Stella Mook T3-108
Transcript of Stella Mook T3-108

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 1/248
Prognostic factors in
breast cancer
One fits all?
Stella Mook

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 2/248
Prognostic Factors in Breast Cancer
One fits all?
Stella Mook

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 3/248
Cover: Jantien Mook – www.jantienmook.nl
Layout: Gildeprint Drukkerijen – www.gildeprint.nl
Printed by: Gildeprint Drukkerijen – www.gildeprint.nl
ISBN: 978-94-6108-151-3
Online: http:// dare.uva.nl/document
The work described in this thesis was performed at the Netherlands Cancer Institute-Antoni
van Leeuwenhoek Hospital, Amsterdam, the Netherlands.
Financial support provided by:
Netherlands Cancer Institute, Academic Medical Center, Agendia BV, AstraZeneca,
Boehringer Ingelheim, GlaxoSmithKline, Hoofdredactie OncoMotief.nl - EURIN BV, Novartis,
Roche, Sanofi-Aventis.
© 2011 Stella Mook, Amsterdam, the Netherlands

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 4/248
Prognostic Factors in Breast Cancer
One fits all?
ACADEMISCH PROEFSCHRIFT
ter verkrijging van de graad van doctor
aan de Universiteit van Amsterdam
op gezag van de Rector Magnificus
prof. dr. D.C. van den Boom
ten overstaan van een door het college voor promoties
ingestelde commissie,in het openbaar te verdedigen in de Agnietenkapel
op donderdag 21 april 2011, te 12:00 uur
door
Stella Mook
geboren te Hoorn

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 5/248
Promotiecommissie
Promotores: Prof. dr. E.J.Th. Rutgers
Prof. dr. L.J. Van ‘t Veer
Overige Leden: Prof. dr. R. Bernards
Prof. dr. J.W. Coeberg
Prof. dr. C.C.E. Koning
Prof. dr. J.W.R. Nortier
Prof. dr. S. Rodenhuis
Prof. dr. M.J. van de Vijver
Dr. J.H.G. Klinkenbijl
Faculteit der Geneeskunde

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 6/248
Voor Marcel & mijn ouders

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 7/248
Table of contents
Chapter 1 Introduction and outline 11
Chapter 2 Individualization of therapy using Mammaprint: 23
from development to the MINDACT Trial.
Cancer Genomics Proteomics2007; 4: 147-155.
Chapter 3 Daily clinical practice of fresh tumour tissue freezing and 41
gene expression profiling; logistics pilot study preceding
the MINDACT trial.
Eur J Cancer 2009; 45: 1201-1208.
Chapter 4 The 70-gene prognosis signature predicts early metastasis in 57
breast cancer patients between 55 and 70 years of age.
Ann Oncol 2010; 21: 717-722.
Chapter 5 The 70-gene prognosis-signature predicts disease outcome 73
in breast cancer patients with 1-3 positive lymph nodes in an
independent validation study.
Breast Cancer Res Treat 2009; 116: 295-302.
Chapter 6 Metastatic potential of T1 breast cancer can be predicted by 97
the 70-gene MammaPrint signature.
Ann Surg Oncol 2010; 17: 1406-1413.
Chapter 7 The predictive value of the 70-gene signature for adjuvant 117
chemotherapy in early breast cancer
Breast Cancer Res Treat 2010; 120: 655-661.
Chapter 8 Calibration and discriminatory accuracy of prognosis calculation 133
for breast cancer with the online Adjuvant! program:
a hospital-based retrospective cohort study
Lancet Oncol 2009; 10: 1070-1076.
Chapter 9 Independent prognostic value of screen detection in 157
invasive breast cancer
JNCI accepted for publication

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 8/248
Chapter 10 General discussion and future prospects 197
Chapter 11 Summary 215
Chapter 12 Nederlandse samenvatting 223
List of publications 233
Dankwoord 237
Curriculum vitae 245
Appendix Gene signature evaluation as a prognostic tool: 249
challenges in the design of the MINDACT trial.
