Mostert, Onnink et al. 2015). The main domains
of neuropsychological dysfunction in ADHD are: memory, inhibitory control,
delay aversion, decision making, timing, and response variability. The levels of
deficiency in each of these domains differ more or less independently within
patients with ADHD, and there is considerable overlap between neuropsychologi-
cal performance in patients with ADHD and normal controls (Coghill, Seth et al.
2014). Use of multivariate classification techniques has led to the identification of
subgroups of individuals with ADHD based on a similar neurocognitive profile,
both in children and in adults (Fair, Bathula et al. 2012; Mostert, Hoogman et al.
2015; van Hulst, de Zeeuw et al. 2015). Such results provide some structure to the
heterogeneity in ADHD. However the clinical utility of subgrouping based on neu-
ropsychological characteristics in ADHD needs to be explored.
Contributing to the heterogeneity of ADHD is the presence of temperament
and personality traits. Temperament traits can be described as a set of biologically
based behavioural and emotional tendencies covering negative and positive
emotion systems as well as attentional capacities (Rothbart 2011). A recent study
used the technique of ‘community detection’ to cluster children with ADHD into
subgroups based on temperament dimensions of the Temperament in Middle
Childhood Questionnaire. The results suggested three novel types of ADHD that
were independent of existing clinical demarcations, including DSM-5 presentations
(Karalunas, Fair et al. 2014). Type 1, the mild type, had milder impulsivity, inhibition,
and attentional control impairments compared with the other two ADHD types.
Type 2, the surgent type, had increased impulsivity, activity levels and assertiveness,
decreased shyness coupled to high intensity pleasure seeking than the other two
types. Type 3, the irritable type, had increased impulsivity and attentional control
impairments than type 1 and increased negative emotionality compared to the
other two types. Personality research in general has mostly used the Five Factor
Model (FFM) (Costa and McCrae 1992) as a well-supported organizing framework
that has been characterized with respect to underlying temperament dimensions
(i.e. the initial state of emotional, motor, and attentional reactivity from which
personality develops in interaction with experience) (Rothbart 2007). A recent

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
112
CHAPTER 6
review of findings on ADHD and FFM personality suggests that, in general, ADHD
has associations with the FFM traits of Neuroticism (positive), Agreeableness
(negative) and Conscientiousness (negative). Mixed findings (positive, negative, and
no associations) have been reported for Extraversion and Openness (Gomez and
Corr 2014).
Prior research, mostly assessing the relationship between single tasks or facets
of executive function and single FFM traits in healthy participants, suggests that
significant associations also exist between FFM traits and neurocognitive
functioning, especially executive functioning (for an overview, see (Williams,
Suchy et al. 2009)). Three more recent studies extended that early research by
considering all five FFM traits in relation to a more fully characterized domain of
executive functioning. A first study among 58 healthy older adults investigated
four tests assessing all core aspects of executive functioning (cognitive flexibility,
initiation, inhibition, response selection, working memory, generative fluency,
and attentional vigilance) (Williams, Suchy et al. 2010). The results showed that
the executive functioning factor, that emerged from four executive functioning
scores (one for each executive functioning test), was negatively correlated with
Neuroticism and positively with Openness and Agreeableness. But although high
Neuroticism was associated with poorer executive functioning, both the middle
and high executive functioning groups were in the average range for Neuroticism
(compared to normative values). Individuals with better executive functioning
were characterized by high Openness and Agreeableness and average levels of
Neuroticism. Executive functioning was not associated with Extraversion or
Conscientiousness in this study.
A second study, including 182 students, examined three separate core executive
function factors (i.e. inhibition, updating/monitoring information in working
memory, and cognitive flexibility) as predictors of the five FFM traits (Murdock,
Oddi et al. 2013). Higher Neuroticism and lower Openness were associated with
poor updating/monitoring, and Openness was positively associated with cognitive
flexibility (the ability to shift one’s attention between multiple tasks or mental
sets). The authors suggested that Neuroticism and Openness may share some
common underlying cognitive mechanism, in particular working memory.
Connections between executive functioning and Extraversion, Agreeableness, and
Conscientiousness did not emerge in this study.
A third study examined associations between FFM traits and cognitive
performance to 1) uncover the specific facets of each trait that are most closely
related to cognition, and 2) examine, how these associations may vary by age in
154 healthy older and younger adults. The cognitive domains measured were
processing speed, reaction time, verbal fluency, inductive reasoning, and working
and episodic memory. Neuroticism (trait) and in particular ‘depression’ (a facet of

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
113
FFM TRAITS RELATE TO ADHD BUT NOT TO THEIR COGNITIVE PROFILES
6
Neuroticism) were negatively associated with performance on cognitive tasks that
require effortful processing. The results suggested that individuals, who are more
angry and depressed, have slower processing speed and lower reasoning scores.
Openness (trait) and ‘ideas’ (a facet of openness) were positively associated with
verbal fluency, indicating that ‘ideas’ may be a key characteristic in the association
between Openness and cognition. Those open to ideas are likely to spend more
time exploring intellectual pursuits, which could translate into a greater facility
with words. Extraversion (trait) and ‘assertiveness’ (a facet of Extraversion) were
negatively related to reasoning and reaction time, indicating that extraverted
individuals may be faster, but are less likely to take time to think thoroughly
about a task. The FFM traits and their facets did not predict working memory or
episodic memory in this study. The association between Neuroticism and cognitive
performance was found primarily among younger adults. In older adulthood,
better performance was associated with positive aspects of personality (Graham
and Lachman 2014).
So far, the studies of cognitive performance and personality did not take the
presence of psychopathology into account. In the present study, we follow-up on
this previous work regarding the subtyping of ADHD by cognition and
temperament. Specifically, we examined, whether adults with ADHD and healthy
controls, who share similar neurocognitive profiles, also share specific personality
traits, or, alternatively, whether ADHD is related to personality irrespective of a
specific neurocognitive profile. To this end, we built on our earlier work, in which
we had identified by community detection analysis three subgroups of patients
and healthy controls based on cognitive profiles characterized by (1) poor
performance on attention and inhibition, (2) high scores for impulsive behaviour
on the delay-discounting task (delay aversion), (3) impairment on working memory
and verbal fluency (Mostert, Hoogman et al. 2015). Given the recent evidence for
the relationship between executive functions and FFM trait outcome as outlined
above, we anticipated that our previously identified profiles 1 and 3 would be
associated with higher Neuroticism and lower Openness. Further, in keeping with
previously found associations between Extraversion and higher delayed
discounting rates (Hirsh, Morisano et al. 2008), we also anticipated that Extraversion
would be positively related to our cognitive profile 2. Alternatively, if it would be
the ADHD symptoms that accounted for FFM trait outcome rather than the
cognitive profiles, we expected to find associations of the FFM traits with diagnostic
group, irrespective of cognitive profile membership. Such associations could be
expected for Neuroticism, Conscientiousness, and Agreeableness. The results can
add to the understanding of the associations between FFM traits and executive
functioning, in particular in an adult ADHD population.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
114
CHAPTER 6
Methods
Participants A total of 265 participants (133 adults with ADHD and 132 healthy controls)
between 18 and 65 years old were included in this study. All participants were part
of the Dutch node of the International Multicentre persistent ADHD Collaboration
(IMpACT - 6 http://impactadhdgenomics.com (Franke, Vasquez et al. 2010)).
Participants had been recruited from the Department of Psychiatry of the Radboud
University Medical Center (RadboudUMC) in Nijmegen and through advertisements.
Patients were included if they had previously been diagnosed with adult ADHD
by a psychiatrist according to the Diagnostic and Statistical Manual of Mental
Disorders (4th edition; DSM-IV-TR; American Psychiatric Association, 2000).
Exclusion criteria were psychosis, alcohol, or substance addiction in the last six
months, current major depression, full-scale IQ estimate < 70 (assessed using the
Wechsler Adult Intelligence Scale-III), neurological disorders, sensorimotor
disabilities, non-Caucasian ethnicity, and medication use other than psychostimu-
lants, atomoxetine, or bupropion. Additional exclusion criteria for healthy
participants were a current or lifetime neurological or psychiatric disorder in
either the participant or his/her first-degree relatives.
Ethical standards This study was approved by the regional ethics committee (Centrale Commissie
Mensgebonden Onderzoek: CMO Regio Arnhem – Nijmegen; Protocol number
III.04.0403). Written informed consent was obtained from all participants. The
authors assert that all procedures contributing to this work complied with the
ethical standards of the relevant national and international and institutional
committees on human experimentation and with the Helsinki Declaration of
1975, as revised in 2008.
Psychiatric assessment Both patients and controls were assessed using the structured diagnostic interview
for adult ADHD (DIVA 2.0.; www.divacenter.eu (Kooij 2010)). This interview focuses
on the 18 DSM-IV symptoms of ADHD and uses concrete and realistic examples to
thoroughly investigate whether a symptom is currently present or was present in
childhood. Additionally, a self-report questionnaire on current symptoms was
obtained using the ADHD Rating Scale-IV (Kooij, Buitelaar et al. 2005). Lifetime
DSM IV axis I and II disorders were assessed with the Structured Clinical Interview
for DSM disorders I and II (SCID I and SCID II) (Groenestijn, Akkerhuis et al. 1999;
Weertman, Arntz et al. 2000). With regard to the Axis II personality disorders,
participants first filled out the SCID II self-report questionnaire, and when

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
115
FFM TRAITS RELATE TO ADHD BUT NOT TO THEIR COGNITIVE PROFILES
6
applicable, according to the SCID II manual, the clinical interview followed.
Further measurements included an MRI scanning session and blood withdrawal for
DNA analysis. These data are described elsewhere and are not part of the current
analyses (Franke, Hoogman et al. 2008; Franke, Vasquez et al. 2010; Hoogman,
Aarts et al. 2011; Hoogman, Onnink et al. 2013; Onnink, Zwiers et al. 2014).
Neuropsychological testing batteryNeuropsychological performance was measured using a test battery that included
measures tapping into executive functioning (working memory, attention,
inhibition, set-shifting, fluency) and delay discounting, deficits of which have been
earlier reported in ADHD. Details about tasks and main outcome measures are
described in Supplementary Table 1 and our previous reports (Mostert, Hoogman
et al. 2015; Mostert, Onnink et al. 2015). The tests were always administered in the
same order. In total, 21 variables in seven tasks were analysed. Outliers were
defined as having a score higher than four times the standard deviation above or
below the mean per group (Leth-Steensen, Elbaz et al. 2000; Nigg, Stavro et al. 2005).
This threshold guarded against artefacts, while still including cases performing
at the extreme of the normal distribution (i.e., including low performing cases
that might have more severe ADHD symptoms). If a participant’s score was an
outlier on one outcome variable of a task, his/her scores on all outcome variables
from that task were excluded. All data was transformed in such a way that higher
values indicated worse performance. To estimate IQ, subtests of the Wechsler Adult
Intelligence Scale (WAIS) were administered (vocabulary and block design)
(Wechsler 1997).
Neurocognitive profiles In our previous report, Confirmatory Factor Analysis (CFA) was used to reduce
neurocognitive data to six cognitive factors: reaction time and variability,
delay discounting, verbal fluency, working memory, attention and inhibition.
Subsequently, factor scores were correlated across subjects to form networks.
Further, a community detection algorithm was used to cluster these networks into
subgroups. The ADHD and the control group each separated into three profiles
that differed in cognitive performance. Profile 1 was characterized by aberrant
attention and inhibition, profile 2 by increased delay discounting, and profile 3
by atypical working memory and verbal fluency. The same profiles were observed
in the control and ADHD sample. Details about the method, sample sizes, results
are described in (Mostert, Hoogman et al. 2015).

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
116
CHAPTER 6
Five Factor Model Personality Measurement The participants completed the NEO-FFI (Costa and McCrae 1992), a 60 item self-
report assessing each of the 5 FFM personality domains: Extraversion, Agreeableness,
Conscientiousness, Neuroticism, and Openness to experiences. Each domain
includes 12 items. The NEO-FFI was not intended to provide definitive measurement
of the five personality factors, but was designed as a brief instrument that would
yield reasonable estimates of the factors, useful in exploratory research. In over a
decade of use, it has shown itself to be reliable, valid, and useful in a variety of
contexts and cultures (McCrae and Costa 2004). Extraversion reflects being
sociable, outgoing, optimistic, sensation seeking, and talkativeness. Agreeableness
refers to the tendency to be agreeable, trustworthy, friendly, and cooperative with
others, rather than suspicious and antagonistic towards others. It is also a measure
of whether a person is generally well tempered or not. Conscientiousness reflects
a person’s tendency to be well organized, responsible, and task-focused in pursuing
goals. Neuroticism indicates the tendency for proneness to unpleasant experience,
such as anger, anxiety, depression, and maladjustment. Neuroticism also refers to
the degree of emotional stability and impulse control and is sometimes referred to
by its low pole, “emotional stability”. Openness to experience reflects a person’s
tendency for being imaginative, creative, and interested in cultural and educational
experiences.
Statistical analysis In the current study, we tested for FFM trait differences between the three
neurocognitive profiles using analysis of variance (ANOVA). For this, a two (group:
ADHD vs. Control) by three (the cognitive profiles: inattention and inhibition
[profile 1] vs. delay aversion [profile 2] vs. working memory and verbal fluency
[profile 3]) ANOVA was performed on the scores of each of the five factors of the
FFM, with group and cognitive profile as between-subject factors and the FFM
factors as dependent variables. These calculations were done using SPSS (version
20; SPSS, Chicago, IL).
Results
Demographics of the sample are described in Table 1. Adults with ADHD and
healthy controls did not differ in age , gender, or IQ, but controls had a higher level
of education. Table 2 presents the scores (mean and SD) of all six groups analysed
in the ANOVA on all factors of the FFM.
The analyses of the Neuroticism scale did not reveal a main effect of cognitive
profile (F(2, 246) = 0.26, p = .77), but a main effect of diagnostic status was observed,

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
117
FFM TRAITS RELATE TO ADHD BUT NOT TO THEIR COGNITIVE PROFILES
6
with a significantly higher score on Neuroticism for the ADHD than the control
group (F(1, 246) = 124.09, p = .0001). Furthermore, the interaction effect of group
and cognitive profile was significant (F(2, 246) = 4.25, p = .02). Using a one-way
ANOVA to localize this effect revealed no significant differences between any of
the profile groups for the ADHD-group (F(2, 121) = 1.18, p = .31), whereas the same
analysis on the control group yielded a significant effect, F(2, 125) = 3.50, p = .03.
Within the ADHD group profile 1 had the highest average score on Neuroticism,
whereas in the control group profile 1 was associated with the lowest score on
Neuroticism. However, these findings did not survive Bonferroni correction. 9
On the Extraversion scale a main effect of group was found (F(1, 247) = 7.76,
p = .006) with significantly higher scores for the healthy control group. There was
no main effect for cognitive profile (F(2, 247) = 2.03, p = .13), nor was a significant
Table 1 Demographics of the participants
ADHD patients(N=133)
Healthy controls(N=132) Statistics
Gender M/F 56/77 53/79 χ² (1, N = 265) = 0.10, p = .75
Age Mean (SD) 35.56 (10.40) 36.30 (11.75) t(258,7) = 0.54, p = .59
IQ1 Mean (SD) 107.84 (14.34) 109.97 (14.90) t(263) = 1.19, p = .24
Education2 Mean (SD) 4.70 (0.80) 5.16 (0.81) t(263) = 4.66, p < 0.001
1 Estimated IQ based on performance on the WAIS-III block pattern and vocabulary tasks.2 Education levels were coded from 1 (unfinished primary school) to 7 (post-university).
Because Levene’s test for equality of variances was significant in the t test for the differences in ages,
degrees of freedom were adjusted accordingly.
Table 2 Outcome of Five Factor Model traits for the ADHD and healthy control groups in Profile 1, 2, and 3
Profile 1 (N=98; 53% ADHD)
Profile 2 (N=62; 50% ADHD)
Profile 3 (N=105; 48% ADHD)
ADHD (SD) HC (SD) ADHD (SD) HC (SD) ADHD (SD) HC (SD)
Neuroticism 39.8 (8.9) 24.0 (7.1) 36.9 (9.8) 28.3 (10.1) 38 (6.8) 27.4 (6.7)
Extraversion 41.7 (7.4) 44.6 (6.2) 40.1 (6.7) 42.1 (6.5) 40.9 (6.7) 42.9 (4.5)
Openness 43.6 (6.1) 41.6 (4.8) 38.4 (6.8) 39.5 (5.1) 41 (5.4) 38.9 (5.5)
Agreeableness 42.8 (5.7) 46.2 (6.2) 40.7 (6.7) 46.2 (5.4) 43.6 (5.4) 46.7 (4.5)
Conscientiousness 34 (6.4) 44.9 (6.5) 35.2 (6.2) 45.9 (5.3) 34.5 (6.5) 46.4 (4.4)
Profile 1: poor performance on attention and inhibition; Profile 2: high scores for impulsive behaviour
on the delay-discounting task (delay aversion); Profile 3: impairment on working memory and verbal
fluency. HC= healthy control.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
118
CHAPTER 6
interaction effect of group and cognitive profile observed (F(2, 247) = 0.15, p = .87).
The analysis of the Openness scale revealed a main effect of cognitive profile
(F(2, 247) = 9.10, p = .0001), showing that the participants in profile 1 scored
significantly higher than the participants in profile 2 and profile 3. Effects of
group and the interaction of group with cognitive profile were non-significant
(F(1, 247) = 1.92, p = .17; F(2, 247) = 1.76, p = .17).
On the Agreeableness scale, a significant main effect for group was found,
with significantly higher Agreeableness scores for the healthy controls (F(1, 247) =
30.68, p = .0001). No effects of cognitive profile (F(2, 247) = 1.71, p = .18) or the
interaction of group and cognitive profile (F(2, 247) = 0.95, p = .39) were observed.
Lastly, there was a significant main effect for group on the Conscientiousness
scale, with significantly higher scores for the healthy controls compared to the
ADHD patients (F(1, 247) = 214.50, p = .0001). There was no significant main effect
for cognitive profile (F(2, 247) = 0.89, p = .41), and no interaction effect of group and
cognitive profile were observed (F(2, 247) = 0.23, p = .80).
Discussion
The present research investigated, whether FFM traits are significantly related to
neurocognitive profiles in adults with ADHD and controls or are related to ADHD
irrespective of a specific neurocognitive profile. Our main findings are: 1) that
there is no particular relationship between personality traits and cognitive
profiles for most FFM traits; 2) that a relationship between Openness to experience
and inattention / disinhibition is observed; 3) that we can confirm a relationship
between ADHD and personality traits.
Irrespective of cognitive profile, participants with ADHD were found to have
higher scores for Neuroticism and lower scores for Extraversion, Agreeableness,
and Conscientiousness than healthy controls. Cognitive profile was significantly
related to Openness, which was higher in participants with profile 1 (inattention
and disinhibition) than in participants with one of the other two cognitive profiles
(2 (delay aversion / impulsivity) and 3 (working memory / verbal fluency) in both
ADHD patients and controls. No additional associations between FFM measures
and cognitive profiles were found. Previously, it has been proposed that ADHD
originates from a primary cognitive deficit in a specific executive functioning (EF)
domain such as response inhibition or working memory or a more general
weakness in executive control (Pennington and Ozonoff 1996; Barkley 1997;
Schachar, Mota et al. 2000; Castellanos and Tannock 2002). The current study
demonstrates that personality and cognitive performance are mainly separate
domains that apparently do not share similar etiological factors or underlying