Nat Clin Pract Oncol 2006; 3: 540-551.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 9/248
Chapter 1
Introduction and outline

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 10/248
Chapter 1
12

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 11/248
Introduction and outline
13
1Introduction
Breast cancer
Breast cancer is the most frequently diagnosed malignancy in women worldwide. In the
Netherlands in 2008, 13,005 women were diagnosed with invasive breast cancer and 3,327
patients died of the disease.1 Although there is an increase in breast cancer incidence,
breast cancer mortality is decreasing in the last decennia. 2-4 This decrease in mortality is
mainly caused by both the introduction of breast cancer screening and the improvement
and more extensive use of adjuvant systemic therapy.2,3,5-9 Currently, approximately 2/3
of the patients who are diagnosed with breast cancer do not have nodal involvement at
diagnosis and about 2/3 of the patients are 55 years of age or older at diagnosis.10
Treatment of breast cancer
The treatment of early stage breast cancer consists of two aspects. The first is loco-regional
control, which is primarily achieved by surgery with or without radiotherapy. The second part
of breast cancer treatment focuses on preventing the development of distant metastases.
Distant metastases account for the majority of breast cancer deaths and are thought to
develop from undetectable micrometastases or circulating tumor cells that are already
present at time of diagnosis. Adjuvant systemic therapy (i.e. chemotherapy, hormonal
therapy and/or targeted therapy) can help eradicate micrometastases and circulatingtumor cells, thereby preventing distant metastases to occur and thus improving survival.
The incurable nature of metastatic breast cancer emphasizes the importance of selecting
patients for adjuvant systemic therapy who are at risk of developing distant metastases. In
patients with lymph node-negative disease, adjuvant chemotherapy improves survival on
average by 25%.11 On the other hand, especially chemotherapy can cause a wide range of
acute and long-term side effects.12
Adjuvant systemic therapy
Since the introduction in the early 1980s, there is a steady increase in the use of adjuvant
systemic therapy (AST) in the Netherlands.9 This increase is supported by data from the
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) overviews showing a significant
benefit of adjuvant systemic therapy for disease-free and overall survival. 11,13-15 In the
1990s, adjuvant systemic therapy was recommended mainly for patients with lymph
node-positive breast cancer. In 2000, the National Breast Cancer Consultation Netherlands
(NABON) developed the first national guideline for adjuvant systemic therapy.16 Tamoxifen
was recommended for lymph node-positive, estrogen receptor (ER)-positive tumors
in postmenopausal patients. For lymph node-positive premenopausal patients and

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 12/248
Chapter 1
14
for lymph node-positive postmenopausal patients with an estrogen receptor negative
tumor chemotherapy was recommended. In addition, it was recommended to consider
adjuvant systemic therapy for a subgroup of patients with lymph node-negative tumors
depending on tumor size and tumor grade. The use of AST for Dutch patients with early
stage breast cancer increased significantly over time, from 37% in the period 1990–1997, to
53% in 2002–2006.17,18 Currently, Dutch breast cancer patients are treated according to the
NABON and Dutch Institute for Healthcare Improvement (CBO) guidelines and adjuvant
systemic therapy is recommended for > 80% of all patients.19 As in the Netherlands, the
administration of AST increased substantially in the US, were the use of chemotherapy or
hormonal therapy tripled from 1987 to 2000 in women with node-negative disease.20 Only
1 in 5 women with node negative disease did not receive any form of adjuvant systemic
therapy in the US in the year 2000.20
Who to treat; prognostic factors
Patients who are at high risk of developing distant metastases are candidates for AST.
Prognostic factors help identify patients who are at high risk of distant metastases in
the absence of AST.21 An ideal prognostic factor tells us exactly ‘who to treat’, by reliably
distinguishing patients who are at high risk of developing distant metastases from those
who are at low risk. Nowadays, the selection of patients who are at high risk of recurrence
is based on clinical and pathological prognostic factors, such as age, menopausal status,
co-morbidity, tumor size, tumor grade, lymph node status and hormonal receptor status.22 These clinicopathological criteria are often combined into guidelines or models such as the
St. Gallen recommendations, the Nottingham Prognostic Index, the Dutch CBO guideline or
the Adjuvant! tool.19,23-25 However, tumors with the same clinicopathological characteristics
can have strikingly different outcomes. Consequently, AST recommendation according
to these guidelines is far from accurate. Although 60-70% of patients with lymph node-
negative breast cancer are likely to be cured by surgery and radiotherapy alone, the majority
of patients is currently treated with chemotherapy, hormonal therapy and/or targeted
therapy (Figure 1).11 As a result, a substantial proportion of patients will unnecessarily receive
AST and will be needlessly exposed to its toxicity. This overtreatment is due to the lack ofaccurate identification of patients with a low risk of developing distant metastases, who are
unlikely to benefit from adjuvant systemic therapy. Apparently, better prognostic factors
are urgently needed. Although, a number of single parameter prognostic biomarkers have
been studied, few have achieved the level of supporting evidence required for routine
clinical use.26 One of the more recently developed techniques that provides us with
promising new prognostic tools is the microarray gene expression technique.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 13/248
Introduction and outline
15
1
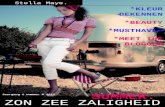
Figure 1. Survival of early stage breast cancer patients after loco-regional treatment.
Gene expression profiling
The introduction of the new high-throughput microarray technology at the beginning of
this century, has introduced a new era of multi-parameter prognostic tests and causeda revolution in medicine, particularly in the oncology field. 27 In contrast to the single-
parameter biomarker, microarray analyses can measure the expression of thousands of
genes in the tumor simultaneously.28-30 The expression level of all genes together gives
insight in tumor biology and in this way provides the possibility to subdivide breast cancer
based on its biology. Since tumor behavior and clinical outcome depend largely on tumor
biology, gene expression profiles are anticipated to refine the prognostication of breast
cancer.
The first published molecular classification of breast cancer using microarray technology
displayed the molecular heterogeneity of the disease. Unsupervised analyses of microarraygene expression data of breast cancer patients have resulted in the identification of 4
molecular subtypes, according to gene expression profile: Luminal A, Luminal B, Basal-like
and ERBB2 breast cancers.31 Those gene expression profiles reflect biological diversity and
were shown to be associated with disease outcome as well.31,32 Many subsequent studies
have discovered several other prognostic gene expression profiles.31,33-40 Remarkably,
although the prognostic performance of these signatures in terms of individual patient
classification was similar, overlap in terms of gene identity was limited.41 However, it was
shown that these signatures reflect overlapping common biological processes and cellular
phenotypes that drive breast cancer prognosis.42,43
~30% die of breast canceradjuvant therapy can be beneficial
~70% survive breast canceradjuvant therapy is not beneficial

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 14/248
Chapter 1
16
In addition to unsupervised analyses, supervised analyses can be used to develop a
gene expression signature that can predict clinical outcome. In contrast to unsupervised
analyses that classify tumors based on the similarity of gene expression, supervised
analyses compares gene-expression data from patients with known clinical outcomes
(e.g. absence or presence of distant metastases) to identify genes that are associated
with prognosis. Such classification method was used to identify the 70-gene prognosis
signature (MammaPrint™).38 The 70-gene signature has been identified using frozen tumor
samples from 78 patients who were diagnosed at the Netherlands Cancer Institute-Antoni
van Leeuwenhoek hospital (NKI-AVL) with lymph node-negative breast cancer and who
were up to 55 years of age at diagnosis. Among these 78 patients, 44 remained free of
distant metastases for at least 5 years (defined as the good prognosis group), whereas 34
patients developed distant metastases within 5 years of diagnosis (poor prognosis group).
The signature consists of the top 70 genes that were differentially expressed between
the two prognosis groups and most accurately classified tumors in the good- or poor
prognosis group. The signature was validated in a consecutive second patient series from
the NKI-AVL, consisting of 151 lymph node-negative and 144 lymph node-positive patients
up to 53 years at diagnosis, and in a third independent patient series of 302 lymph node-
negative breast cancer patients from 5 European hospitals, who were up to 60 years of
age at diagnosis.44,45 Subsequently, the prognostic value of 70-gene signature has been
confirmed by others.46-48
In 2004, another prognostic test has been developed. The OncotypeDX™ is a RT-PCR based
assay performed on paraffin-embedded tumor samples that classifies tumors based on theexpression of 16 genes into a low Recurrence Score (RS), an intermediate RS or a high RS.36
A community-based validation study demonstrated that the RS could be used to predict
the outcome of node-negative patients receiving tamoxifen alone.49 Retrospective analysis
of the node-negative NSABP B20 and node-positive SWOG 8814 trial showed similar
prognostic value for the RS in patients treated with the combination of tamoxifen and
chemotherapy.50,51
Validation studies to assess the reliability and reproducibility are of utmost importance to
determine a signature’s clinical utility. Furthermore, practical issues of the implementation
of gene expression microarrays need to be addressed and quality of performance andstandardized procedures for a diagnostic test should be monitored by International
Organization for Standardization (ISO) or Clinical Laboratory Improvement Amendments
(CLIA) certification and should preferably fall under the regulatory oversight such as the
US Food and Drug Administration (FDA).52 Successful implementation of a gene expression
profile requires, in addition to thorough validation studies, the collection of good quality,
fresh frozen tumor tissue and close collaboration between different departments in the
hospital.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 15/248
Introduction and outline
17
1Rationale and outline of this thesis
The overall aim of this thesis is to evaluate the accuracy and clinical utility of a relatively new
prognostic microarray test, the 70-gene signature, in several breast cancer subpopulations.