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
119
FFM TRAITS RELATE TO ADHD BUT NOT TO THEIR COGNITIVE PROFILES
6
mechanisms in adult ADHD. Our study also documents that personality may be
more closely related to clinical symptoms than the cognitive profiles. Treating the
cognitive domains may therefore not necessarily be the most useful therapeutic
approach in ADHD. However, the cognitive profiles may be more closely related
to functional impairments (Mostert, Hoogman et al. 2015). In any case, it seems
important to look at other factors such as personality beyond cognition in considering
what are the most clinically useful options for patient management. Although
this aspect was outside the scope of the current study, it would be useful to know
if patient stratification on personality profile could inform treatment response.
With regard to the relationship between personality and cognitive domains in
ADHD, we only found a higher score on openness to experiences in participants
with cognitive profile 1 (poor performance on attention and inhibition) than in
participants with profiles 2 and 3. Individuals high in openness tend to be
unconventional, explorative, and interested in novelty. This would suggest that
openness is associated with active and impulsive behaviour. Indeed, this would
suggest that disinhibition may underlie openness. This relationship has been
observed before by DeYoung and coworkers, and indeed in that study the authors
controlled for cognitive abilities in order to reveal an association of openness with
externalizing behaviour (i.e. aggression, opposition, and hyperactivity) (Deyoung,
Peterson et al. 2008). In that case, the variance in openness was related to the meta-
trait plasticity (i.e. the shared variance of Extraversion and Openness appearing to
reflect the tendency to explore both behaviourally and cognitive). Plasticity was
positively associated with externalizing behaviour, whereas variance due to
cognitive ability was negatively associated with such behaviour. In other words,
the findings of that study indicated that if one examines individuals equal in the
meta-trait stability (i.e. the shared variance of Neuroticism reversed, Conscientious-
ness, and Agreeableness) and cognitive ability, those higher in plasticity are likely
to show higher levels of externalizing behaviour. In our current study, this may
underline the relatively higher Openness outcome in profile 1, since it is characterized
by inhibition deficits (as measured by a go/no go task). Interestingly, when the
number of self-reported hyperactivity/impulsivity symptoms was examined in our
previous study defining the cognitive profiles, those symptoms were shown to be
unequally distributed across the three cognitive profiles: The patients in profile 1
(and 2) had indeed significantly more hyperactivity/impulsivity symptoms than in
profile 3 (Mostert, Hoogman et al. 2015). While DeYoung et al. also found a
relationship between Extraversion and the cognitive profiles, we did not observe
this link.
The basis for the association found for Openness but not for Extraversion may
be related to the choice of instrument chosen for personality profiling, i.e. the NEO
FFI. Within the literature, there is currently a debate over the basis of personality

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
120
CHAPTER 6
traits. Some emphasise the phenotypical aspects of the FFM traits (Saucer and
Goldberg 1996), whereas others emphasize the neurobiological bases of the FFM,
such as cognition and affect (McCrae and Costa 1907 1999). Research on the levels
of affects (A), behaviours (B) and cognitions (C) included within the operational
definitions of each of the FFM traits has been conducted. They demonstrate that
Openness within the NEO FFI inventory emphasizes cognition and affect over
behaviour. Thus, the association we found between Openness and cognitive profile
1 may also simply reflect the fact that poor attention and inhibition within profile
1 is in line with the used definition of cognition (i.e. thought, beliefs, patterns, or
modes of thinking) in Openness. In contrast, for Extraversion (for which we have
not seen a relationship with cognitive profiles), there is a striking lack of cognitive
content within its NEO FFI definition and instead a substantial emphasis on its
affective aspects (i.e. internal, motivational, and evaluative ‘valenced’ states
including patterns of feelings, emotions, and preferences) and some behavioural
content (i.e. observable actions, including both active and passive behaviours, but
not including mental events) (Pytlik Zillig, Hemenover et al. 2002). Therefore, it
may be not surprising that no relationship is found with cognitive profile.
The finding that the presence of ADHD rather than cognitive profile is
associated with personality traits is in keeping with previous research questioning
the mediating role of cognition in ADHD. It is in line with the thinking that the
relationship between cognitive deficits and symptomatic aspects of ADHD is more
complex than previously recognized (Coghill, Hayward et al. 2014; Mostert,
Hoogman et al. 2015; Mostert, Onnink et al. 2015). Indeed, we observed several
direct links between personality and ADHD diagnosis. More specifically, we noted
lower Agreeableness, Conscientiousness and Extraversion and higher Neuroticism
in the ADHD participants than in the controls, irrespective of cognitive profile
and similar to previous findings on ADHD and personality (Gomez and Corr 2014).
The implications of the lack of significant interactions between adult ADHD,
cognitive profiles and personality deserve discussion. Theoretically, personality
and psychopathology can relate to one another in three different ways (Widiger
2011). Personality and psychopathology can influence the presentation or
appearance of one another, commonly referred to as a pathoplastic relationship.
They can share a common, underlying etiology, referred to as a spectrum
relationship, touching upon the possibility that personality and psychopathology
may themselves fail in some instances to be distinct entities. They may instead
exist along a common spectrum of functioning. All personality disorders may in
fact be maladaptive variants of general personality traits, and some personality
disorders could be early onset, chronic, and pervasive variants of other mental
disorders. Finally, they can have a causal role in the development or etiology of one
another. Unfortunately, the current study cannot tell us, which of the three is

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
121
FFM TRAITS RELATE TO ADHD BUT NOT TO THEIR COGNITIVE PROFILES
6
applicable to ADHD and personality, as it is a cross-sectional study in adults.
Moreover, it also suggests that personality and cognition are independent entities
without significant influence on each other. Future studies should therefore
characterise, whether the NEO FFI personality profiles are related to innate
temperament or behavioural responses. This may clarify, whether the relationship
between personality and ADHD is based on latent temperamental aspects and/or
the ability to behaviourally respond to changing internal and external cues.
Although we used data from a large sample of adults with persistent ADHD
and healthy controls, the interpretation of the results of our study should be
viewed in the context of some limitations. Firstly, the neuropsychological
measurements did not cover exactly the same cognitive domains that were used in
other studies investigating links between personality and cognitive performance.
Secondly, we focused on previously obtained cognitive profiles that were created
using a specific clustering method; different clustering methods may result in the
creation of different cognitive profiles. Thirdly, we employed the NEO FFI, which
is the shortened version of the NEO-PI-R and not intended to replace the full NEO
PI-R. As such, the NEO FFI measures a reduced range of constructs, which could be
argued not to represent the full spectrum of personality profiles. However, despite
these limitations, the current study confirms that ADHD patient show different
levels of personality traits compared to controls.
Conclusion
Our study suggests that the presence of ADHD is strongly connected to personality
traits, as four out of five factors of the FFM Model differed between ADHD patients
and healthy controls. Moreover, a link between personality and cognitive profile
was observed for Openness. Openness was significantly related to a neurocognitive
profile of poor performance on attention and inhibition tasks in ADHD patients as
well as in healthy controls. In sum, our data suggest that personality and cognitive
performance are mainly separate domains that do not share similar etiological
factors or underlying mechanisms in ADHD.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
122
CHAPTER 6
Conflict of interest The authors report no conflicts of interest. Jan Buitelaar has been in the past 3
years a consultant to/member of advisory board of/and/or speaker for Janssen Cilag
BV, Eli Lilly, Shire, Novartis, Roche and Servier. He is not an employee of any of
these companies, and not a stock shareholder of any of these companies. He has no
other financial or material support, including expert testimony, patents, and
royalties. Barbara Franke has received educational speaking fees from Merz and
Shire. Jeffrey Glennon has been in the past 3 years a consultant to Boehringer
Ingelheim on a topic not related to the content of this manuscript. Cornelis Kan
has participated in adult-ADHD Advisory and Consultancy Boards of Eli Lilly
(2011-2014) and presented the ADHD Academy of Eli Lilly (2014-2015).
Acknowledgements We thank all the participants in this study. Prof. dr. Anna Bosman and Dr. A.R. den
Otter are gratefully acknowledged for contributing their expert knowledge to the
study. This study used the sample of the Dutch node of the International Multi-
centre persistent ADHD Collaboration (IMpACT). The Dutch IMpACT study is
supported by grants from the Netherlands Organization for Scientific Research
(NWO), i.e. the NWO Brain & Cognition Excellence Program (grant 433-09-229) and
a personal Vici grant to BF (grant 016-130-669), and by grants from the Netherlands
Brain Foundation (grant 15F07[2]27) and BBMRI-NL (grant CP2010-33). The research
leading to these results also received funding from the European Community’s
Seventh Framework Programme (FP7/2007 – 2013) under grant agreements n° 278948
(TACTICS), n° 602805 (Aggressotype), n° 603016 (MATRICS), and n° 602450
(IMAGEMEND), and from the European Community’s Horizon 2020 Programme
(H2020/2014 – 2020) under grant agreements n° 643051 (MiND) and n° 667302
(CoCA).

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
123
FFM TRAITS RELATE TO ADHD BUT NOT TO THEIR COGNITIVE PROFILES
6
Sup
ple
men
tary
Tab
le 1
Ta
sks
and
ou
tcom
e m
easu
res
of t
he
neu
rop
sych
olog
ical
tes
t ba
tter
y
Task
(Co
gnit
ive
do
mai
n)
Des
crip
tio
nO
utc
om
e m
easu
re
1. B
asel
ine
Spee
d ta
sk1
(Mot
or s
pee
d &
rea
ctio
n t
ime)
A fi
xati
on c
ross
is s
how
n o
n a
com
pute
r sc
reen
, wh
ich
in
vari
able
inte
rval
s ch
ange
s in
to a
blo
ck. T
he
par
tici
pan
t is
ask
ed
to r
eact
as
fast
as
pos
sibl
e to
th
is b
lock
by
pres
sin
g a
key.
Bot
h
the
non
-dom
inan
t an
d do
min
ant
han
d ar
e as
sess
ed. S
core
s ar
e av
erag
ed o
ver
dom
inan
t an
d n
on-d
omin
ant
han
d.
Mea
n R
T SD
of R
T
2. W
AIS
-III D
igit
Spa
n t
ask
2
(Exe
cuti
ve f
un
ctio
nin
g:
Wor
kin
g m
emor
y)
Dig
it-s
trin
gs a
re r
ead
alou
d by
th
e ex
per
imen
ter.
In
th
e fo
rwar
d
con
dit
ion
, th
e pa
rtic
ipan
t is
ask
ed t
o re
pea
t d
igit
s in
th
e sa
me
orde
r. In
th
e ba
ckw
ard
con
dit
ion
, th
e pa
rtic
ipan
t is
ask
ed t
o re
pea
t th
e d
igit
s in
th
e re
vers
e or
der.
Forw
ard
dig
it s
pan
sco
reBa
ckw
ard
dig
it s
pan
sco
re
3. S
ust
ain
ed A
tten
tion
Dot
s
(SA
-dot
s) t
ask3
(Exe
cuti
ve f
un
ctio
nin
g:
Att
enti
on &
inh
ibit
ion
)
Part
icip
ants
are
ask
ed t
o re
act
to a
ser
ies
of d
ots
on t
he
scre
en;
ther
e ca
n b
e ei
ther
3, 4
or
5 do
ts p
rese
nte
d si
mu
ltan
eou
sly.
Dot
s ap
pea
r in
a r
ando
m o
rder
in a
pac
ed t
emp
o. W
hen
3 o
r 5
dots
ap
pea
r on
th
e sc
reen
, th
e p
arti
cip
ant
has
to
reac
t w
ith
, th
e ‘n
o-
key’
(th
e ke
y h
and
led
by t
he
non
-dom
inan
t h
and)
an
d w
hen
4
dots
app
ear
the
part
icip
ant
is a
sked
to
reac
t w
ith
th
e ‘y
es-k
ey’
(th
e ke
y h
and
led
by t
he
dom
inan
t h
and)
. Pre
ssin
g th
e ‘n
o-k
ey’
wh
en 4
dot
s ap
pea
r is
cal
led
a fa
lse
alar
m. P
ress
ing
the
‘yes
-key
’ w
hen
3 o
r 5
dots
app
ear
is c
alle
d a
mis
s. F
or a
nal
ysis
, th
e ta
sk is
sp
lit
up
into
10
bloc
ks,
or
seri
es, i
n o
rder
to
com
pute
var
ian
ce in
p
erfo
rman
ce o
ver
tim
e.
Mea
n s
erie
s co
mpl
etio
n t
ime
SD s
erie
s co
mpl
etio
n t
ime
SD s
erie
s er
rors
(SD
of t
he
erro
rs m
ade
acro
ss b
lock
s)R
esp
onse
bia
s (t
he
dif
fere
nce
bet
wee
n t
he
nu
mbe
r of
mis
ses
and
the
nu
mbe
r of
fals
e al
arm
s ac
ross
th
e en
tire
tas
k).
4. F
lan
ker
task
4
(Exe
cuti
ve f
un
ctio
nin
g:
Inh
ibit
ion
)
The
part
icip
ant
is p
rese
nte
d a
mat
rix
of 9
blo
cks
and
has
to
resp
ond
by in
dic
atin
g if
th
e co
lor
of t
he
mid
dle
blo
ck is
blu
e or
ye
llow
(lef
t or
rig
ht
butt
on p
ress
). In
par
t 1
of t
he
task
, th
is b
lock
is
flan
ked
by o
ther
blo
cks
in t
he
sam
e co
lor
as is
th
e m
idd
le
bloc
k (c
onsi
sten
t tr
ial),
or
in a
dif
fere
nt
colo
r (n
eutr
al t
rial
, gre
en
bloc
ks)
. In
par
t 2,
th
e m
idd
le b
lock
is fl
anke
d by
blo
cks
of t
he
sam
e co
lor
(con
sist
ent
tria
l), o
r by
blo
cks
that
hav
e th
e co
lor
of
the
alte
rnat
ive
resp
onse
(in
con
sist
ent
tria
l), fo
r ex
ampl
e, a
yel
low
bl
ock
flan
ked
by b
lue
bloc
ks
or v
ice
vers
a.
Tota
l mea
n R
T (a
vera
ge o
ver
part
1 a
nd
2)To
tal S
D o
f RT
(ave
rage
ove
r pa
rt 1
an
d 2)
In
hib
itio
n R
T (d
iffe
ren
ce in
RT
on
con
sist
ent
and
inco
nsi
sten
t tr
ials
in p
art
2)
Inh
ibit
ion
err
ors
(dif
fere
nce
in e
rror
rat
e be
twee
n c
onsi
sten
t an
d in
con
sist
ent
tria
ls
in p
art
2)