In addition, we evaluated the accuracy of the extensively used prognostic tool Adjuvant!,
which is based on clinicopathological characteristics. Finally, we evaluated whether the
method of detection of a tumor (i.e. screen-detected or symptomatic) affect prognosis and
should be taken into account to improve patient selection for AST.
The first part of this thesis focuses on the applicability of the 70-gene signature
(MammaPrint™) and the potential improvement of patient selection for adjuvant systemic
therapy by using this microarray test.
In chapter 2 the development of the 70-gene signature, its initial retrospective validation
studies and logistical feasibility studies are described. In addition, the currently conducted
prospective randomized clinical trial, the so-called MINDACT study (Microarray In Node-
negative and 1-3 positive lymph node disease may Avoid ChemoTherapy) which will
compare the prognostic value of the 70-gene signature with that of currently available
prognostic clinicopathological variables, is discussed. More detailed information about the
design of the MINDACT trial is provided in Appendix 1.
Chapter 3 presents the results of a European pilot study preceding the MINDACT trial to
test the feasibility and to optimize the logistics for the collection of good-quality fresh
frozen tumor tissue in order to perform the 70-gene signature. The 70-gene signature has been developed and so far mostly validated in premenopausal
patients with lymph node-negative breast cancer. However, the majority of breast
carcinomas is diagnosed in postmenopausal women. Therefore, we evaluated the accuracy
of the 70-gene signature in postmenopausal patients, which is described in chapter
4. Although lymph node metastases are a strong indicator of a poor prognosis, still
approximately 30-40% of patients with 1-3 positive lymph nodes at diagnosis will remain
free of distant metastases without adjuvant systemic therapy. Currently, there are no
biomarkers available to select these low risk lymph node-positive patients. In chapter 5 we
evaluated the ability of the 70-gene signature to identify patients with 1-3 positive lymphnodes who are at low risk of recurrence in an independent, retrospective validation study.
In addition to lymph node status, tumor size is known to be a powerful prognostic factor,
with small tumor size being thought to indicate a low risk of recurrence. Nevertheless, small
tumors still can metastasize, which leaves us with the question of the necessity of adjuvant
systemic therapy in patients with pT1 (≤20mm) tumors. In Chapter 6 the prognostic value
and clinical utility of the 70-gene signature in a pooled retrospective series of patients with
pT1 (≤20mm) breast carcinomas are discussed. Adjuvant treatment allocation based on
the 70-gene signature seems to be justified when the low risk of recurrence in the good
prognosis group is sufficiently low to withhold chemotherapy and the expected benefit

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 16/248
Chapter 1
18
from adjuvant chemotherapy is limited. In addition, administration of chemotherapy in
patients classified as high risk is legitimate when the benefit of treatment in these patients
is substantial. In chapter 7 we assessed this predictive value of the 70-gene signature in a
pooled analysis.
The 70-gene signature is currently studied in the prospective MINDACT (Microarray In Node-
negative and 1-3 positive lymph node disease may Avoid ChemoTherapy) trial, which will
evaluate whether patients who are considered high risk according to the currently available
prognostic tool Adjuvant! but classified as low risk by the 70-gene signature can be safely
spared chemotherapy. Adjuvant! combines clinicopathological characteristics, such as
patient age, co-morbidity, tumor size, lymph node involvement, histological grade and
estrogen receptor status, to forecast the overall and breast cancer-specific mortality and to
predict the benefit of additional chemotherapy and/or endocrine therapy. The Adjuvant!
model is based on information from breast cancer patients in the United States who were
diagnosed between 1988 and 1992 and recorded in the Surveillance, Epidemiology and
End Results (SEER) registry.24 In 2005, the model was retrospectively validated in breast
cancer patients from British Columbia.53 Since the European breast cancer populations
may differ from those in the US and Canada, the question remains whether outcome
predictions of the Adjuvant! model are applicable to the European population. Therefore,
we conducted a retrospective validation study to test the accuracy of Adjuvant! in a Dutch
breast cancer cohort of 5,830 patients, which is described in chapter 8. The aim of this
study was to assess both the ability of Adjuvant! to predict outcomes in (sub)groups ofDutch breast cancer patients (calibration) and its ability to distinguish individuals who will
experience different outcomes (discriminatory accuracy).
Awaiting the incorporation of gene expression profiles in prognostic tools, models such as
Adjuvant! are still suboptimal. Incorporation of other prognostic markers may also improve
these tools. It has been shown that mammographic screening detects breast cancer at an
earlier stage.54-56 Therefore, we investigated whether method of detection has additional
prognostic value that could improve the estimation of disease outcome, assuming that
screen-detected carcinomas are of a different tumor biology. This question is addressed inchapter 9, where we studied the accuracy of Adjuvant! in patients with a screen-detected
carcinoma as well as assessed the independent prognostic value of screen-detection in a
retrospective patient cohort.
This thesis ends with concluding remarks and future prospects in chapter 10 and a
summary of the results presented in chapter 11.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 17/248
Introduction and outline
19
1Reference List
1. http://www.ikcnet.nl. Last accessed January 12, 2011.
2. Jatoi I and Miller AB. Why is breast-cancer mortality declining? Lancet Oncol 2003; 4: 251-254.
3. Smigal C, Jemal A, Ward E, et al. Trends in breast cancer by race and ethnicity: update 2006. CA Cancer J Clin
2006; 56: 168-183.
4. http://www.cancer.org. Cancer Facts & Figures 2010. Last accessed January 15, 2011.
5. Berry DA and Ravdin PM. Breast cancer trends: a marriage between clinical trial evidence and
epidemiology. J Natl Cancer Inst 2007; 99: 1139-1141.
6. Chu KC, Tarone RE, Kessler LG, et al. Recent trends in U.S. breast cancer incidence, survival, and mortality
rates. J Natl Cancer Inst 1996; 88: 1571-1579.
7. Garne JP, Aspegren K, Balldin G, Ranstam J. Increasing incidence of and declining mortality from breast
carcinoma. Trends in Malmo, Sweden, 1961-1992. Cancer 1997; 79: 69-74.
8. Otten JD, Broeders MJ, Fracheboud J, et al . Impressive time-related influence of the Dutch screening
programme on breast cancer incidence and mortality, 1975-2006. Int J Cancer 2008; 123: 1929-1934.
9. Vervoort MM, Draisma G, Fracheboud J, van de Poll-Franse LV, de Koning HJ. Trends in the usage of
adjuvant systemic therapy for breast cancer in the Netherlands and its effect on mortality. Br J Cancer
2004; 91: 242-247.
10. Ries LAG, Melbert D, Krapcho M et al. SEER Cancer Statistics Review, 1975-2005. Bethesda, MD: National
Cancer Institute 2008; http://seer.cancer.gov/csr/1975_2005/, based on November 2007 SEER data
submission, posted to the SEER web site. Last accessed 28 November, 2008.
11. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for
early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet
2005; 365: 1687-1717.
12. Eifel P, Axelson JA, Costa J, et al . National Institutes of Health consensus development conference
statement: Adjuvant therapy for breast cancer, November 1-3, 2000. J Natl Cancer Inst 2001; 93: 979-989.
13. Clarke M, Coates AS, Darby SC, et al . Adjuvant chemotherapy in oestrogen-receptor-poor breast cancer:
patient-level meta-analysis of randomised trials. Lancet 2008; 371: 29-40.
14. Early Breast Cancer Trialists’ Collaborative Group. Tamoxifen for early breast cancer: an overview of the
randomised trials. Lancet 1998; 351: 1451-1467.
15. Early Breast Cancer Trialists’ Collaborative Group. Polychemotherapy for early breast cancer: anoverview of the randomised trials. Lancet 1998; 352: 930-942.
16. Bontenbal M, Nortier JW, Beex LV, et al . [Adjuvant systemic therapy for patients with resectable breast
cancer: guideline from the Dutch National Breast Cancer Platform and the Dutch Society for Medical
Oncology]. Ned Tijdschr Geneeskd 2000; 144: 984-989.
17. Van Steenbergen LN, Van de Poll-Franse LV, Wouters MW, et al . Variation in management of early breast
cancer in the Netherlands, 2003-2006. Eur J Surg Oncol 2010; 36 Suppl 1: S36-S43.