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
124
CHAPTER 6
Sup
ple
men
tary
Tab
le 1
C
onti
nu
ed
Task
(Co
gnit
ive
do
mai
n)
Des
crip
tio
nO
utc
om
e m
easu
re
5. S
ust
ain
ed A
tten
tion
to
Res
pon
se T
ask
(SA
RT)
5 (E
xecu
tive
fu
nct
ion
ing:
A
tten
tion
& in
hib
itio
n)
Ada
ptat
ion
of t
he
Go/
NoG
o ta
sk. A
str
eam
of d
igit
s (r
angi
ng
from
1
to 9
) is
pres
ente
d on
th
e sc
reen
. Th
e p
arti
cip
ant
is a
sked
to
reac
t on
th
ese
by p
ress
ing
a bu
tton
(on
a b
utt
onbo
x). T
he
stim
uli
en
sure
th
at r
eact
ion
s fo
llow
a c
erta
in p
ace.
Wh
en t
he
dig
it 3
was
pr
esen
ted,
th
e pa
rtic
ipan
t h
ad t
o w
ith
hol
d a
resp
onse
.
A c
omm
issi
on e
rror
is m
ade
wh
en t
he
part
icip
ant
pres
ses
the
butt
on w
hen
a 3
is p
rese
nte
d. A
n o
mis
sion
err
or is
mad
e w
hen
th
e pa
rtic
ipan
t do
es n
ot p
ress
th
e bu
tton
wh
en a
dig
it t
hat
is n
ot
3 is
pre
sen
ted.
Nu
mbe
r of
com
mis
sion
err
ors
Nu
mbe
r of
om
issi
on e
rror
sM
ean
RT
hit
s SD
of R
T h
its
6. T
rail
mak
ing
task
6 (E
xecu
tive
fu
nct
ion
ing:
M
otor
con
trol
& s
et-s
hif
tin
g;)
In p
art
A, p
arti
cipa
nts
are
ask
ed t
o d
raw
lin
es t
o li
nk
nu
mbe
rs
in c
onse
cuti
ve o
rder
A (1
-2-3
-…-2
5-2
6). I
n P
art
B, t
he
set-s
hif
tin
g co
nd
itio
n, p
arti
cip
ants
are
ask
ed t
o d
raw
lin
es t
o li
nk
nu
mbe
rs
and
lett
ers
in c
onse
cuti
ve o
rder
(e.g
. 1-A
-2-B
-3-…
.-K-1
2-L-
13).
Tim
e to
com
plet
e pa
rt A
Tim
e to
com
plet
e pa
rt B
Dif
fere
nce
in t
ime
to c
ompl
ete
part
B a
nd
ti
me
to c
ompl
ete
part
A.
7. S
eman
tic
cate
gory
an
d
init
ial l
ette
r fl
uen
cy7
(Exe
cuti
ve f
un
ctio
nin
g:
Spee
ch fl
uen
cy)
In t
he
firs
t pa
rt, p
arti
cipa
nts
are
ask
ed t
o n
ame
as m
any
anim
als
as t
hey
can
wit
hin
1 m
inu
te, a
fter
war
ds
they
are
ask
ed t
o m
enti
on a
s m
uch
pro
fess
ion
s as
th
ey c
an w
ith
in 1
min
ute
. In
th
e se
con
d p
art
of t
he
task
par
tici
pan
ts a
re g
iven
a fi
rst-l
ette
r an
d
are
aske
d to
men
tion
as
man
y w
ord
s as
th
ey k
now
th
at b
egin
w
ith
th
at le
tter
. Th
ey h
ave
3 tr
ials
: on
e w
ith
th
e le
tter
‘T’,
one
wit
h t
he
lett
er ‘A
’ an
d on
e w
ith
th
e le
tter
‘D’.
Nu
mbe
r of
wor
ds
men
tion
ed in
ca
tego
ry a
nim
als
Nu
mbe
r of
wor
ds
men
tion
ed in
cat
egor
y pr
ofes
sion
sN
um
ber
of w
ord
s m
enti
oned
in c
ateg
ory
lett
ers
(tot
al o
f 3 le
tter
-tri
als)
8. D
elay
Dis
cou
nti
ng
task
8 (D
elay
ave
rsio
n &
impu
lsiv
ity)
The
part
icip
ant
is r
epea
ted
ly a
sked
to
mak
e a
choi
ce b
etw
een
tw
o (h
ypot
het
ical
) in
cen
tive
s. O
ne
opti
on g
ener
ates
an
ince
nti
ve
(mon
ey) a
t a
shor
t p
erio
d w
hil
e th
e ot
her
opt
ion
gen
erat
es a
n
ince
nti
ve a
t a
late
r ti
me
(i.e.
“D
o yo
u p
refe
r to
rec
eive
30
Euro
s 18
0 da
ys f
rom
now
, or
2 Eu
ros
imm
edia
tely
?”).
Du
rin
g th
e ta
sk, t
he
valu
e of
th
e in
cen
tive
s as
wel
l as
the
tim
e of
th
e de
lay
(wit
h w
hic
h t
he
ince
nti
ve is
gai
ned
) are
var
ied.
Th
e im
puls
ivit
y pa
ram
eter
(k) i
s co
mpu
ted
from
th
e pr
esen
t va
lue
of t
he
dela
yed
re
war
d (V
), th
e re
al v
alu
e of
th
e de
laye
d re
war
d (a
) an
d th
e de
lay
in d
ays
(D) w
ith
th
e fo
rmu
la: V
= a
/ (1+
kD
).
K 1
00
K 3
0 K
10
9. T
ime
Esti
mat
ion
tas
k9
(Tim
ing)
To s
how
th
e le
ngt
h o
f on
e se
con
d,
the
part
icip
ant
is fi
rst
show
n
a pi
ctu
re o
n a
com
pute
r sc
reen
for
one
seco
nd,
th
is is
rep
eate
d
ten
tim
es. N
ext,
th
e pa
rtic
ipan
t h
as t
o re
act
to a
sou
nd
by
pres
sin
g th
e sp
ace
bar
one
seco
nd
afte
r th
e so
un
d is
pre
sen
ted.
Pa
rtic
ipan
ts r
ecei
ve fe
edba
ck a
fter
eac
h t
rial
on
th
e ac
cura
cy o
f th
eir
tim
ing
(‘too
slo
w’,
‘too
fast
’, ‘c
orre
ct’).
Med
ian
res
pon
se t
ime
Abs
olu
te d
evia
tion
of t
he
med
ian
res
pon
se
tim
e fr
om 1
000
ms
AN
T =
‘Am
ster
dam
se N
euro
psy
chol
ogis
che
Test
’ (D
e So
nn
evil
le 1
999)
; RT
= re
acti
on t
ime;
SD
= s
tan
dar
d d
evia
tion
1 P
art
of t
he
AN
T te
stin
g ba
tter
y
2 S
ubt
est
of t
he
Wec
hsl
er A
dult
Inte
llig
ence
Sca
le S
attl
er, J
. M. (
1992
). A
sses
smen
t of
Ch
ild
ren
: WIS
C-I
II a
nd
WPP
SI-R
Su
pp
lem
ent.
La
Mes
a, C
A, U
SA, J
erom
e M
. Sat
tler
,
Pu
blis
her
, In
c, W
ech
sler
, D. (
1997
). W
AIS
-III
—W
ech
sler
Adu
lt I
nte
llig
ence
Sca
le. S
an A
nto
nio
, Psy
chol
ogic
al C
orp
orat
ion
..
3 P
art
of t
he
AN
T te
stin
g ba
tter
y H
uij
breg
ts,
S. C
., A
. J. W
arre
n,
et a
l. (2
008)
. “H
ot a
nd
coo
l fo
rms
of i
nh
ibit
ory
con
trol
an
d e
xter
nal
izin
g b
ehav
ior
in c
hil
dre
n o
f
mot
her
s w
ho
smok
ed d
uri
ng
pre
gnan
cy: a
n e
xplo
rato
ry s
tud
y.”
J Abn
orm
Ch
ild
Psy
chol
36(
3): 3
23-3
33.
4 P
art
of t
he
AN
T te
stin
g H
uij
breg
ts,
S. C
., L.
M.
de
Son
nev
ille
, et
al.
(200
2).
“Th
e n
euro
psy
chol
ogic
al p
rofi
le o
f ea
rly
and
con
tin
uou
sly
trea
ted
ph
enyl
keto
nu
ria:
orie
nti
ng,
vig
ilan
ce, a
nd
mai
nte
nan
ce v
ersu
s m
anip
ula
tion
-fu
nct
ion
s of
wor
kin
g m
emor
y.”
Neu
rosc
i Bio
beh
av R
ev 2
6(6)
: 697
-712
.
5 S
mit
, A. S
., P.
A. T
. M. E
lin
g, e
t al
. (20
04).
“Men
tal e
ffor
t ca
use
s vi
gila
nce
dec
reas
e du
e to
res
ourc
e d
eple
tion
.” A
cta
Psyc
hol
ogic
a 11
5(1)
: 35
-42.
6 K
ortt
e, K
. B.,
M. D
. Hor
ner
, et
al. (
2002
). “T
he
trai
l m
akin
g te
st, p
art
B: c
ogn
itiv
e fl
exib
ilit
y or
abi
lity
to
mai
nta
in s
et?”
Ap
pl
Neu
rop
sych
ol 9
(2):
106
-109
, Stu
ss, D
. T.
and
B. L
evin
e (2
002)
. “A
dult
cli
nic
al n
euro
psy
chol
ogy:
Les
son
s fr
om s
tud
ies
of t
he
fron
tal l
obes
.” A
nn
ual
Rev
iew
of
Psyc
hol
ogy
53: 4
01-4
33, Z
akza
nis
, K. K
., R
. Mra
z,
et a
l. (2
005)
. “A
n f
MR
I stu
dy
of t
he
Trai
l Mak
ing
Test
.” N
euro
psy
chol
ogia
43(
13):
1878
-188
6.
7 H
urk
s, P
. P. M
., J.
G. M
. Hen
dri
kse
n, e
t al
. (20
04).
“Ver
bal fl
uen
cy o
ver
tim
e as
a m
easu
re o
f au
tom
atic
an
d c
ontr
olle
d p
roce
ssin
g in
ch
ild
ren
wit
h A
DH
D.”
Bra
in a
nd
Cog
nit
ion
55(
3): 5
35-5
44.
8 D
om, G
., P.
D’H
aen
e, e
t al
. (20
06).
“Im
pu
lsiv
ity
in a
bsti
nen
t ea
rly-
an
d l
ate-
onse
t al
coh
olic
s: d
iffe
ren
ces
in s
elf-r
epor
t m
easu
res
and
a d
isco
un
tin
g ta
sk.”
Ad
dic
tion
101(
1): 5
0-5
9.
9 V
an M
eel,
C. S
., J.
Oos
terl
aan
, et
al. (
2005
). “M
otiv
atio
nal
eff
ects
on
mot
or t
imin
g in
att
enti
on-d
efici
t/h
yper
acti
vity
dis
ord
er.”
Jou
rnal
of
the
Am
eric
an A
cad
emy
of
Ch
ild
an
d A
dol
esce
nt
Psyc
hia
try
44
(5):
451-
460
, R
omm
else
, N
. N
. J.,
M.
E.
Alt
ink
, et
al.
(200
8).
“Sp
eed
, va
riab
ilit
y, a
nd
tim
ing
of m
otor
ou
tpu
t in
AD
HD
: W
hic
h
mea
sure
s ar
e u
sefu
l for
en
dop
hen
otyp
ic r
esea
rch
?” B
ehav
ior
Gen
etic
s 38
(2):
121-
132.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
125
FFM TRAITS RELATE TO ADHD BUT NOT TO THEIR COGNITIVE PROFILES
6
Sup
ple
men
tary
Tab
le 1
C
onti
nu
ed
Task
(Co
gnit
ive
do
mai
n)
Des
crip
tio
nO
utc
om
e m
easu
re
5. S
ust
ain
ed A
tten
tion
to
Res
pon
se T
ask
(SA
RT)
5 (E
xecu
tive
fu
nct
ion
ing:
A
tten
tion
& in
hib
itio
n)
Ada
ptat
ion
of t
he
Go/
NoG
o ta
sk. A
str
eam
of d
igit
s (r
angi
ng
from
1
to 9
) is
pres
ente
d on
th
e sc
reen
. Th
e p
arti
cip
ant
is a
sked
to
reac
t on
th
ese
by p
ress
ing
a bu
tton
(on
a b
utt
onbo
x). T
he
stim
uli
en
sure
th
at r
eact
ion
s fo
llow
a c
erta
in p
ace.
Wh
en t
he
dig
it 3
was
pr
esen
ted,
th
e pa
rtic
ipan
t h
ad t
o w
ith
hol
d a
resp
onse
.
A c
omm
issi
on e
rror
is m
ade
wh
en t
he
part
icip
ant
pres
ses
the
butt
on w
hen
a 3
is p
rese
nte
d. A
n o
mis
sion
err
or is
mad
e w
hen
th
e pa
rtic
ipan
t do
es n
ot p
ress
th
e bu
tton
wh
en a
dig
it t
hat
is n
ot
3 is
pre
sen
ted.
Nu
mbe
r of
com
mis
sion
err
ors
Nu
mbe
r of
om
issi
on e
rror
sM
ean
RT
hit
s SD
of R
T h
its
6. T
rail
mak
ing
task
6 (E
xecu
tive
fu
nct
ion
ing:
M
otor
con
trol
& s
et-s
hif
tin
g;)
In p
art
A, p
arti
cipa
nts
are
ask
ed t
o d
raw
lin
es t
o li
nk
nu
mbe
rs
in c
onse
cuti
ve o
rder
A (1
-2-3
-…-2
5-2
6). I
n P
art
B, t
he
set-s
hif
tin
g co
nd
itio
n, p
arti
cip
ants
are
ask
ed t
o d
raw
lin
es t
o li
nk
nu
mbe
rs
and
lett
ers
in c
onse
cuti
ve o
rder
(e.g
. 1-A
-2-B
-3-…
.-K-1
2-L-
13).
Tim
e to
com
plet
e pa
rt A
Tim
e to
com
plet
e pa
rt B
Dif
fere
nce
in t
ime
to c
ompl
ete
part
B a
nd
ti
me
to c
ompl
ete
part
A.
7. S
eman
tic
cate
gory
an
d
init
ial l
ette
r fl
uen
cy7
(Exe
cuti
ve f
un
ctio
nin
g:
Spee
ch fl
uen
cy)
In t
he
firs
t pa
rt, p
arti
cipa
nts
are
ask
ed t
o n
ame
as m
any
anim
als
as t
hey
can
wit
hin
1 m
inu
te, a
fter
war
ds
they
are
ask
ed t
o m
enti
on a
s m
uch
pro
fess
ion
s as
th
ey c
an w
ith
in 1
min
ute
. In
th
e se
con
d p
art
of t
he
task
par
tici
pan
ts a
re g
iven
a fi
rst-l
ette
r an
d
are
aske
d to
men
tion
as
man
y w
ord
s as
th
ey k
now
th
at b
egin
w
ith
th
at le
tter
. Th
ey h
ave
3 tr
ials
: on
e w
ith
th
e le
tter
‘T’,
one
wit
h t
he
lett
er ‘A
’ an
d on
e w
ith
th
e le
tter
‘D’.
Nu
mbe
r of
wor
ds
men
tion
ed in
ca
tego
ry a
nim
als
Nu
mbe
r of
wor
ds
men
tion
ed in
cat
egor
y pr
ofes
sion
sN
um
ber
of w
ord
s m
enti
oned
in c
ateg
ory
lett
ers
(tot
al o
f 3 le
tter
-tri
als)
8. D
elay
Dis
cou
nti
ng
task
8 (D
elay
ave
rsio
n &
impu
lsiv
ity)
The
part
icip
ant
is r
epea
ted
ly a
sked
to
mak
e a
choi
ce b
etw
een
tw
o (h
ypot
het
ical
) in
cen
tive
s. O
ne
opti
on g
ener
ates
an
ince
nti
ve
(mon
ey) a
t a
shor
t p
erio
d w
hil
e th
e ot
her
opt
ion
gen
erat
es a
n
ince
nti
ve a
t a
late
r ti
me
(i.e.
“D
o yo
u p
refe
r to
rec
eive
30
Euro
s 18
0 da
ys f
rom
now
, or
2 Eu
ros
imm
edia
tely
?”).
Du
rin
g th
e ta
sk, t
he
valu
e of
th
e in
cen
tive
s as
wel
l as
the
tim
e of
th
e de
lay
(wit
h w
hic
h t
he
ince
nti
ve is
gai
ned
) are
var
ied.
Th
e im
puls
ivit
y pa
ram
eter
(k) i
s co
mpu
ted
from
th
e pr
esen
t va
lue
of t
he
dela
yed
re
war
d (V
), th
e re
al v
alu
e of
th
e de
laye
d re
war
d (a
) an
d th
e de
lay
in d
ays
(D) w
ith
th
e fo
rmu
la: V
= a
/ (1+
kD
).
K 1
00
K 3
0 K
10
9. T
ime
Esti
mat
ion
tas
k9
(Tim
ing)
To s
how
th
e le
ngt
h o
f on
e se
con
d,
the
part
icip
ant
is fi
rst
show
n
a pi
ctu
re o
n a
com
pute
r sc
reen
for
one
seco
nd,
th
is is
rep
eate
d
ten
tim
es. N
ext,
th
e pa
rtic
ipan
t h
as t
o re
act
to a
sou
nd
by
pres
sin
g th
e sp
ace
bar
one
seco
nd
afte
r th
e so
un
d is
pre
sen
ted.
Pa
rtic
ipan
ts r
ecei
ve fe
edba
ck a
fter
eac
h t
rial
on
th
e ac
cura
cy o
f th
eir
tim
ing
(‘too
slo
w’,
‘too
fast
’, ‘c
orre
ct’).
Med
ian
res
pon
se t
ime
Abs
olu
te d
evia
tion
of t
he
med
ian
res
pon
se
tim
e fr
om 1
000
ms
AN
T =
‘Am
ster
dam
se N
euro
psy
chol
ogis
che
Test
’ (D
e So
nn
evil
le 1
999)
; RT
= re
acti
on t
ime;
SD
= s
tan
dar
d d
evia
tion
1 P
art
of t
he
AN
T te
stin
g ba
tter
y
2 S
ubt
est
of t
he
Wec
hsl
er A
dult
Inte
llig
ence
Sca
le S
attl
er, J
. M. (
1992
). A
sses
smen
t of
Ch
ild
ren
: WIS
C-I
II a
nd
WPP
SI-R
Su
pp
lem
ent.
La
Mes
a, C
A, U
SA, J
erom
e M
. Sat
tler
,
Pu
blis
her
, In
c, W
ech
sler
, D. (
1997
). W
AIS
-III
—W
ech
sler
Adu
lt I
nte
llig
ence
Sca
le. S
an A
nto
nio
, Psy
chol
ogic
al C
orp
orat
ion
..
3 P
art
of t
he
AN
T te
stin
g ba
tter
y H
uij
breg
ts,
S. C
., A
. J. W
arre
n,
et a
l. (2
008)
. “H
ot a
nd
coo
l fo
rms
of i
nh
ibit
ory
con
trol
an
d e
xter
nal
izin
g b
ehav
ior
in c
hil
dre
n o
f
mot
her
s w
ho
smok
ed d
uri
ng
pre
gnan
cy: a
n e
xplo
rato
ry s
tud
y.”
J Abn
orm
Ch
ild
Psy
chol
36(
3): 3
23-3
33.
4 P
art
of t
he
AN
T te
stin
g H
uij
breg
ts,
S. C
., L.
M.
de
Son
nev
ille
, et
al.
(200
2).
“Th
e n
euro
psy
chol
ogic
al p
rofi
le o
f ea
rly
and
con
tin
uou
sly
trea
ted
ph
enyl
keto
nu
ria:
orie
nti
ng,
vig
ilan
ce, a
nd
mai
nte
nan
ce v
ersu
s m
anip
ula
tion
-fu
nct
ion
s of
wor
kin
g m
emor
y.”
Neu
rosc
i Bio
beh
av R
ev 2
6(6)
: 697
-712
.
5 S
mit
, A. S
., P.
A. T
. M. E
lin
g, e
t al
. (20
04).
“Men
tal e
ffor
t ca
use
s vi
gila
nce
dec
reas
e du
e to
res
ourc
e d
eple
tion
.” A
cta
Psyc
hol
ogic
a 11
5(1)
: 35
-42.
6 K
ortt
e, K
. B.,
M. D
. Hor
ner
, et
al. (
2002
). “T
he
trai
l m
akin
g te
st, p
art
B: c
ogn
itiv
e fl
exib
ilit
y or
abi
lity
to
mai
nta
in s
et?”
Ap
pl
Neu
rop
sych
ol 9
(2):
106
-109
, Stu
ss, D
. T.
and
B. L
evin
e (2
002)
. “A
dult
cli
nic
al n
euro
psy
chol
ogy:
Les
son
s fr
om s
tud
ies
of t
he
fron
tal l
obes
.” A
nn
ual
Rev
iew
of
Psyc
hol
ogy
53: 4
01-4
33, Z
akza
nis
, K. K
., R
. Mra
z,
et a
l. (2
005)
. “A
n f
MR
I stu
dy
of t
he
Trai
l Mak
ing
Test
.” N
euro
psy
chol
ogia
43(
13):
1878
-188
6.
7 H
urk
s, P
. P. M
., J.
G. M
. Hen
dri
kse
n, e
t al
. (20
04).
“Ver
bal fl
uen
cy o
ver
tim
e as
a m
easu
re o
f au
tom
atic
an
d c
ontr
olle
d p
roce
ssin
g in
ch
ild
ren
wit
h A
DH
D.”
Bra
in a
nd
Cog
nit
ion
55(
3): 5
35-5
44.
8 D
om, G
., P.
D’H
aen
e, e
t al
. (20
06).
“Im
pu
lsiv
ity
in a
bsti
nen
t ea
rly-
an
d l
ate-
onse
t al
coh
olic
s: d
iffe
ren
ces
in s
elf-r
epor
t m
easu
res
and
a d
isco
un
tin
g ta
sk.”
Ad
dic
tion
101(
1): 5
0-5
9.
9 V
an M
eel,
C. S
., J.
Oos
terl
aan
, et
al. (
2005
). “M
otiv
atio
nal
eff
ects
on
mot
or t
imin
g in
att
enti
on-d
efici
t/h
yper
acti
vity
dis
ord
er.”
Jou
rnal
of
the
Am
eric
an A
cad
emy
of
Ch
ild
an
d A
dol
esce
nt
Psyc
hia
try
44
(5):
451-
460
, R
omm
else
, N
. N
. J.,
M.
E.
Alt
ink
, et
al.
(200
8).
“Sp
eed
, va
riab
ilit
y, a
nd
tim
ing
of m
otor
ou
tpu
t in
AD
HD
: W
hic
h
mea
sure
s ar
e u
sefu
l for
en
dop
hen
otyp
ic r
esea
rch
?” B
ehav
ior
Gen
etic
s 38
(2):
121-
132.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
126
CHAPTER 6
References
Association, A. P. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV TR®. Washington,
DC, American Psychiatric Press.
Barkley, R. A. (1997). “Behavioral inhibition, sustained attention, and executive functions: constructing a
unifying theory of ADHD.” Psychol Bull 121(1): 65-94.
Castellanos, F. X. and R. Tannock (2002). “Neuroscience of attention-deficit/hyperactivity disorder: the
search for endophenotypes.” Nat Rev Neurosci 3(8): 617-628.
Coghill, D. R., D. Hayward, et al. (2014). “A longitudinal examination of neuropsychological and clinical
functioning in boys with attention deficit hyperactivity disorder (ADHD): improvements in executive
functioning do not explain clinical improvement.” Psychol Med 44(5): 1087-1099.
Coghill, D. R., S. Seth, et al. (2014). “A comprehensive assessment of memory, delay aversion, timing,
inhibition, decision making and variability in attention deficit hyperactivity disorder: advancing
beyond the three-pathway models.” Psychol Med 44(9): 1989-2001.
Costa, P. T., Jr. and R. R. McCrae (1992). Manual for the revised NEO personality inventory (NEO P-R) and NEO
five-factor inventory (NEO-FFI). Odessa, Psychological Assessment Resources.
De Sonneville, L. M. J. (1999). Amsterdam Neuropsychological Tasks: a computer-aided assessment program.
Cognitive ergonomics, clinical assessment and computer-assisted learning: Computers in Psychology.
B. P. L. M. Den Brinker, P. J. Beek, A. N. Brand, S. J. Maarse and L. J. M. Mulder. Lisse, The Netherlands,
Swets & Zeitlinger. 6: 187-203.
de Zeeuw, P., J. Weusten, et al. (2012). “Deficits in cognitive control, timing and reward sensitivity appear
to be dissociable in ADHD.” PLoS One 7(12): e51416.
Deyoung, C. G., J. B. Peterson, et al. (2008). “Externalizing behavior and the higher order factors of the Big
Five.” J Abnorm Psychol 117(4): 947-953.
Dom, G., P. D’Haene, et al. (2006). “Impulsivity in abstinent early- and late-onset alcoholics: differences in
self-report measures and a discounting task.” Addiction 101(1): 50-59.
Fair, D. A., D. Bathula, et al. (2012). “Distinct neuropsychological subgroups in typically developing youth
inform heterogeneity in children with ADHD.” Proc Natl Acad Sci U S A 109(17): 6769-6774.
Faraone, S. V. A., P. ; Banaschewski, T. ; Biederman, J. ; Buitelaar, J.K. ; Ramos-Quiroga, J.A. ; Rohde, L.A. ;
Sonuga-Barke, E. ; Tannock, R. ; Franke, B. (2015). “Attention Deficit Hyperactivity Disorder. .” Nature
Review Disease Primers.
Franke, B., M. Hoogman, et al. (2008). “Association of the dopamine transporter (SLC6A3/DAT1) gene 9-6
haplotype with adult ADHD.” Am J Med Genet B Neuropsychiatr Genet 147B(8): 1576-1579.
Franke, B., A. A. Vasquez, et al. (2010). “Multicenter analysis of the SLC6A3/DAT1 VNTR haplotype in
persistent ADHD suggests differential involvement of the gene in childhood and persistent ADHD.”
Neuropsychopharmacology 35(3): 656-664.
Gomez, R. and P. J. Corr (2014). “ADHD and personality: a meta-analytic review.” Clin Psychol Rev 34(5): 376-388.
Graham, E. K. and M. E. Lachman (2014). “Personality Traits, Facets and Cognitive Performance: Age
Differences in Their Relations.” Pers Individ Dif 59: 89-95.
Groenestijn, M., G. Akkerhuis, et al. (1999). Gestructureerd klinisch interview voor de vaststelling van
DSM-IV as I stoornissen [structured Clinical Interview for DSM-IV axis I disorders]. Lisse, The
Netherlands, Swets & Zeitlinger.
Hirsh, J., D. Morisano, et al. (2008). “Delay discounting: Interactions between personality and cognitive
ability.” Journal of Research in Personality(42): 1646-1650.
Hoogman, M., E. Aarts, et al. (2011). “Nitric oxide synthase genotype modulation of impulsivity and ventral
striatal activity in adult ADHD patients and healthy comparison subjects.” Am J Psychiatry 168(10):
1099-1106.
Hoogman, M., M. Onnink, et al. (2013). “The dopamine transporter haplotype and reward-related striatal
responses in adult ADHD.” Eur Neuropsychopharmacol 23(6): 469-478.
Huijbregts, S. C., L. M. de Sonneville, et al. (2002). “The neuropsychological profile of early and continuously
treated phenylketonuria: orienting, vigilance, and maintenance versus manipulation-functions of
working memory.” Neurosci Biobehav Rev 26(6): 697-712.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
127
FFM TRAITS RELATE TO ADHD BUT NOT TO THEIR COGNITIVE PROFILES
6
Huijbregts, S. C., A. J. Warren, et al. (2008). “Hot and cool forms of inhibitory control and externalizing
behavior in children of mothers who smoked during pregnancy: an exploratory study.” J Abnorm
Child Psychol 36(3): 323-333.
Hurks, P. P. M., J. G. M. Hendriksen, et al. (2004). “Verbal fluency over time as a measure of automatic and
controlled processing in children with ADHD.” Brain and Cognition 55(3): 535-544.
Karalunas, S. L., D. Fair, et al. (2014). “Subtyping attention-deficit/hyperactivity disorder using temperament
dimensions: toward biologically based nosologic criteria.” JAMA Psychiatry 71(9): 1015-1024.
Kooij, J. J. (2010). Diagnostic interview for ADHD in adults 2.0 (DIVA 2.0). Adult ADHD. Diagnostic Assessment
and Treatment. Amsterdam, Pearson Assessment and Information BV.
Kooij, J. J., J. K. Buitelaar, et al. (2005). “Internal and external validity of attention-deficit hyperactivity
disorder in a population-based sample of adults.” Psychol Med 35(6): 817-827.
Kortte, K. B., M. D. Horner, et al. (2002). “The trail making test, part B: cognitive flexibility or ability to
maintain set?” Appl Neuropsychol 9(2): 106-109.
Leth-Steensen, C., Z. K. Elbaz, et al. (2000). “Mean response times, variability, and skew in the responding of
ADHD children: a response time distributional approach.” Acta Psychol (Amst) 104(2): 167-190.
McCrae, R. R. and P. T. Costa (2004). “A contemplated revision of the NEO Five-Factor Inventory.” Personality
and Individual Differences 36: 587-596.
Mostert, J. C., M. Hoogman, et al. (2015). “Similar Subgroups Based on Cognitive Performance Parse
Heterogeneity in Adults With ADHD and Healthy Controls.” J Atten Disord.
Mostert, J. C., A. M. Onnink, et al. (2015). “Cognitive heterogeneity in adult attention deficit/hyperactivity
disorder: A systematic analysis of neuropsychological measurements.” Eur Neuropsychopharmacol.
Murdock, K. W., K. B. Oddi, et al. (2013). “Cognitive correlates of personality.” Journal of Individual
Differences 34(2): 97-104.
Nigg, J. T., G. Stavro, et al. (2005). “Executive functions and ADHD in adults: Evidence for selective effects on
ADHD symptom domains.” Journal of Abnormal Psychology 114(4): 706-717.
Onnink, A. M., M. P. Zwiers, et al. (2014). “Brain alterations in adult ADHD: effects of gender, treatment and
comorbid depression.” Eur Neuropsychopharmacol 24(3): 397-409.
Pennington, B. F. and S. Ozonoff (1996). “Executive functions and developmental psychopathology.” J Child
Psychol Psychiatry 37(1): 51-87.
Pytlik Zillig, L. M., S. H. Hemenover, et al. (2002). “What do we assess when we assess a Big 5 trait? A content
analysis of the affective, behavioral, and cognitive proecesses represented in Big 5 personality
inventories.” Personality and Social Psychology Bulletin 28(6): 847-858.
Rommelse, N. N. J., M. E. Altink, et al. (2008). “Speed, variability, and timing of motor output in ADHD:
Which measures are useful for endophenotypic research?” Behavior Genetics 38(2): 121-132.
Rothbart, M. K. (2007). “Temperament, development, and personality.” Current Directions in Psychological
Science 16: 207-212.
Rothbart, M. K. (2011). Becoming who we are: Temperament and personality in development. . New York,
NY, Guidford Press.
Sattler, J. M. (1992). Assessment of Children: WISC-III and WPPSI-R Supplement. La Mesa, CA, USA, Jerome
M. Sattler, Publisher, Inc.
Schachar, R., V. L. Mota, et al. (2000). “Confirmation of an inhibitory control deficit in attention-deficit/
hyperactivity disorder.” J Abnorm Child Psychol 28(3): 227-235.
Smit, A. S., P. A. T. M. Eling, et al. (2004). “Mental effort causes vigilance decrease due to resource depletion.”
Acta Psychologica 115(1): 35-42.
Sonuga-Barke, E., P. Bitsakou, et al. (2010). “Beyond the dual pathway model: evidence for the dissociation of
timing, inhibitory, and delay-related impairments in attention-deficit/hyperactivity disorder.” J Am
Acad Child Adolesc Psychiatry 49(4): 345-355.
Stuss, D. T. and B. Levine (2002). “Adult clinical neuropsychology: Lessons from studies of the frontal lobes.”
Annual Review of Psychology 53: 401-433.
van Hulst, B. M., P. de Zeeuw, et al. (2015). “Distinct neuropsychological profiles within ADHD: a latent class
analysis of cognitive control, reward sensitivity and timing.” Psychol Med 45(4): 735-745.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
128
CHAPTER 6
Van Meel, C. S., J. Oosterlaan, et al. (2005). “Motivational effects on motor timing in attention-deficit/
hyperactivity disorder.” Journal of the American Academy of Child and Adolescent Psychiatry 44(5):
451-460.
Wechsler, D. (1997). WAIS-III—Wechsler Adult Intelligence Scale. San Antonio, Psychological Corporation.
Weertman, A., A. Arntz, et al. (2000). Gestructureerd klinisch interview voor DSM-IV as II persoonlijkheids-
stoornissen [The Structured Clinical Interview for DSM-IVAxis II Disorders]. Lisse, The Netherlands,
Swets & Zeitlinger.
Widiger, T. A. (2011). “Personality and psychopathology.” World Psychiatry 10: 103-106.
Williams, P. G., Y. Suchy, et al. (2010). “Five-Factor Model personality traits and executive functioning
among older adults.” Journal of Research in Personality 44: 485-491.
Williams, P. G., Y. Suchy, et al. (2009). “Individual differences in executive functioning: implications for
stress regulation.” Ann Behav Med 37(2): 126-140.
Zakzanis, K. K., R. Mraz, et al. (2005). “An fMRI study of the Trail Making Test.” Neuropsychologia 43(13):
1878-1886.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
129
FFM TRAITS RELATE TO ADHD BUT NOT TO THEIR COGNITIVE PROFILES
6