18. Sukel MP, Van de Poll-Franse LV, Nieuwenhuijzen GA, et al . Substantial increase in the use of adjuvant
systemic treatment for early stage breast cancer reflects changes in guidelines in the period 1990-2006
in the southeastern Netherlands. Eur J Cancer 2008; 44: 1846-1854.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 18/248
Chapter 1
20
19. CBO Richtlijn Mammacarcinoom 2008. http://www.cbo.nl/product/richtlijnen/folder20021023121843/rl_mamma_08.pdf
20. Harlan LC, Clegg LX, Abrams J, Stevens JL, Ballard-Barbash R. Community-based use of chemotherapy
and hormonal therapy for early-stage breast cancer: 1987-2000. J Clin Oncol 2006; 24: 872-877.
21. Weigelt B, Peterse JL, van ‘t Veer LJ. Breast cancer metastasis: markers and models. Nat Rev Cancer 2005; 5:
591-602.
22. Harris JR. Staging of Breast Cancer. 2009; Fourth edition: 489-500.
23. Goldhirsch A, Ingle JN, Gelber RD, et al . Thresholds for therapies: highlights of the St. Gallen International
Expert Consensus on the primary therapy of early breast cancer 2009. Ann Oncol 2009; 20: 1319–1329.
24. Ravdin PM, Siminoff LA, Davis GJ, et al. Computer program to assist in making decisions about adjuvant
therapy for women with early breast cancer. J Clin Oncol 2001; 19: 980-991.
25. Todd JH, Dowle C, Williams MR, et al. Confirmation of a prognostic index in primary breast cancer. Br J
Cancer 1987; 56: 489-492.
26. Harris L, Fritsche H, Mennel R, et al. American Society of Clinical Oncology 2007 update of
recommendations for the use of tumor markers in breast cancer. J Clin Oncol 2007; 25: 5287-5312.
27. Schena M. Microarray Analysis. New York, Wiley-Liss. First edition 2002.
28. Brown PO and Botstein D. Exploring the new world of the genome with DNA microarrays. Nat Genet 1999;
21: 33-37.
29. DeRisi J, Penland L, Brown PO, et al. Use of a cDNA microarray to analyse gene expression patterns in
human cancer. Nat Genet 1996; 14: 457-460.
30. Schena M, Shalon D, Davis RW, Brown PO. Quantitative monitoring of gene expression patterns with a
complementary DNA microarray. Science 1995; 270: 467-470.
31. Perou CM, Sorlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature 2000; 406: 747-
752.
32. Sorlie T, Perou CM, Tibshirani R, et al . Gene expression patterns of breast carcinomas distinguish tumor
subclasses with clinical implications. Proc Natl Acad Sci USA 2001; 98: 10869-10874.
33. Chang HY, Nuyten DSA, Sneddon JB, et al . Robustness, scalability, and integration of a wound-response
gene expression signature in predicting breast cancer survival. Proc Natl Acad Sci USA 2005; 102: 3738-3743.
34. Huang E, Cheng SH, Dressman H, et al . Gene expression predictors of breast cancer outcomes. Lancet
2003; 361: 1590-1596..
35. Ma XJ, Hilsenbeck SG, Wang W, et al. The HOXB13:IL17BR expression index is a prognostic factor in early-
stage breast cancer. J Clin Oncol 2006; 24: 4611-4619.36. Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative
breast cancer. N Engl J Med 2004; 351: 2817-2826.
37. Sotiriou C, Neo SY, McShane LM, et al . Breast cancer classification and prognosis based on gene
expression profiles from a population-based study. Proc Natl Acad Sci USA 2003; 100: 10393-10398.
38. Van ‘t Veer LJ, Dai H, Van de Vijver MJ, et al . Gene expression profiling predicts clinical outcome of breast
cancer. Nature 2002; 415: 530-536.
39. Wang Y, Klijn JG, Zhang Y, et al. Gene-expression profiles to predict distant metastasis of lymph-node-
negative primary breast cancer. Lancet 2005; 365: 671-679.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 19/248
Introduction and outline
21
140. West M, Blanchette C, Dressman H, et al . Predicting the clinical status of human breast cancer by using
gene expression profiles. Proc Natl Acad Sci USA 2001; 98: 11462-11467.
41. Fan C, Oh DS, Wessels L, et al. Concordance among gene-expression-based predictors for breast cancer.
N Engl J Med 2006; 355: 560-569.
42. Loi S, Haibe-Kains B, Desmedt C, et al. Definition of clinically distinct molecular subtypes in estrogen
receptor-positive breast carcinomas through genomic grade. J Clin Oncol 2007; 25: 1239-1246.
43. Yu JX, Sieuwerts AM, Zhang Y, et al. Pathway analysis of gene signatures predicting metastasis of node-
negative primary breast cancer. BMC Cancer 2007; 7: 182.