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Summary and General Discussion
7

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
133
SUMMARY AND GENERAL DISCUSSION
7
Summary and General Discussion
The current thesis examines both the symptomatic overlap and differences
between ADHD and BPD, and studies the interactions with regard to symptoms,
temperament/personality, and response inhibition (chapter 3-5). Furthermore,
chapter 6 focuses on the relationship between neurocognition and personality
traits in adult ADHD vs controls.
Here we summarize and discuss our findings within the context of the
literature in this field. The clinical relevance and recommendations for future
research are then outlined.
Summary of our main findings
Chapter 2, a literature review, dealt with several concepts and issues concerning
the relation of adult ADHD to personality disorders and traits. One of our conclusions
was that most previous studies on adult ADHD and personality did not account for
co-occurring personality disorders, making it difficult to draw specific conclusions
on the delineation and overlap among ADHD, personality disorders and personality
traits.
In chapter 3 we illustrated that every female with BPD in our sample had some
ADHD symptoms in both childhood and adulthood and that hyperactivity
symptoms appear to be characteristic for both female ADHD and BPD patients. We
suggested that hyperactivity could play a mediating role in the development of
BPD along the path of ADHD.
This connects with our finding in chapter 4 where we showed that an outspoken
Novelty Seeking temperament suggests a vulnerability for the development of
female ADHD and co-occurring BPD. Here we also pointed out that females with
only symptoms of ADHD (i.e. without BPD symptoms) showed normal character
development and thus absence of a personality disorder.
In chapter 5 we addressed whether the shared hyperactivity symptoms and
impulsivity traits are pointing to the same underlying cognitive processes or whether
ADHD and BPD could be differentiated at the level of cognitive processes. We showed
that, independently of ADHD, response inhibition deficits are also related to BPD.
Moreover, contrary to patients with ADHD, BPD patients may suffer from more
widespread inhibition deficiencies and a specific impairment in context processing.
Thus, it seems that ADHD and BPD share features of hyperactivity and
impulsivity at the level of symptoms, personality traits and neurocognitive
performance. An interesting question following this conclusion is whether such
clinical features, neurocognitive performance, and personality traits are related

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
134
CHAPTER 7
to one another, taking the presence of psychopathology into account. In Chapter 6
we showed that there was no relation between cognitive profile and personality in
the ADHD population, and that the presence of ADHD rather than cognitive profile
is associated with personality traits.
General Discussion
There is no BPD without at least some current and childhood ADHD hyperactivity/impulsivity symptoms The clinical distinction to enable the diagnosis (and treatment) of adults with BPD
(and ADHD) is not clearly defined. In this regard, understanding how ADHD and
BPD are different and/or alike in order to create a clinical distinction is important.
A common underlying trait such as impulsivity can create co-occurrence and obscure
syndrome specific symptoms. Furthermore, not appreciating the comorbidity of BPD
with ADHD could result in inappropriate treatment. Previous studies had already
documented associations between symptoms of ADHD in either childhood or
adulthood and BPD, but rather than showing differences in clinical severity of the
symptoms we have identified qualitatively different symptom profiles for both
childhood and adult ADHD and adult BPD symptoms in female adults with ADHD
and/or BPD (chapter 3).
Whereas adults with a primary diagnosis of ADHD and no BPD showed no
symptoms of BPD, we found that all adults with BPD showed some ADHD symptoms,
with at least hyperactivity/impulsivity. Some adults also showed a symptom profile
with BPD, hyperactivity/impulsivity, and inattention problems. While inattention
symptoms may not be exclusive in ADHD, they may play a role in other diagnostic
cohorts such as BPD. We also showed that the presence of hyperactive/impulsive
symptoms in childhood could possibly play a mediating role in the development of
an adult BPD. This study therefore develops our understanding of the evolution of
BPD in adulthood from childhood ADHD symptoms. Moreover, since we included
only women in this clinical sample and the sex ratio for ADHD is more equally
divided than for BPD (1:1 vs. 1:3 male: female), the results are probably more
representative for the population with BPD. It is not yet determined which factors
mediate whether childhood ADHD progresses to adult ADHD rather than adult
BPD (or both).
In summary, we conclude that hyperactivity/impulsivity has little discriminative
value for ADHD and BPD in women. Most likely, a client with a BPD diagnosis has
already had (and may still retain) hyperactivity/impulsivity symptoms in childhood
similar to that seen in ADHD. Although it is possible that the processes underlying
the expression of any one childhood disorder may increase the likelihood of

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
135
SUMMARY AND GENERAL DISCUSSION
7
developing BPD in adulthood, we suggest that hyperactivity/impulsivity is one, of
maybe several, unique areas of overlap between BPD and ADHD which warrant
further investigation as to the links between these conditions. Indeed, previous
research has demonstrated that disruptive behavior disorders and ADHD are
predictive of personality disorders (which includes BPD) (Helgeland, Kjelsberg et
al. 2005; Miller, Flory et al. 2008).
Prospective research demonstrated that growth scores in ADHD severity from
10-13 years predicted BPD symptoms at age 14. Additionally, the development of
ODD severity in age 8-10 years also predicted BPD symptoms at age 14 (Stepp, Burke
et al. 2012). Such findings indeed suggest that girls who develop BPD symptoms
may experience many features in common with girls who have ADHD (and ODD).
Furthermore, a recent study revealed a significant association between ADHD and
BPD symptoms and showed that impulsivity, as well as emotion dysregulation,
fully mediated the relationship between retrospectively assessed ADHD symptoms
and current BPD features (Fossati, Gratz et al. 2015). Notably and surprisingly, this
effect was found to be true among only females (vs males). The authors conclude
therefore that gender seems to be an important factor to consider in understanding
the relation between (childhood) ADHD and BPD, at least in clinical populations.
Previous literature mostly suggests that men and women with BPD are more
similar in their clinical presentation than they are different. Gender differences
are found in the type of impulse related disorders that they predominantly display.
For example women are more familiar with eating disorders (internalizing behaviors)
and men with substance abuse and antisocial personality disorder (externalizing
behaviors) (Zanarini, Frankenburg et al. 1998; Zlotnick, Rothschild et al. 2002).
However, it has also been suggested that the few gender differences that are found
in BPD are similar to those found in the general population (Johnson, Shea et al.
2003). Epidemiological research on eating disorders have shown that eating
disorders are more prevalent in women than in men and community studies have
reported higher rates of antisocial behavior in men than in women (Hsu 1996;
Torgersen, Kringlen et al. 2001)
In sum, chapter 3 in this thesis adds to a growing body of literature that
provides support for the notion that ADHD and BPD in women are probably, but
not solely, linked through hyperactivity/impulsivity features. Whether BPD may
emerge as a result of ADHD symptoms is however not clear. It is important to note
that there is likely an interaction between vulnerabilities in emotion regulation,
impulse control, and dysfunctional environment as well as traumatic events that
must occur for BPD to emerge (Crowell, Beauchaine et al. 2009). Additionally, the
developmental progression of childhood ADHD to adult BPD may depend on the
presence of vulnerability and risk factors that have different rates of occurrence
(or different implications) across gender.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
136
CHAPTER 7
Further research should investigate how developmental risk factors, such as
childhood abuse/neglect and attachment disturbances, may differently interact
with childhood ADHD symptoms in influencing the developmental trajectory of
BPD in females versus males. With regard to the outcome in BPD, it is of interest to
note that prospectively designed studies suggest that a favorable outcome depends
more on the presence of favorable personality traits rather than on the absence of
certain symptoms or syndromes (Stone 2016). Three variables associated with an
earlier time-to-recovery are aspects of temperament: being without the avoidance
and dependency of anxious cluster personality disorders as well as exhibiting
higher levels of extraversion and agreeableness. Besides this, it was also found that
the absence of ADHD also significantly predicted earlier time to recovery in
patients with BPD (Zanarini, Frankenburg et al. 2014). In terms of directions for
future research, it would be important to determine the best predictive model for
the recovery of BPD with co-occurring ADHD.
Extreme Novelty Seeking temperament in ADHD might predispose to later co-occurring BPD
In chapter 4 of this thesis we examined the role of temperament and personality
traits in the co-occurrence of ADHD and BPD. We aimed to identify shared and
unique personality characteristics and to gain greater insight in the possible
pathways from early temperament to future ADHD and/or BPD. Previous studies
had already shown that ADHD and BPD seem to share a number of temperament
and character traits but, at that time, neither the comorbid presence of ADHD in
the BPD samples nor the comorbid presence of BPD in the ADHD samples were
controlled for. Chapter 4 shows that, except for those BPD and ADHD patients that
are characterized by a symptom profile with mostly BPD and ADHD hyperactivity
symptoms, all other patients showed significantly above average scores on a
Novelty Seeking (associated with behavioral activation, including impulsivity)
temperament. Novelty Seeking may therefore be more strongly linked to ADHD
and less to BPD. Later research also illustrated that ADHD and ADHD-BPD patients
differed from BPD subjects by a higher level of impulsivity (Prada and Hasler 2014).
However, the Highest Novelty Seeking was found in those ADHD and BPD patients
with symptoms of BPD and symptoms in all areas of ADHD. Thus, an extreme
Novelty Seeking temperament (i.e. a temperament tendency toward impulsivity in
response to novel stimuli) might suggest a vulnerability for the development of
ADHD and co-occurring BPD. This finding seems in line with previous findings
and our own finding in chapter 3; that impulsivity is an important factor in the
development of BPD, in addition to ADHD.
Furthermore, we showed that Harm Avoidance (which is associated with emotional
sensitivity, negative affectivity, behavioral inhibition in response to danger or

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
137
SUMMARY AND GENERAL DISCUSSION
7
novelty and trait anxiety) may be specifically linked to BPD, which is a finding in
keeping with previous findings (Joyce, McKenzie et al. 2003). Later work indeed
shows that temperament/personality traits could mediate the relation between
childhood ADHD and adult BPD features. Impulsivity, aggression, novelty seeking,
and juvenile conduct problems altogether completely mediated the relationship
between retrospective ADHD symptoms and current BPD features (Carlotta,
Borroni et al. 2013). Additionally, in a female sample mediation analyses revealed
that both impulsivity and emotion dysregulation fully mediated the relationship
between childhood ADHD symptoms and current BPD features (Fossati, Gratz et
al. 2015). It has also been suggested that emotion dysregulation is prevalent in
ADHD throughout the lifespan and is a major contributor to impairment (Shaw,
Stringaris et al. 2014). Thus, a Novelty Seeking and Harm Avoidance temperament
might indeed predispose for later BPD features. Moreover, adolescents with BPD
show a strong affinity to self-injurious behavior due to experiencing aversive
emotions as intolerable and impulsively attempt to ameliorate those (Kaess,
Brunner et al. 2014).
The basis for the expression of BPD features in those individuals with an
extreme Novelty Seeking temperament is poorly understood. Theoretically it
could be argued that Novelty Seeking may also play a protective role, as aspects of
Novelty Seeking may also dispose to an active coping style. An orientation toward
approaching novel stimuli and overcoming hurdles to achieve goals may run
counter to the avoidance tendencies that have been proposed to underlie self-injury
in BPD (Chapman, Specht et al. 2005). Indeed, there are indications that Novelty
Seeking is negatively associated with future self-injury among females with BPD,
whereas the role of higher levels of Harm Avoidance may need further examination
(Chapman, Derbidge et al. 2009).
Overall, such findings suggest that difficulties with negative emotionality and
behavioral control represent critical elements in the relationship between
childhood ADHD (symptoms) and BPD (symptoms) in adult women. Future research
could concern the role of the interaction between a child’s personality profile and
his/her family environment in the transition from ADHD to BPD. In this regard,
attachment disturbances are of particular interest. On the one hand, because they
represent another developmental risk factor that has been consistently found to be
associated with BPD (Agrawal, Gunderson et al. 2004; Choi-Kain, Fitzmaurice et al.
2009; Fossati, Borroni et al. 2012). On the other hand, when attachment is strong,
individuals may be more likely to experience belongingness, and thereby are less
likely to engage in self-injury (Chapman, Derbidge et al. 2009).

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
138
CHAPTER 7
ADHD and BPD are associated with distinct impulsive phenotypes While it is clear that there is a behavioral overlap in impulsivity in co-occurring
BPD and ADHD, at the level of symptoms and traits, it is unclear if this involves the
same underlying cognitive process. One such process could be response inhibition
deficits, which were assessed in the continuous performance task (CPT) in ADHD
and BPD patients. Previous research has not convincingly established whether or
not BPD is related to response inhibition deficits independently of ADHD. Chapter 5
demonstrated that response inhibition deficits may be related to BPD independently
of ADHD (in both males and females). In fact, patients with BPD performed
significantly worse than ADHD patients on several CPT indices. Therefore, counter-
intuitively, they may suffer from more widespread inhibition deficiencies than
ADHD patients. Moreover, the BPD patients might be specifically impaired in
context processing (i.e. the mental representation, maintenance and updating of
context information). Context processing is an executive ability that refers to
the adaptive control of behavior through use of prior contextual information
that must be mentally represented and maintained to support context-appropriate
behavior (Cohen and Servan-Schreiber 1992). Context processing thus depends on
several cognitive processes including selective attention, working memory, cognitive
control, and response inhibition. In the CPT task representation and maintenance
of antecedent contextual information relevant to an immediate goal is needed to
overcome an established automatic or pre-potent response. Although our work
may contribute to the growing evidence that executive function deficits play a role
in BPD, the specific domains that may account for these contributions are far less
apparent (McClure, Hawes et al. 2016).
Recent studies have suggested that impulsivity symptoms in BPD may be
stress-dependent or linked with high emotionality and therefore variation in
impulsivity may be explained by state changes. Indeed, even under resting state
conditions, BPD patients demonstrated higher trait and state impulsivity compared
to healthy controls and significant correlations between these self-reported
difficulties in emotion regulation and attentional impulsiveness (Cackowski, Reitz
et al. 2014). Such findings might help interpret our data demonstrating differences
in context processing. Moreover, a recent paper, has suggested that top-down regulation
in ADHD differs in comparison to specific emotional instability disorders including
BPD (Sebastian, Jung et al. 2014) which may underlie differential contextual inter-
pretations in both disorders. However, contradictory findings showed no impairment
in inhibitory function in BPD without ADHD and even enhanced response inhibition
after stress induction in patients with BPD without ADHD compared to healthy
particiapants (Krause-Utz, Sobanski et al. 2013).
More globally, whether brain processes associated with “emotion” can be separated
from those involved in “cognition” is debatable (Okon-Singer, Hendler et al. 2014).

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
139
SUMMARY AND GENERAL DISCUSSION
7
Previous work demonstrates that emotional cues, - states, and – traits can strongly
influence key elements of information processing, including selective attention,
working memory and cognitive control. In turn, circuits involved in attention and
working memory contribute to the voluntary regulation of emotion. The distinction
between the ‘emotional” and the “cognitive” brain is blurry and context dependent
and emotion and cognition seem deeply interwoven together (Okon-Singer,
Hendler et al. 2015). Although ADHD has been classically defined on the basis of
dysfunctional regulation of non-emotional information processing and BPD on
the basis of dysfunctional regulation of emotional processes, it has been recently
proposed that dysregulation in these different dimensions can be incorporated
into one theoretical unified model. This model suggests that ADHD and BPD are
mechanistically related in that they all involve similar dysfunctional top-down
regulation of information processing. The difference is whether this dysfunctional
regulation is related to emotional processing or non-emotional processing. Since
there is substantial overlap between the disorders and a tight relation between
symptoms, in line with a common underlying mechanism for these clinical states,
possibly the best way to describe these states is with traits related to emotional
dysregulation and traits related to non-emotional dysregulation that are combined
to different degrees. Hence, using a dimensional rather than a categorical approach
is recommended, which may both improve our understanding of patients’ needs
and their treatment (Petrovic and Castellanos 2016).
Personality traits are related to clinical symptoms rather than to cognitive profile
In chapter 6 we investigated whether the Five Factor Model (FFM) personality traits
are related to neurocognitive profiles in adults with ADHD and/or healthy controls.
Unfortunately, we could not control for BPD in this study as there was a lack of
sufficient and clear data on BPD diagnosis and symptoms. This impacts on the
ability to discuss the results of chapter 6 in relation to BPD. Therefore, adding to this
discussion, we examined the limited available datasets, i.e. the number of self-
reported BPD symptoms, in relation to the neurocognitive profiles and the FFM traits.
Irrespective of cognitive profile, participants with ADHD showed significantly
higher Neuroticism and lower Extraversion, Agreeableness, and Conscientiousness
than healthy controls. Previous research also showed associations of ADHD with
higher levels of neuroticism and lower levels of conscientiousness and agreeableness
(Nigg, John et al. 2002; Miller, Miller et al. 2008). Findings with regard to extra -
version in ADHD have been inconsistent. Only the FFM personality factor Openness
differed significantly between neurocognitive profiles. Higher Openness was more
common in those with aberrant attention and inhibition than those with increased
delay discounting and atypical working memory / verbal fluency. The results

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
140
CHAPTER 7
suggest that the personality trait Openness, but not any other FFM factor, is linked
to neurocognitive profiles in ADHD. Thus, the presence of ADHD rather than
cognitive profile is associated with personality traits.
With regard to the BPD symptoms, we also found no significant effect of total
number of BPD traits on the cognitive profiles for either the ADHD and the control
group. Of note, 33% of the adults with ADHD had reported five or more BPD features
(compared to 2% of the healthy controls. The cut off of 5 reported traits is used in
clinical practice to initiate full assessment of the existence of BPD. This is in line
with the high frequency of co-occurring ADHD and BPD, as was also the case in
chapter 2 with a frequency of 15% BPD in our ADHD population and 33% ADHD in
our BPD population. The total number of BPD traits showed a significant positive
correlation with Neuroticism, but not with the other four FFM traits. Thus the
more BPD symptoms were reported, the higher the score on the Neuroticism trait.
This finding is consistent with extensive prior literature showing strong positive
associations between phenotypic associations for BPD with Neuroticism. Previous
work also shows that low Agreeableness and low Conscientiousness are consistently
associated with BPD (Widiger and Costa 2002; Kendler, Myers et al. 2011).
With regard to the FFM traits it thus seems that both ADHD and BPD are
associated with high Neuroticism, Low Agreeableness and low Conscientiousness.
Furthermore, there is evidence suggesting genetic correlations for Neuroticism,
Agreeableness and Conscientiousness with BPD characteristics and for Neuroticism
and Conscientiousness with ADHD (Martel, Nikolas et al. 2010; Kendler, Myers et
al. 2011). Thus, ADHD and BPD appear to be linked to similar personality traits.
The underlying basis may however differ. Analyses of the facets of the overall
domains could be quite important and fundamental to the description and
understanding of both ADHD and BPD. For example, it was found that five
personality disorders were meaningfully related to the domain of Neuroticism.
However, facet level analysis indicated that only one of these five personality
disorders correlated significantly with the facet impulsivity (i.e. BPD) (Saulsman
and Page 2004). Therefore, a next step in the understanding of the relation between
ADHD and BPD could be to explore not only domain but also facet scores of the
FFM in both ADHD and BPD patient groups.
Chapter 6 showed no relation between FFM traits and cognitive profile in
adults with ADHD, except for the domain Openness to experience, which was
associated with a cognitive profile mostly characterized by inattention and
disinhibition. This may explain reports, that show that, contrary to the other four
domains of FFM, Openness to experience is poorly related to the DSM personality
disorders and warrants further consideration regarding its conceptualization and
assessment (Samuel and Widiger 2008). Therefore, the finding that Openness is
linked to the cognitive profile in adult ADHD remains to be more fully resolved.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
141
SUMMARY AND GENERAL DISCUSSION
7
The lack of significant interactions between the other cognitive profiles (that
were similar in ADHD and controls) and FFM traits deserves more discussion.
It suggests that personality and cognition are independent entities without
significant influence on each other. The relative influence of emotional processing
on FFM traits may be useful to explore. Given the cross-talk between cognitive and
emotion processing, it would be useful to know to which extent self-reported
symptoms or traits reflect the neurocognitive constructs (that interact with emotion
processing). Recent work in non-clinical samples indicates that self-reports of
executive functioning are minimally related to performance measures of these
cognitive abilities but are consistently associated with Neuroticism (positive) and
Conscientiousness (negatively) (Buchanan 2016). Moreover, exploratory analysis by
the same group showed little to no relationship between FFM traits and objectively
measured executive functions. This may confirm our inability to find associations
between FFM traits and cognitive profiles, in spite of the clear link between ADHD
classification and FFM traits. Research focusing on ADHD also indicate that (self)
ratings of executive problems have greater ecological validity than cognitive tests,
which often do not correlate with the real world problems experienced by the
patient (Barkley and Fischer 2011; Kamradt, Ullsperger et al. 2014). Such findings
lead to the question of the clinical utility of neurocognitive testing and suggest
that it may also be useful to consider personality in the clinical management of
ADHD.
Clinical implications and future directions
Towards a person specific management of their vulnerabilities In this thesis we looked at the symptomatic overlap between ADHD and BPD and
the role of temperament, personality and cognition. Taken together, we may
conclude that the frequent co-occurrence of adult ADHD and BPD can be
understood by the presence of hyperactive/impulsive symptoms and temperament
traits, already inherent in childhood and a probable precursor for a BPD outcome
in adulthood. A difference between both patient groups may reflect the more
harm avoidant temperament in adults with BPD, but both groups are associated
with high Neuroticism traits. Although neurocognitive measurements show
deficiencies in both ADHD and BPD populations, it seems that these cognitive
deficiencies are not so different from those that are found in the whole population.
Rather, they are at a more extreme end of a dimension which can result in
functional problems. Furthermore, specific cognitive profiles do not seem to link
with specific ADHD symptoms nor with personality traits. Hence, the boundaries
between ADHD and BPD remain blurred.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
142
CHAPTER 7
An interesting line of thinking might be that our results are in line with a
network approach. Meaning that the boundaries between both disorders are
unclear not as a result of methodological limitations, but rather as a result of the
intrinsic structure of disorders. Perhaps we should accept that the reason we have
been unable to find true boundaries is because there are no true boundaries. It
seems that no longer can comorbidity be meaningfully explained as a correlation
between two disorders, nor as a result of a common underlying (neurobiological
dysfunction) or “super disorder”. Instead the causal relations between symptoms
constitute pathways that can connect different disorders (Borsboom and Cramer
2013). Such multiple pathways from one disorder to another might exist in such a
way that there is no objective or “true” point at which to dissect the symptom
network in two, with each part representing a different disorder (Cramer, Waldorp
et al. 2010).
The present thesis also provides knowledge of psychopathology beyond and
outside the DSM. DSM might provide a guide to but can hardly be a replacement
for our rich psychopathological tradition. Part of the process of good clinical care
is to explore the experience of our patients. This helps us better understand them
and this sense of shared understanding can be directly therapeutic. Therefore we
need knowledge outside of the DSM in order to fully enable clinical management
(Kendler 2016).
Given this, it is important to map the individual specific symptoms and vul-
nerabilities that cause someone to seek help and to connect with the need that is
expressed by them. Our data suggest that in case of reported ADHD and/or BPD
symptoms it is important to know that hyperactivity/impulsivity symptoms and
traits are of poor diagnostic value in the differentiation of ADHD and BPD and that
inattention symptoms may also not be particularly unique to ADHD. Thus, the
DSM classification may not always be representative for the experiences of the
individual. In other words, they do not represent all the relevant symptoms that
deserve evaluation. The same seems true for emotional instability; a feature mostly
associated with BPD. However, a harm avoidant temperament can also be seen in
combination with what might be classified as mostly ADHD features. Such a
combination of hyperactivity symptoms with a novelty seeking and harm avoidant
temperament might predispose for poor prognostic outcomes and increased risk
of generalization between ADHD and BPD diagnoses. Since ADHD and BPD may
not be discernable categories, the examination of how networks of ADHD and BPD
symptoms in unselected groups of patients interact with networks of personality
traits would be useful. Such a network model could be used to simulate the
generalization of symptom activity through the network to predict future psycho-
pathological states (Goekoop and Goekoop 2014).