44. Buyse M, Loi S, Van ‘t Veer L, et al . Validation and clinical utility of a 70-gene prognostic signature for
women with node-negative breast cancer. J Natl Cancer Inst 2006; 98: 1183-1192.
45. Van de Vijver MJ, He YD, Van ‘t Veer LJ, et al . A gene-expression signature as a predictor of survival in
breast cancer. N Engl J Med 2002; 347: 1999-2009.
46. Bueno de Mesquita JM, Linn SC, Keijzer R et al. Validation of 70-gene prognosis signature in node-
negative breast cancer. Breast Cancer Res Treat 2009; 117: 483–495.
47. Ishitobi M, Goranova TE, Komoike Y, et al. Clinical utility of the 70-gene MammaPrint profile in a Japanese
population. Jpn J Clin Oncol 2010; 40: 508-512.
48. Wittner BS, Sgroi DC, Ryan PD, et al. Analysis of the MammaPrint breast cancer assay in a predominantly
postmenopausal cohort. Clin Cancer Res 2008; 14: 2988-2993.
49. Habel LA, Shak S, Jacobs MK, et al. A population-based study of tumor gene expression and risk of breast
cancer death among lymph node-negative patients. Breast Cancer Res 2006; 8: R25.
50. Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-
negative, estrogen receptor-positive breast cancer. J Clin Oncol 2006; 24: 3726-3734.
51. Albain KS, Barlow WE, Shak S, et al. Prognostic and predictive value of the 21-gene recurrence score
assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on
chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol 2010; 11: 55-65.
52. Couzin J. Diagnostics: Amid debate, gene-based cancer test approved. Science 2007; 315: 924.
53. Olivotto IA, Bajdik CD, Ravdin PM, et al. Population-based validation of the prognostic model ADJUVANT!
for early breast cancer. J Clin Oncol 2005; 23: 2716-2725.
54. Chu KC, Smart CR, Tarone RE. Analysis of breast cancer mortality and stage distribution by age for the
Health Insurance Plan clinical trial. J Natl Cancer Inst 1988; 80: 1125-1132.
55. Connor RJ, Chu KC, Smart CR. Stage-shift cancer screening model. J Clin Epidemiol 1989; 42: 1083-1095.56. Fracheboud J, Otto SJ, van Dijck JA, et al . Decreased rates of advanced breast cancer due to
mammography screening in The Netherlands. Br J Cancer 2004; 91: 861-867.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 20/248
Chapter 2
Individualization of therapy using
Mammaprint: from development to the
MINDACT Trial
Stella Mook
Laura J. Van ‘t Veer
Emiel J. Th. Rutgers
Martine J. Piccart-Gebhart
Fatima Cardoso
Cancer Genomics Proteomics 2007; 4: 147-155.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 21/248
Chapter 2
24
Abstract
To date, most treatment decisions for adjuvant chemotherapy in breast cancer are based
on conventional clinicopathological criteria. Since breast cancer tumors with similar
clinicopathological characteristics can have strikingly different outcomes, the current
selection for adjuvant chemotherapy is far from accurate. Using high-throughput microarray
analysis, a 70-gene signature was identified which can accurately select early stage breast
cancer patients who are highly likely to develop distant metastases, and therefore, may
benefit the most from adjuvant chemotherapy. This review describes the development of
the 70-gene profile (MammaPrint™), its retrospective validation and feasibility studies, and
its prospective validation in the large adjuvant MINDACT (Microarray In Node-negative
Disease may Avoid ChemoTherapy) clinical trial.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 22/248
Development of the MammaPrint
25
2
Introduction
The outcome of patients with breast cancer has improved in the last 20 years, due to
both early detection and the amelioration of adjuvant systemic treatment. The majority
of early stage breast cancer patients receive adjuvant systemic treatment, which may
include chemotherapy, hormonal therapy, immunotherapy or a combination. Nowadays,
patients who should receive chemotherapy are selected by using consensus guidelines like
the St. Gallen, or the National Comprehensive Cancer Network (NCCN) guidelines which
are based on the assessment of clinicopathological criteria such as age, tumor size and
grade, hormonal receptor status and axillary lymph node involvement.1-3 However, breast
cancer tumors with similar clinicopathological characteristics can have strikingly different
outcomes, reflecting the heterogeneity of the disease. Consequently, the current adjuvant
treatment decision-making process for breast cancer patients is far from accurate. The
majority of early stage breast cancer patients, particularly those with lymph node-negative
disease (60-70%), has a fairly good 10-year overall survival with locoregional treatment
alone, with only 30-40% developing distant metastases.4 Notwithstanding these facts,
most lymph node-negative breast cancer patients are offered chemotherapy, according to
the currently used guidelines, causing an important proportion of overtreatment.1-3 This is
justified largely by our inability to clearly identify those patients who will not relapse and
hence do not need adjuvant chemotherapy. Since metastatic breast cancer is an incurable
disease, the only chance for cure is in the adjuvant setting. However, overtreatment not
only unnecessarily exposes women to potential toxicity and side-effects of this treatment,but also increases the economic burden of breast cancer on society. It is thus quite clear
that robust and reliable prognostic markers to accurately select patients not requiring
aggressive adjuvant therapy are urgently needed.