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
143
SUMMARY AND GENERAL DISCUSSION
7
Treat a person with difficulties, rather than a DSM classification The current thesis may inform clinical assessment and treatment of ADHD and
BPD. Overall, our research, and that from others, show that both ADHD and BPD
are often characterized by regulation problems in behavior (impulsivity) as well as
regulation problems in emotions (emotional instability). Our results indicated
that ADHD combined with an extreme Novelty Seeking and high Harm Avoidance
temperament might predispose for co-occurring BPD. It could therefore be of
critical importance to assess temperament in children with ADHD in order to
identify those that may be particularly vulnerable and at risk of worsening of their
problems. Consequently, it may be valuable to add the assessment of temperament
in ADHD children to current diagnostic guidelines. In conjunction with this, the
results in this thesis underline the importance of acknowledging that there are no
clear boundaries between developmental disorders (in youth) and personality
(disorders in adulthood).
Without disregarding the usefulness of the DSM system for diagnosis, we
want to make a plea for a more personal and dimensional approach in the
assessment and treatment of the problems that we encounter in clinical practice,
both in children as in adults. Recognizing the evidence that two DSM categories
show overlap not only in their symptoms, but also with regard to temperament
and personality traits, and neurocognitive functioning undeniably calls for a less
categorical perspective. Indeed, recent work suggested that trait models provide
greater specificity in distinguishing personality pathology among those with
childhood and adulthood ADHD (Smith and Samuel 2016).
This thesis also suggests that there is no clear relationship between cognition
and the Five Factor model personality traits in ADHD (with the exception of
Openness). It may be worth determining whether markers of emotional processing
rather than cognitive processing may offer a better match to the FFM scores in
ADHD. In contrast to the accepted role of emotion dysregulation as one of the
primary mechanisms underlying BPD, the role of emotional processing in ADHD
remains relatively unexplored. However, recently emotion dysregulation has been
emphasized as a core feature of ADHD and a significant contributor to the
functional impairment suffered by youth and adults with ADHD (Bunford, Evans
et al. 2014). Generally, emotion dysregulation occurs when an individual fails to
modify an emotional state so as to promote adaptive behaviors that are necessary
to accomplish his/her goals (Thompson 1994). Within the ADHD literature,
emotion dysregulation has been conceptualized as emotional impulsiveness,
difficulty in effortful regulation of induced emotions, and /or difficulty inducing
more acceptable mood states (Bunford, Evans et al. 2015). Meta-analysis of ADHD
and emotion dysregulation in children and adolescents document significant and
strong links between ADHD and emotion reactivity and emotion regulation and to

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
144
CHAPTER 7
a lesser degree emotion understanding (Graziano and Garcia 2016). The link
between emotion dysregulation and ADHD was found to be similar in strength for
boys and girls. Despite the extensive research documenting an association between
emotion dysregulation and BPD, there is also a need to elucidate the precise
emotion regulation deficits that are most relevant (Gratz, Moore et al. 2016). Such
knowledge could contribute to future development of clinical interventions that
more directly target emotion regulation as this may be of importance in improving
the impairments in both ADHD and BPD.
Psychotherapeutic strategies for emotion processing difficulties are commonly
found in the treatment of individuals with BPD. For example: targeting emotional
dysregulation is a key element of Dialectical Behaviour Therapy (DBT). This DBT
treatment has shown to be effective in decreasing inappropriate anger, a reduction
in self-harm and an improvement in general functioning in BPD (Stoffers, Vollm et
al. 2012). Recently it has been recommended that principles of DBT may also
successfully treat ADHD in adults, as adjunct to medication (Asherson, Young et al.
2014). Such skill training approach (i.e. a behavioral approach where painful
emotion can be alleviated through general skills and actions) to emotion regulation
is one that can be applied across distressing situations and largely irrespective of
individual differences (Neacsiu, Eberle et al. 2014). This could therefore be an
important tool that might also help in the coping with some of the ADHD problems.
Another interesting perspective could be that emotional arousal can also be
regulated by qualitatively changing the difficult emotion in question. In this
case, painful emotion is alleviated through the exploration of memories and
idiosyncratic meanings. From this experiential viewpoint, the act of emotion
regulation is essentially a means to another end: allowing one to tolerate emotion
just enough to turn one’s focus inward and complete a distressing but meaningful
task (e.g. exploring and accepting painful material) (Pascual-Leone, Gillespie et al.
2016). Since it is known that attachment difficulties and childhood trauma are not
only related to BPD but also to persistent ADHD (Ferrer, Andion et al. 2016; Storebo,
Rasmussen et al. 2016), this might be a valuable additional strategy in cases that
call for more specific and personal understanding by the patient of their emotions.
Future work should focus on clarifying exactly how, when, and what needs to
be done to help clients to gain the ability to adapt ones responses to match the
situation they are in. This might inform us further on how best to integrate
current research and clinical practice in processing cognitive and emotional
dysregulation in ADHD and BPD.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
145
SUMMARY AND GENERAL DISCUSSION
7
Future research recommendations
This thesis has demonstrated a clear symptomatic overlap in ADHD and BPD cases.
It remains to be resolved whether this overlap is present on a biological level. Such
strategies may be useful to further enlighten the relationship between ADHD and
BPD. Currently the association between ADHD and BPD has primarily been
investigated at the phenotypic level and there is still a lack of sufficient information
about the biological etiology of co-occurring ADHD and BPD.
The high rate of co-occurring ADHD and BPD may suggest a shared genetic
architecture. Indeed, genetic effects behind the shared features of ADHD and BPD
have been suggested (Distel, Carlier et al. 2011; Reif, Nguyen et al. 2011; Weissflog,
Scholz et al. 2013; Weber, Scholz et al. 2014). Although this adds to identifying
unique and shared genetic imprints, larger sample sizes are needed for more
robust results. Furthermore, it has been argued that it is important to shift away
from categorical case-control approaches that view psychiatric disorders as
unitary constructs, towards a dimensional approach that incorporate endo-pheno-
types, or intermediate traits, and bottom-up statistical classification methods
(Hawi, Cummins et al. 2015). Such an approach may help to better characterize the
heterogeneous nature of the disorders and the extent of overlap.
Another genetic research strategy that might be successful in the identification
of common versus unique risk factors for ADHD and BPD could be family-genetic
studies. For example, family genetic research in ADHD and autism spectrum
disorder has built on the idea that polygenic and multifactorial causes of disease
will increase symptom levels in most or all members of the family, whereas
sporadic genetic and non-genetic causes will be strictly personal to the patient
(Oerlemans, Hartman et al. 2015). To our knowledge, such particular attempt has
not yet been made for ADHD and BPD. However, twin family data of a large
population based sample was used to determine whether shared (genetic and
environmental) etiology could explain (part of) the comorbidity between ADHD
symptoms and BPD symptoms (Distel, Carlier et al. 2011). The genetic analysis
showed that the high correlation between BPD and ADHD symptoms could be
explained for 49% by additive genetic factors and for 51% by unique environmental
factors. It thus seems that common biological factors influence both ADHD and
BPD. Further research is needed to investigate the underlying sources of the
genetic and (non) shared environmental factors that influence both ADHD and
BPD symptoms.
Another way of further gaining knowledge about the overlap in ADHD and
BPD might be through brain imaging studies. Brain volume abnormalities are
important indicators of pathophysiological processes that likely reflect disorder
etiology. For ADHD, total brain volume and grey matter volume have been found

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
146
CHAPTER 7
to be decreased compared to typically developing controls (Valera, Faraone et al.
2007; Seidman, Biederman et al. 2011; Frodl and Skokauskas 2012; Greven, Bralten
et al. 2015). With regard to BPD there are also indications of abnormalities in gray
matter (Rossi, Lanfredi et al. 2015; Yang, Hu et al. 2016). No studies to date have
investigated structural correlates between ADHD and BPD. It could be of interest
to investigate whether the extent to which ADHD symptoms occur in BPD (or vice
versa) may have an effect on the brain volumes in ADHD (or BPD).
Lastly, we want to highlight the potential use of pharmacological studies in
dissecting ADHD and BPD traits. Case reports and a small scale study of successful
methylphenidate treatment (the first line treatment in adult ADHD) have been
reported in BPD (Golubchik, Sever et al. 2008). Methylphenidate treatment was
associated with a significant improvement not only in ADHD symptoms but also in
BPD severity, aggressive behavior, and self-injurious behavior. However, the effects
of pharmacological treatments for ADHD and/or BPD have not been investigated in
large scale controlled trials which consider effects on the symptomatic overlap.
More generally, it could be suggested that medication strategies that alter response
inhibition such as methylphenidate, citalopram and atomoxetine may be useful in
the comparison of ADHD and BPD (Nandam, Hester et al. 2014).
Given the multitude of biological substrates deserving of investigation as
candidate mechanisms underlying common ADHD and BPD symptoms, it may be
useful to consider applying the NIH Research Domain Criteria (RDoC) approach to
the study of common ADHD and BPD endophenotypes (Cuthbert 2015; Kozak and
Cuthbert 2016).

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
147
SUMMARY AND GENERAL DISCUSSION
7
References
Agrawal, H. R., J. Gunderson, et al. (2004). “Attachment studies with borderline patients: a review.” Harv
Rev Psychiatry 12(2): 94-104.
Asherson, P., A. H. Young, et al. (2014). “Differential diagnosis, comorbidity, and treatment of attention-
deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality disorder in
adults.” Curr Med Res Opin 30(8): 1657-1672.
Barkley, R. A. and M. Fischer (2011). “Predicting impairment in major life activities and occupational
functioning in hyperactive children as adults: self-reported executive function (EF) deficits versus EF
tests.” Dev Neuropsychol 36(2): 137-161.
Borsboom, D. and A. O. Cramer (2013). “Network analysis: an integrative approach to the structure of psy-
chopathology.” Annu Rev Clin Psychol 9: 91-121.
Buchanan, T. (2016). “Self-report measures of executive function problems correlate with personality, not
performance-based executive function measures, in nonclinical samples.” Psychol Assess 28(4):
372-385.
Bunford, N., S. W. Evans, et al. (2014). “Emotion Dysregulation Is Associated With Social Impairment
Among Young Adolescents With ADHD.” J Atten Disord.
Bunford, N., S. W. Evans, et al. (2015). “ADHD and Emotion Dysregulation Among Children and Adolescents.”
Clin Child Fam Psychol Rev 18(3): 185-217.
Cackowski, S., A. C. Reitz, et al. (2014). “Impact of stress on different components of impulsivity in
borderline personality disorder.” Psychol Med 44(15): 3329-3340.
Carlotta, D., S. Borroni, et al. (2013). “On the relationship between retrospective childhood ADHD symptoms
and adult BPD features: the mediating role of action-oriented personality traits.” Compr Psychiatry
54(7): 943-952.
Chapman, A. L., C. M. Derbidge, et al. (2009). “Temperament as a prospective predictor of self-injury among
patients with borderline personality disorder.” J Pers Disord 23(2): 122-140.
Chapman, A. L., M. W. Specht, et al. (2005). “Borderline personality disorder and deliberate self-harm: does
experiential avoidance play a role?” Suicide Life Threat Behav 35(4): 388-399.
Choi-Kain, L. W., G. M. Fitzmaurice, et al. (2009). “The relationship between self-reported attachment styles,
interpersonal dysfunction, and borderline personality disorder.” J Nerv Ment Dis 197(11): 816-821.
Cohen, J. D. and D. Servan-Schreiber (1992). “Context, cortex, and dopamine: a connectionist approach to
behavior and biology in schizophrenia.” Psychol Rev 99(1): 45-77.
Cramer, A. O., L. J. Waldorp, et al. (2010). “Comorbidity: a network perspective.” Behav Brain Sci 33(2-3):
137-150; discussion 150-193.
Crowell, S. E., T. P. Beauchaine, et al. (2009). “A biosocial developmental model of borderline personality:
Elaborating and extending Linehan’s theory.” Psychol Bull 135(3): 495-510.
Cuthbert, B. N. (2015). “Research Domain Criteria: toward future psychiatric nosologies.” Dialogues Clin
Neurosci 17(1): 89-97.
Distel, M. A., A. Carlier, et al. (2011). “Borderline personality traits and adult attention-deficit hyperactivity
disorder symptoms: a genetic analysis of comorbidity.” Am J Med Genet B Neuropsychiatr Genet
156B(7): 817-825.
Ferrer, M., O. Andion, et al. (2016). “Differences in the association between childhood trauma history and
borderline personality disorder or attention deficit/hyperactivity disorder diagnoses in adulthood.”
Eur Arch Psychiatry Clin Neurosci.
Fossati, A., S. Borroni, et al. (2012). “Predicting borderline personality disorder features from personality
traits, identity orientation, and attachment styles in Italian nonclinical adults: issues of consistency
across age ranges.” J Pers Disord 26(2): 280-297.
Fossati, A., K. L. Gratz, et al. (2015). “The relationship between childhood history of ADHD symptoms and
DSM-IV borderline personality disorder features among personality disordered outpatients: the
moderating role of gender and the mediating roles of emotion dysregulation and impulsivity.” Compr
Psychiatry 56: 121-127.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
148
CHAPTER 7
Frodl, T. and N. Skokauskas (2012). “Meta-analysis of structural MRI studies in children and adults with
attention deficit hyperactivity disorder indicates treatment effects.” Acta Psychiatr Scand 125(2):
114-126.
Goekoop, R. and J. G. Goekoop (2014). “A network view on psychiatric disorders: network clusters of
symptoms as elementary syndromes of psychopathology.” PLoS One 9(11): e112734.
Golubchik, P., J. Sever, et al. (2008). “Methylphenidate in the treatment of female adolescents with
cooccurrence of attention deficit/hyperactivity disorder and borderline personality disorder: a
preliminary open-label trial.” Int Clin Psychopharmacol 23(4): 228-231.
Gratz, K. L., K. E. Moore, et al. (2016). “The role of emotion dysregulation in the presence, associated
difficulties, and treatment of borderline personality disorder.” Personal Disord 7(4): 344-353.
Graziano, P. A. and A. Garcia (2016). “Attention-deficit hyperactivity disorder and children’s emotion
dysregulation: A meta-analysis.” Clin Psychol Rev 46: 106-123.
Greven, C. U., J. Bralten, et al. (2015). “Developmentally stable whole-brain volume reductions and develop-
mentally sensitive caudate and putamen volume alterations in those with attention-deficit/
hyperactivity disorder and their unaffected siblings.” JAMA Psychiatry 72(5): 490-499.
Hawi, Z., T. D. Cummins, et al. (2015). “The molecular genetic architecture of attention deficit hyperactivity
disorder.” Mol Psychiatry 20(3): 289-297.
Helgeland, M. I., E. Kjelsberg, et al. (2005). “Continuities between emotional and disruptive behavior
disorders in adolescence and personality disorders in adulthood.” Am J Psychiatry 162(10): 1941-1947.
Hsu, L. K. (1996). “Epidemiology of the eating disorders.” Psychiatr Clin North Am 19(4): 681-700.
Johnson, D. M., M. T. Shea, et al. (2003). “Gender differences in borderline personality disorder: findings
from the Collaborative Longitudinal Personality Disorders Study.” Compr Psychiatry 44(4): 284-292.
Joyce, P. R., J. M. McKenzie, et al. (2003). “Temperament, childhood environment and psychopathology as
risk factors for avoidant and borderline personality disorders.” Aust N Z J Psychiatry 37(6): 756-764.
Kaess, M., R. Brunner, et al. (2014). “Risk-behaviour screening for identifying adolescents with mental
health problems in Europe.” Eur Child Adolesc Psychiatry 23(7): 611-620.
Kamradt, J. M., J. M. Ullsperger, et al. (2014). “Executive function assessment and adult attention-deficit/
hyperactivity disorder: tasks versus ratings on the Barkley deficits in executive functioning scale.”
Psychol Assess 26(4): 1095-1105.
Kendler, K. S. (2016). “The Phenomenology of Major Depression and the Representativeness and Nature of
DSM Criteria.” Am J Psychiatry 173(8): 771-780.
Kendler, K. S., J. Myers, et al. (2011). “Borderline personality disorder traits and their relationship with
dimensions of normative personality: a web-based cohort and twin study.” Acta Psychiatr Scand
123(5): 349-359.
Kozak, M. J. and B. N. Cuthbert (2016). “The NIMH Research Domain Criteria Initiative: Background, Issues,
and Pragmatics.” Psychophysiology 53(3): 286-297.
Krause-Utz A., Sobanski E. et al. (2013). Impulsivity in relation to stress in patients with borderline
personality disorder with and without co-occurring attention-deficit/hyperactivity disorder: an
exploratory study. J Nerv Ment Dis. 201(2):116-123.
Martel, M. M., M. Nikolas, et al. (2010). “Personality mediation of genetic effects on Attention- Deficit/
Hyperactivity Disorder.” J Abnorm Child Psychol 38(5): 633-643.
McClure, G., D. J. Hawes, et al. (2016). “Borderline personality disorder and neuropsychological measures of
executive function: A systematic review.” Personal Ment Health 10(1): 43-57.
Miller, C. J., J. D. Flory, et al. (2008). “Childhood attention-deficit/hyperactivity disorder and the emergence
of personality disorders in adolescence: a prospective follow-up study.” J Clin Psychiatry 69(9): 1477-1484.
Miller, C. J., S. R. Miller, et al. (2008). “Personality characteristics associated with persistent ADHD in late
adolescence.” J Abnorm Child Psychol 36(2): 165-173.
Nandam, L. S., R. Hester, et al. (2014). “Dissociable and common effects of methylphenidate, atomoxetine
and citalopram on response inhibition neural networks.” Neuropsychologia 56: 263-270.
Neacsiu, A. D., J. W. Eberle, et al. (2014). “Dialectical behavior therapy skills for transdiagnostic emotion
dysregulation: a pilot randomized controlled trial.” Behav Res Ther 59: 40-51.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
149
SUMMARY AND GENERAL DISCUSSION
7
Nigg, J. T., O. P. John, et al. (2002). “Big five dimensions and ADHD symptoms: links between personality
traits and clinical symptoms.” J Pers Soc Psychol 83(2): 451-469.
Oerlemans, A. M., C. A. Hartman, et al. (2015). “Simplex and multiplex stratification in ASD and ADHD
families: a promising approach for identifying overlapping and unique underpinnings of ASD and
ADHD?” J Autism Dev Disord 45(3): 645-657.
Okon-Singer, H., T. Hendler, et al. (2014). “Introduction to the special research topic on the neurobiology of
emotion-cognition interactions.” Front Hum Neurosci 8: 1051.
Okon-Singer, H., T. Hendler, et al. (2015). “The neurobiology of emotion-cognition interactions: fundamental
questions and strategies for future research.” Front Hum Neurosci 9: 58.
Pascual-Leone, A., N. M. Gillespie, et al. (2016). “Measuring Subtypes of Emotion Regulation: From Broad
Behavioural Skills to Idiosyncratic Meaning-making.” Clin Psychol Psychother 23(3): 203-216.
Petrovic, P. and F. X. Castellanos (2016). “Top-Down Dysregulation-From ADHD to Emotional Instability.”
Front Behav Neurosci 10: 70.
Prada P., Hasler R. et al. (2014). Distinguishing borderline personality disorder from adult attention deficit/
hyperactivity disorder: a clinical and dimensional perspective. Psychiatry Res. 217:107-114.
Reif, A., T. T. Nguyen, et al. (2011). “DIRAS2 is associated with adult ADHD, related traits, and co-morbid
disorders.” Neuropsychopharmacology 36(11): 2318-2327.
Rossi, R., M. Lanfredi, et al. (2015). “Abnormalities in cortical gray matter density in borderline personality
disorder.” Eur Psychiatry 30(2): 221-227.
Samuel, D. B. and T. A. Widiger (2008). “A meta-analytic review of the relationships between the five-factor
model and DSM-IV-TR personality disorders: a facet level analysis.” Clin Psychol Rev 28(8): 1326-1342.
Saulsman, L. M. and A. C. Page (2004). “The five-factor model and personality disorder empirical literature:
A meta-analytic review.” Clin Psychol Rev 23(8): 1055-1085.
Sebastian, A., P. Jung, et al. (2014). “Frontal dysfunctions of impulse control - a systematic review in
borderline personality disorder and attention-deficit/hyperactivity disorder.” Front Hum Neurosci 8:
698.
Seidman, L. J., J. Biederman, et al. (2011). “Gray matter alterations in adults with attention-deficit/
hyperactivity disorder identified by voxel based morphometry.” Biol Psychiatry 69(9): 857-866.
Shaw, P., A. Stringaris, et al. (2014). “Emotion dysregulation in attention deficit hyperactivity disorder.” Am
J Psychiatry 171(3): 276-293.
Smith T.E. and Samuel D.B. (2016). A Multi-Method Examination of the Links Between ADHD and
Personality Disorder. J Pers Disord. 4:1-23.
Stepp, S. D., J. D. Burke, et al. (2012). “Trajectories of attention deficit hyperactivity disorder and oppositional
defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent
girls.” J Abnorm Child Psychol 40(1): 7-20.
Stoffers, J. M., B. A. Vollm, et al. (2012). “Psychological therapies for people with borderline personality
disorder.” Cochrane Database Syst Rev(8): CD005652.
Stone, M. H. (2016). “Long-Term Course of Borderline Personality Disorder.” Psychodyn Psychiatry 44(3):
449-474.
Storebo, O. J., P. D. Rasmussen, et al. (2016). “Association Between Insecure Attachment and ADHD:
Environmental Mediating Factors.” J Atten Disord 20(2): 187-196.
Thompson, R. A. (1994). “Emotion regulation: a theme in search of definition.” Monogr Soc Res Child Dev
59(2-3): 25-52.
Torgersen, S., E. Kringlen, et al. (2001). “The prevalence of personality disorders in a community sample.”
Arch Gen Psychiatry 58(6): 590-596.
Valera, E. M., S. V. Faraone, et al. (2007). “Meta-analysis of structural imaging findings in attention-deficit/
hyperactivity disorder.” Biol Psychiatry 61(12): 1361-1369.
Weber, H., C. J. Scholz, et al. (2014). “SPOCK3, a risk gene for adult ADHD and personality disorders.” Eur
Arch Psychiatry Clin Neurosci 264(5): 409-421.
Weissflog, L., C. J. Scholz, et al. (2013). “KCNIP4 as a candidate gene for personality disorders and adult
ADHD.” Eur Neuropsychopharmacol 23(6): 436-447.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
150
CHAPTER 7
Widiger, T. A. and P. T. Costa (2002). Five factor model personality disorder research. Personality Disorders
and the Five Factor Model of Personality. P. T. Costa and T. A. Widiger. Washingtin DC, American
Psychological Association: 59-87.
Yang, X., L. Hu, et al. (2016). “Default mode network and frontolimbic gray matter abnormalities in patients
with borderline personality disorder: A voxel-based meta-analysis.” Sci Rep 6: 34247.
Zanarini, M. C., F. R. Frankenburg, et al. (1998). “Axis I comorbidity of borderline personality disorder.”
Am J Psychiatry 155(12): 1733-1739.
Zanarini, M. C., F. R. Frankenburg, et al. (2014). “Prediction of time-to-attainment of recovery for borderline
patients followed prospectively for 16 years.” Acta Psychiatr Scand 130(3): 205-213.
Zlotnick, C., L. Rothschild, et al. (2002). “The role of gender in the clinical presentation of patients with
borderline personality disorder.” J Pers Disord 16(3): 277-282

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
151
SUMMARY AND GENERAL DISCUSSION
7

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
Nederlandse samenvattingList of publications
DankwoordCurriculum Vitae

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
155
NEDERLANDSE SAMENVATTING
Nederlandse samenvatting
ADHDADHD staat voor ‘Attention-Deficit Hyperactivity Disorder’ en is een ontwikkelings-
stoornis die gekenmerkt wordt door de aanwezigheid van een hardnekkig patroon
van onoplettendheid en/of hyperactiviteit en impulsiviteit dat leidt tot functionele
belemmeringen. Lange tijd zag men ADHD als een stoornis in de kindertijd met
beperkt effect op de volwassenheid. Inmiddels weten we dat bij tot wel 50% van de
kinderen met ADHD de symptomen en functionele beperkingen voortduren in de
volwassenheid. Volwassenen met ADHD hebben veelal nog bijkomende psychische
en/of psychiatrische problemen. Dit wordt co-morbiditeit genoemd. Het betreft
vooral andere ontwikkelingsstoornissen zoals autismespectrumstoornissen, maar
ook angst- en stemmingsstoornissen, middelenmisbruik, gedragsstoornissen en
persoonlijkheidsstoornissen. Het begrijpen van de overeen komsten en verschillen
met stoornissen die vaak samen met ADHD voorkomen is van belang om onder-di-
agnostiek (of foutieve diagnostiek) van ADHD te voorkomen en kan bijdragen aan
het inzetten van passende behandelinterventies.
Borderline persoonlijkheidsstoornisDe borderline persoonlijkheidsstoornis (BPS) wordt gekenmerkt door een hardnekkig
en uitgebreid patroon van instabiliteit in de emotieregulatie, interpersoonlijke
relaties en zelfbeeld, en verhoogde impulsiviteit. Hoewel de diagnose BPS per
definitie niet voor de adolescentie gesteld kan worden laat onderzoek zien dat het
klinische beeld ook bij jongeren een valide construct is. Ook bij BPS is sprake van
onder-diagnostiek. Er is een grote overlap van symptomen met bijvoorbeeld
depressieve stoornissen, impulsiviteitsstoornissen en identiteitsstoornissen. Dit
kan het in de praktijk moeilijk maken om vast te stellen of de symptomen horen
bij de BPS of bij een co-morbide stoornis. Ook hier geldt dat het begrijpen van de
overeenkomsten en verschillen met stoornissen waarmee BPS vaak samen
voorkomt van belang is om onder-diagnostiek te voorkomen en bij te dragen aan
het inzetten van passende behandelinterventies.
Overlap tussen ADHD en BPSIn de klinische praktijk kan het soms moeilijk zijn om ADHD en BPS van elkaar te
onderscheiden. Symptomen als impulsiviteit, emotionele instabiliteit, risicovol
gedrag, moeite om boosheid te controleren zijn kenmerken die zowel bij ADHD als
bij BPS worden gezien. Impulsiviteit is een van de meest kenmerkende overlappende
symptomen. Maar ook emotionele instabiliteit en interpersoonlijke problemen,
beiden belangrijke kenmerken van BPS, worden herkend als bijkomende problemen
bij ADHD. Beide stoornissen kennen een chronisch beloop en bovendien komen

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
156
NEDERLANDSE SAMENVATTING
ADHD en BPS vaak samen voor in de klinische praktijk. De oorsprong van de
relatie tussen ADHD en BPS wordt echter nog niet goed begrepen.
Het doel van het onderzoek in dit proefschriftHet doel van het onderzoek in dit proefschrift is het kritisch beschouwen van de
overeenkomsten (en verschillen) tussen ADHD bij volwassenen en de borderline
persoonlijkheidsstoornis en daarmee een bijdrage te leveren aan het beter
begrijpen van de relatie tussen beide stoornissen. We hebben gekeken naar de
overlap op het gebied van symptomen, persoonlijkheidstrekken, en neurocognitie.
In hoofdstuk 2 presenteren we een literatuurstudie naar ADHD, persoonlijkheids-
stoornissen, en persoonlijkheidstrekken. In hoofdstuk 3 werd er een Latente
Klasse Analyse uitgevoerd bij volwassen vrouwen met ADHD en/of BPS om van
elkaar te onderscheiden groepen met homogene symptoomprofielen te identificeren.
In hoofdstuk 4 onderzochten we de rol van temperament en karaktertrekken in
het onderscheiden van volwassen vrouwen met gelijke ADHD en BPS symptoom-
profielen. Ook keken we naar mogelijke ontwikkelingstrajecten van temperament
naar toekomstig ADHD en/of BPS uitkomsten. In hoofdstuk 5 onderzochten we of
een cognitieve maat van respons inhibitie kon differentiëren tussen volwassenen
met ADHD, BPS en gezonde controles. In hoofdstuk 6 bestudeerden we de interacties
tussen cognitieve profielen in volwassenen met ADHD en persoonlijkheidstrekken.
Belangrijkste bevindingen uit dit proefschriftHoofdstuk 2, een literatuuronderzoek, behandelt en bespreekt diverse concepten
en thema’s die betrekking hebben op de relatie tussen ADHD, persoonlijkheids-
stoornissen en persoonlijkheidstrekken. Een belangrijke conclusie was dat eerdere
studies naar ADHD en persoonlijkheid geen rekening hielden met co-morbide
persoonlijkheidsstoornissen bij de ADHD waardoor het moeilijk is specifieke
conclusies te trekken over de overlap en verschillen tussen ADHD, persoonlijk-
heidsstoornissen en persoonlijkheidstrekken. We concludeerden daarom ook dat
meer onderzoek nodig is om de relatie tussen ADHD en persoonlijkheidsstoornis-
sen (meer specifiek de borderline persoonlijkheidsstoornis) beter te gaan begrijpen
en hun gedeelde kenmerken beter te ontrafelen.
In hoofdstuk 3 hebben we kwalitatief verschillende symptoomprofielen van
zowel ADHD in de kindertijd als volwassen leeftijd en BPS symptomen bij volwassen
vrouwen met ADHD en/of BPS geïdentificeerd. We illustreerden dat elke volwassen
vrouw met BPS in ons onderzoek enkele ADHD symptomen had in de kindertijd en
volwassenheid en dat hyperactiviteit karakteristiek is voor zowel volwassen vrouwen
met ADHD als BPS. Hier hebben we ook laten zien dat hyperactiviteit mogelijk een
mediërende rol speelt tussen ADHD en de ontwikkeling van BPS. Concluderend
stelden we daarom dat hyperactiviteit/impulsiviteit weinig discriminatieve

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
157
NEDERLANDSE SAMENVATTING
waarde heeft voor ADHD en BPS. Het onderzoek in hoofdstuk 3 heeft bijgedragen
aan een groeiend bewijs dat ADHD en BPS waarschijnlijk, maar niet alleen, aan
elkaar gerelateerd zijn via hyperactiviteit/impulsiviteit kenmerken. Of BPS ook
ontstaat uit de ADHD symptomen is niet helder.
In hoofdstuk 4 hebben we laten zien dat een opvallend uitgesproken ‘Prikkel-
zoekend’ temperament een kwetsbaarheid suggereert voor de ontwikkeling van
een ADHD met co-morbide BPS bij vrouwen. Daarnaast vonden we dat een ‘Leed-
vermijdend’ temperament meer specifiek geassocieerd zou kunnen zijn met BPS.
Deze bevinding komt overeen met later werk waaruit bleek dat impulsiviteit,
maar ook emotie-disregulatie, de relatie tussen ADHD symptomen in de kindertijd
en volwassen BPS kenmerken volledig medieerde. Zulke bevindingen suggereren
dat moeilijkheden met negatieve emoties en gedragscontrole kritische elementen
zijn in de relatie tussen ADHD symptomen in de kindertijd en BPS symptomen in
de volwassenheid.
In hoofdstuk 5 hebben we onderzocht of ADHD en BPS ook overlappen in
onderliggende cognitieve problemen of dat ADHD en BPS van elkaar te
onderscheiden zijn op het niveau van cognitieve processen. We hebben laten zien
dat onafhankelijk van de aanwezigheid van ADHD, respons-inhibitieproblemen
ook gerelateerd zijn aan BPS. Bovendien bleek dat de groep met BPS meer en meer
specifieke inhibitieproblemen had dan de ADHD groep. Hoewel ons werk hiermee
bijdraagt aan groeiend bewijs dat executieve functie beperkingen een rol spelen in
BPS, is nog erg onduidelijk wat aan deze beperkingen ten grondslag ligt.
Samenvattend lijkt het er op dat ADHD en BPS kenmerken van hyperactiviteit
en impulsiviteit delen op het niveau van symptomen, persoonlijkheidstrekken en
neurocognitieve prestaties. Een interessante vraag die hieruit volgt is of deze
klinische kenmerken, persoonlijkheidstrekken en neurocognitieve prestaties aan
elkaar gerelateerd zijn. In hoofdstuk 6 hebben we laten zien dat alleen de persoon-
lijkheidstrek ‘openheid’, maar geen enkele andere persoonlijkheidstrek uit het vijf
factoren model van persoonlijkheid, gerelateerd was aan neurocognitieve
profielen in ADHD. Juist de aanwezigheid van ADHD, en niet het cognitieve profiel,
was geassocieerd met persoonlijkheidstrekken. Onze bevindingen, en die van
anderen, leiden tot de vraag hoe klinisch bruikbaar neurocognitief testen is en
suggereert dat het nuttig zou kunnen zijn persoonlijkheid mee te nemen in de
diagnostiek en behandeling van ADHD.
Klinische implicatiesWe kunnen concluderen dat het frequent samen voorkomen van ADHD en BPS
begrepen kan worden vanuit de aanwezigheid van hyperactiviteit en impulsiviteit
symptomen en persoonlijkheidstrekken die al aanwezig zijn in de kindertijd en
een mogelijke precursor zijn voor BPS in de volwassenheid. Deze kenmerken

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
158
NEDERLANDSE SAMENVATTING
blijken dus niet uniek voor ADHD. Een verschil tussen beide stoornissen kan een
meer ‘Leedvermijdend’ temperament bij vrouwen met BPS zijn. De rol van emotionele
disregulatie in ADHD is nog relatief onbekend, maar er zijn aanwijzingen dat
emotionele disregulatie, net zoals bij BPS, ook sterk geassocieerd is met ADHD.
Kortom, de afgrenzingen tussen ADHD en BPS blijven vaag.
Het onderzoek in dit proefschrift heeft kennis gegenereerd in aanvulling op
de kennis uit de DSM en dit is van belang voor goede klinische zorg. Het kan helpen
om het individu beter te begrijpen.
Omdat ADHD en BPS niet zo eenvoudig van elkaar te onderscheiden zijn en
de DSM classificatie mogelijk niet altijd representatief voor de ervaring van een
individu is het belangrijk om de individuele symptomen en kwetsbaarheden
waarvoor iemand hulp vraagt in kaart te brengen en hierbij aan te sluiten. Het kan
waardevol zijn om bij de assessment van ADHD ook temperament te onderzoeken.
De resultaten van het onderzoek in dit proefschrift onderstrepen bovendien dat
er geen duidelijke grenzen zijn tussen ontwikkelingsstoornissen (in de kindertijd)
en persoonlijkheidsstoornissen (in de volwassenheid). Zonder tekort te willen
doen aan DSM systeem willen we pleiten voor een meer persoonlijke en dimensionele
aanpak in de diagnostiek en behandeling van de problemen waar individuen
zich mee melden in de klinische praktijk.
Toekomstig onderzoekHet onderzoek in dit proefschrift heeft aangetoond dat er een duidelijke
symptomatische overlap is tussen ADHD en BPS. Het is echter nog onduidelijk of
deze overlap ook aanwezig is op een biologisch niveau. Het is gesuggereerd dat er
genetische effecten zitten achter de gedeelde kenmerken van ADHD en BPS, maar
meer onderzoek is nodig voor sterkere resultaten. Naast genetische studies zouden
ook beeldvormend onderzoek (brain imaging studies) en farmacotherapie studies
een bijdragen kunnen leveren aan het beter begrijpen van de relaties tussen ADHD
en BPS. Gezien de diverse mogelijke biologische substraten zou het nuttig kunnen
zijn om de NIH Research Domain Criteria (RDoC) methode toe te passen op de
studie naar ADHD en BPS.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
159
LIST OF PUBLICATIONS
List of publications
Articles
Van Dijk, F.E., Mostert, J., Onnink, M., Dammers, J., Arias Vasquez, A., Kan, C., Verkes, R.J., Hoogman, M.,
Franke, B., Buitelaar, J. (2016). Five Factor Model personality traits relate to adult attention-deficit/
hyperactivity disorder but not to their distinct neurocognitive profiles (under review)
Van Dijk, F.E., Schellekens, A.F.A., Van Den Broek, P., Kan, C.C., Verkes, R.J., Buitelaar, J.K.. (2014). Do
cognitive measures of response inhibition differentiate between attention deficit/hyperactivity
disorder and borderline personality disorder? Psychiatry Res 215(3): 733-739.
Van Dijk, F. E., Lappenschaar, M., Verkes, R.J., Kan, C.C., Buitelaar, J.K. (2012). Symptomatic overlap between
attention-deficit/hyperactivity disorder and borderline personality disorder in women: the role of
temperament and character traits. Compr Psychiatry 53(1): 39-47.
Pilgrim, D., Champion, F., Hutschemaekers, G.J.M., Garnoussi, N., Van Dijk, F.E. (2012),”Variations in the
development of psychological therapy in three European Union countries”, The International journal
of sociology and social policy; 32 (1): 70-82
Van Dijk, F.E., Lappenschaar, M., Verkes, R.J., Kan, C.C., Buitelaar, J.K. (2011). Lifespan attention deficit/
hyperactivity disorder and borderline personality disorder symptoms in female patients: a latent
class approach. Psychiatry Res 190(2-3): 327-334.
Van Dijk, F.E. Procesbepalende Factoren in Strategische Allianties tussen Universitair Medische Centra en
Algemene Instellingen voor Geestelijke Gezondheidszorg: een Exploratieve Gevalsstudie. 2008.
Intern gebruik Pro Persona.
Bookchapters
Hutschemaekers, G.J.M. & Van Dijk, F.E. Psychotherapy and Clinical psychology in the Netherlands: The
settlement of five distinctive psy professions. In: Handbook of Counseling and Psychotherapy in an
International Context. Ed. Moodley R, Gielen UP, Wu R. 2012. Routledge.
Van Dijk, F.E. & Anckarsäter, H. ADHD, personality, and its disorders. In: ADHD in Adults: Characterization,
Diagnosis, and Treatment. Ed. Buitelaar JK, Kan CC., Asherson, P. 2011. Cambridge University Press.
Hutschemakers, GJM & Van Dijk, F.E. Klinische psychologie en geestelijke gezondheidszorg. In Psychologie
en Praktijk. Kessels, Hutschemakers, Beckers. 2010. Boom Lemma, Den Haag.
Moene, F.C., Sandijck, P., Spinhoven, P.H., Hoogduin, C.A.L., van Dijk, F.E. & Redert, J.F.M. (2001). Assessment
of conversion disorder, motor type: development, reliability and validity of a video rating scale for
motor conversion symptoms. In: Hypnosis and conversion disorder: assessment and treatment issues.
F.C. Moene. 2001. Cure & Care Uitgeverij, Zeist.
Conference presentations (posters and abstracts)
Van Dijk, FE. Psychotherapie als professie. Oral presentation, Nacholing psychiatrie, PAOG, Januari 2011,
Nijmegen, The Netherlands
Van Dijk, F.E. & Hutschemakers, G.J.M. Psychotherapy in the Netherlands: 1986 - 2010. Oral presentation,
Meeting of CERMES3- CESAMES (La psychothérapie en Europe, spécificités nationales et tendances
communes). September 2010. Paris (ENS), France.
Van Dijk F.E. ADHD bij volwassenen. Oral presentation, Congres NIP. 2006, Utrecht, The Netherlands
Van Dijk F.E. ADHD bij volwassenen: Afgrenzing van en overlap met persoonlijkheidsstoornissen. Oral
presentation, symposium. 2006, Zwolle, The Netherlands
Van Dijk, F.E., Kan C.C., Buitelaar J.K. Temperament en karakter in ADHD en de borderline persoonlijk-
heidsstoornis. Oral presentation, Annual meeting of the Dutch psychiatry association (NVvP), April
2006, The Netherlands.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
160
LIST OF PUBLICATIONS
Van Dijk, F.E., Kan C.C., Buitelaar J.K. Borderline persoonlijkheidsstoornis of ADHD? Oral presentation,
Annual meeting of the Dutch psychiatry association, April 2005, The Netherlands.
Van Dijk F.E., Kan C.C., Buitelaar J.K. ADHD and comorbid borderline and antisocial personality disorder.
Poster presentation, European Conference on ADHD and comorbidities in Adults, 2003, Oslo Norway.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
161
DANKWOORD
Dankwoord
Dit proefschrift zou nooit tot stand zijn gekomen zonder de hulp van vele anderen.
Ik ben dan ook iedereen heel erg dankbaar die heeft bijgedragen aan een lang
proces waarvan het einde nu in zicht is gekomen. Speciaal geldt dat voor de
proefpersonen die mij hun tijd en inzet hebben gegeven. Mensen met ADHD en/of
een borderline persoonlijkheidsstoornis, die ondanks hun zorgen en problemen
mee hebben willen werken in het belang van de wetenschap. Zonder hen was mijn
onderzoek sowieso niet mogelijk geweest.
Beste promotoren en copromotoren,
Natuurlijk wil ik jullie heel erg bedanken. Zonder jullie was er geen begin en zeker
ook geen eind gekomen aan dit proefschrift.
Jan Buitelaar, wij leerden elkaar kennen toen jij naar Nijmegen kwam. Ik wilde
onderzoek doen naar ADHD en de borderline persoonlijkheidsstoornis en jij bood
me die mogelijkheid. Dat zie ik nog steeds als een groot voorrecht. Toch hadden bij
mij andere werkzaamheden of privé omstandigheden altijd voorrang en zo werd
het een bijzonder lang(zaam) proces waarin het promotietraject mijn ondergeschoven
kindje werd. Ik heb de afgelopen jaren meermalen overwogen om het bijltje erbij
neer te gooien, maar jouw reactie was steeds: je bent er bijna, je moet nu niet
stoppen. Jij was voor mij de constante factor en als ik dan na lange tijd weer met
een zoveelste concepttekst aankwam en het toch wel graag zo snel mogelijk terug
wilde dan kreeg ik dat ook. Heel bijzonder. Jan, dankjewel voor jouw hulp, je geduld,
en je vertrouwen! Het is er uiteindelijk dan toch van gekomen.
Robbert-Jan Verkes, hoewel niet vanaf het begin betrokken bij mijn promotie-
traject heb je een hele belangrijke rol gespeeld op cruciale momenten. Je bleef
geïnteresseerd en steeds bereid om bij te dragen. Ik heb jou als bijzonder steunend
ervaren. Dankjewel daarvoor.
Cees Kan, het is alweer lang geleden, maar wij hebben samen en met anderen de
ADHD/ASS poli op de afdeling psychiatrie vormgegeven. Zo ontstond de mogelijkheid
voor mij om data te gaan verzamelen. Een essentiële samenwerking.
Jeffrey Glennon, wat ben ik blij dat Jan jou in de laatste fase van het schrijven
van mijn proefschrift heeft gevraagd om mij te ondersteunen. Samen met jou is
het snel gelukt om tot een afronding te komen. Dankjewel.
Beste werkgevers,
Dank aan het Radboud UMC (afdeling psychiatrie), GGz Nijmegen (inmiddels Pro
Persona), de Radboud Universiteit (Faculteit Sociale Wetenschappen). Dank voor
jullie bereidheid om me toch steeds wat tijd te gunnen om weer een paar stappen
verder te komen in mijn promotietraject. Dank ook aan mijn huidige werkgevers

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
162
DANKWOORD
GGNet en Streekziekenhuis Koningin Beatrix. Ook jullie support heb ik gekregen
bij de laatste loodjes.
Beste manuscript- en promotiecommissieleden,
Judith Prins, Paul Hodiamont, en Sandra Kooij. Dank voor jullie bereidheid om
mijn proefschrift te beoordelen en voor de verleende toegang tot de promotie.
Sandra, speciaal dank aan jou. Jij zette me op het spoor van Jan en daar begon het
allemaal mee.
Dank ook aan Anna Bosman, Toon Cillissen en Theo Ingenhoven voor jullie
deelname aan de promotiecommissie.
Beste onderzoeksmaatjes,
Martijn Lappenschaar, Arnt Schellekens en Pieter van den Broek. Dank voor jullie
samenwerking en inzet. Zonder jullie hulp en vooral ook statistische kennis had
ik het echt niet gered. Onderzoeksassistenten Marjan Knippenberg en Marleen
Bastiaanse, dank voor jullie hulp en inzet bij het verzamelen van de data.
Beste (oud) collega’s,
Cees Clarijs en Maurice Bracelly. Opleider en collega’s van het eerste uur in mijn
tijd bij GGz Nijmegen. Dank voor jullie steun en blijvende betrokkenheid. Gelukkig
zien we elkaar nog regelmatig bij de Nijmeegse nascholingen.
Cees van der Staak en Giel Hutschemaekers. Dankzij jullie kreeg ik 2 prachtige
banen binnen het Academisch Centrum Sociale Wetenschappen en maakte daarmee
een geweldige stap in mijn loopbaan. Het heeft me gebracht waar ik nu sta. Dank
voor jullie steun en vertrouwen.
Harold Beckering. Jouw deur stond altijd voor mij open. Een mentor pro bono
zou ik willen zeggen. Jij gaf me de volgende opdracht: “als iemand aan je vraagt
hoe het met je proefschrift staat dan zeg je alleen maar: goed, ik ben er mee bezig”.
En dat hielp! Dankjewel voor jouw steun.
Anna Bosman, lieve Anna, wat ben jij er voor mij geweest de afgelopen 2 jaar.
Dank voor je hulp en steun bij de laatste loodjes.
Dank ook aan alle andere betrokken oud collega’s van GGz Nijmegen, van het
Radboud UMC, van het SPON, van de Faculteit Sociale Wetenschappen, het onder-
wijsinstituut Pedagogische Wetenschappen en Onderwijskunde, en van het
Ambulatorium. Jullie zijn met te veel om op te noemen. Dank voor jullie blijvende
interesse en steun. Maar ook mijn nieuwe collega’s bij GGnet en het Streekzieken-
huis Koningin Beatrix. Wat een warm bad ben ik in terecht gekomen. Dank voor
jullie enthousiasme en vertrouwen.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
163
DANKWOORD
Ik wil ook mijn intervisiegenoten bedanken, nieuw en oud. Ik ben heel blij dat
ik altijd bij jullie terecht kan en kon. Dank voor jullie luisterend oor, de steun, en
goede adviezen.
Lieve vrienden,
Wim, heel wat uurtjes hebben we samen doorgebracht en vooral heel veel gelachen.
ADHD bij volwassenen op de kaart van GGz Nijmegen gezet. Samen naar Sandra
om ons te specialiseren in de ADHD. Collega’s zijn we niet meer, maar vrienden
zijn we gebleven.
Rob, het is in al die jaren misschien maar 2 of 3 keer geweest dat ik je mening
vroeg over een analyse, maar bij jou durfde ik mijn ‘domme’ vragen gewoon te
stellen en kon dan weer verder. Dankjewel dat je er op die momenten voor me was.
Mirella, ineens was je daar en hoe! Vriendin en trainer, met een dijk van
een ‘Mindset’. Hoe is me niet helemaal duidelijk, maar zeker is wel dat jij hebt
bijgedragen aan het feit dat ik het proefschrift toch heb afgemaakt, dat ik weer
aan het tennissen ben, en dat er inmiddels een prachtige lieve Collie bij ons woont.
Dankjewel.
Hetty, Hans, en Jeske. Lieve Hetty, wat hebben we veel gedeeld. Helaas maak je
mijn promotie niet meer mee. Maar het is mede jouw kracht en positieve energie
die mij er toe hebben aangezet om het proefschrift nu toch echt eens af te maken.
Dankjewel lieverd voor onze tijd samen. Het was, in jouw woorden, goud waard!
Hans, rots in de branding. Die extra uurtjes om de discussie te schrijven was
precies wat nodig was. Jeske, lieve schat, weet dat ook jij er aan hebt bijgedragen
dat er toch een promotiedag is gekomen. Al jouw fijne knuffels geven mij zoveel
energie dat het toch gelukt is om het proefschrift af te maken.
Dominique. Wat ben ik blij en dankbaar dat ik jou en Ris mag en kan onder -
steunen. Ook dat was een hele goede stimulans om mijn proefschrift uiteindelijk
snel af te ronden. Ik hoop dat we nog veel fijne momenten zullen hebben samen.
Esther, lieve Esther, jou noem ik als laatste, dankjewel dat wij al jaren altijd
lief en leed kunnen delen en dat je nu mijn paranimf wil zijn en me helpt met alle
voorbereidingen voor mijn promotiedag. Heel bijzonder.
Lieve familie,
Peter en Ludie, al 25 jaar mijn schoonouders. Elvira, Gerhald, Floor en Mila; mijn
schoonzusje, zwager en nichtjes. Bedankt voor alles wat jullie voor ons betekend
hebben in al die jaren. Ik ben heel blij met jullie.
Pap en mam, al 43 jaar mijn ouders, en jullie staan nog altijd voor ons klaar.
Dank voor alles wat jullie voor mij betekend hebben, dat is meer dan ik hier
opschrijven kan. Ik ben heel blij en dankbaar dat we mijn promotie samen kunnen
vieren!

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
164
DANKWOORD
Edwin en Sylvia, broer en schoonzus, we zien elkaar niet veel maar op belangrijke
momenten zijn jullie er. Dankjewel daarvoor.
Robin, mijn grote broer, dank dat je altijd trots op me bent. Dat voelt fijn. Weet
dat ik ook trots op jou ben! Cindy, mijn schoonzus, lief en betrokken, dankjewel.
Lieve Alexander, jij hebt voor mij de prachtige tekening gemaakt voor de
omslag van dit boekje. Je hebt het “verbonden sterren” genoemd. Een titel recht
uit jouw hart van goud. Dankjewel lieve schat dat je zo lief bent, zo betrokken, en
zo enthousiast. Mama’s boekje is nu af. We hebben weer wat meer tijd om samen
te zijn.
Mijn liefste Alain, samen met Alexander ben jij de allerbelangrijkste in mijn
leven. Jij bent de laatste die dank krijgt. Voor de liefste zijn, voor er altijd zijn.
Ik hou van je.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
165
CURRICULUM VITAE
Curriculum Vitae
Fiona van Dijk was born in Hardenberg on December 2nd 1973. She graduated in
psychology in 1998 at the Catholic University Nijmegen. She specialized in Clinical
Psychology and finished her specialization in 2008 at the SPON in Nijmegen.
During the post initial educations she worked as a clinician at GGZ Nijmegen
(currently called Pro Persona, mental health care organization) and the Radboud
University Medical Center, department of Psychiatry, where she also started her
research for adults with ADHD and BPD. Between 2009 and 2016 she worked as
vice program director of the post-initial education for healthcare psychologists at
the SPON and as head of the Ambulatorium of the Radboud University in Nijmegen.
Recently she started a new assignment for GGNet (mental health care organization)
and the SKB (Regional hospital Koningin Beatrix) in Winterswijk where she
focusses on health innovation, clinical work, and research. She is shaping the
collaboration between GGNet and SKB; collaborates on a project to dramatically
reduce chronicity in the mental health care; and supervises young specialists.
Besides this she works in her private psychotherapy practice where she offers
supervision and learning-therapy for trainee psychiatrists, clinical psychologists,
and psychotherapists.

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk
167
DONDERS GRADUATE SCHOOL FOR COGNITIVE NEUROSCIENCE
Donders Graduate School for Cognitive Neuroscience
For a successful research Institute, it is vital to train the next generation of young
scientists. To achieve this goal, the Donders Institute for Brain, Cognition and
Behaviour established the Donders Graduate School for Cognitive Neuroscience
(DGCN), which was officially recognised as a national graduate school in 2009.
The Graduate School covers training at both Master’s and PhD level and provides
an excellent educational context fully aligned with the research programme of
the Donders Institute.
The school successfully attracts highly talented national and international students
in biology, physics, psycholinguistics, psychology, behavioral science, medicine
and related disciplines. Selective admission and assessment centers guarantee the
enrolment of the best and most motivated students.
The DGCN tracks the career of PhD graduates carefully. More than 50% of PhD
alumni show a continuation in academia with postdoc positions at top institutes
worldwide, e.g. Stanford University, University of Oxford, University of Cambridge,
UCL London, MPI Leipzig, Hanyang University in South Korea, NTNU Norway,
University of Illinois, North Western University, Northeastern University in Boston,
ETH Zürich, University of Vienna etc.. Positions outside academia spread among
the following sectors: specialists in a medical environment, mainly in genetics,
geriatrics, psychiatry and neurology. Specialists in a psychological environment,
e.g. as specialist in neuropsychology, psychological diagnostics or therapy. Positions
in higher education as coordinators or lecturers. A smaller percentage enters
business as research consultants, analysts or head of research and development.
Fewer graduates stay in a research environment as lab coordinators, technical
support or policy advisors. Upcoming possibilities are positions in the IT sector
and management position in pharmaceutical industry. In general, the PhDs
graduates almost invariably continue with high-quality positions that play an
important role in our knowledge economy.
For more information on the DGCN as well as past and upcoming defenses please
visit: http://www.ru.nl/donders/graduate-school/phd/

Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017Processed on: 11-1-2017
507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk507383-L-bw-van Dijk











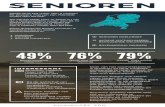






![グラウンド・コンディション² $ª& &t ± í ² 8Õ ]](https://static.fdocuments.nl/doc/165x107/61031521eabadb1bec0e2b0d/ffffffff-t-8-.jpg)