With the introduction of new high-throughput methods, such as gene expression
microarray technologies, the expression level of tens of thousands of genes can be measured
simultaneously. Using microarray techniques, several studies have recently classified
breast tumors according to their gene expression profile and identified prognostic and
predictive classifiers.5-14 Although these studies appear to be very promising, microarray
analysis has some potential pitfalls. For example, the analysis of the large amount of dataobtained through this technology can cause process errors and overfitting. Furthermore,
retrospective studies using frozen tissue processed and stored many years ago could result
in different levels of gene expression due to differences in tissue handling and pertain to
patient populations which may be different from those diagnosed today. Taking all this into
account, validation studies, particularly prospective ones, are indispensable in assessing
the reliability and reproducibility of the results and in identifying the true benefit of a
classifier for clinical practice.
Here we provide an overview of the development of the 70-gene profile (MammaPrint™)
from discovery to application in clinical trials, including retrospective validation and

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 23/248
Chapter 2
26
feasibility studies, and its prospective validation in the large MINDACT (Microarray In Node-
negative Disease may Avoid ChemoTherapy) clinical trial.
The Development of the 70-gene Signature
By using gene expression profiling, Van ’t Veer and colleagues developed a 70-gene
classifier that accurately distinguished breast cancer patients who were likely to remain free
of distant metastases (good profile) from breast cancer patients at high risk of developing
distant metastases (poor profile).8 To develop this 70-gene profile, 78 tumors from women
with lymph node-negative breast cancer were studied. Patients were under 55 years of
age at diagnosis, had a primary invasive breast carcinoma less than 5 cm in diameter,
no previous malignancies and were treated at The Netherlands Cancer Institute (NKI).
All patients were treated by modified radical mastectomy or breast conserving therapy.
Five out of 78 patients received adjuvant systemic treatment, consisting of chemotherapy
(n = 3) or hormonal therapy (n = 2); all 5 patients developed distant metastases within
5 years of diagnosis. Forty-four patients remained free of distant metastases for at least
5 years (good-prognosis group), whereas the remaining 34 patients did develop distant
metastases within 5 years of diagnosis (poor-prognosis group). The mean follow-up of the
good prognosis group was 8.7 years, the mean time to distant metastases was 2.5 years.
From all 78 frozen tumor samples, the percentage of tumor cells was determined in a
hematoxylin and eosin stained section, before and after cutting sections for RNA isolation.
Only tumor samples with at least 50% tumor cells were eligible. RNA was isolated andlabeled with a fluorescent dye. An equal amount of RNA from all tumors was pooled
and provided reference RNA. Both tumor RNA and reference RNA were hybridized on an
oligonucleotide microarray platform containing approximately 25,000 genes, synthesized
by inkjet technology (produced by Agilent).15
In a first step, using a statistical analysis method called ‘supervised classification’, the
expression of 231 genes appeared to be significantly correlated with disease outcome
(distant metastases within 5 years). These 231 genes were ranked, based on their correlation
coefficient with disease outcome; the top 70 of these were shown to most accurately
classify tumors in either the good- or the poor-prognosis category.All 78 tumors were ranked according to their correlation with the average expression of the
70 genes of the patients who did not develop a distant metastasis (good-outcome patients).
Where the sensitivity was optimized by setting a threshold resulting in a misclassification
of less than 10% of patients with a poor disease outcome. Consequently, 3 out of the 34
patients with a poor disease outcome would erroneously be withheld chemotherapy
based on this new tool (9% misclassification).
This supervised classification strategy resulted in the 70-gene dichotomous risk classifier,
using the 78 tumors as a training set. To initially validate the 70-gene profile, an additional
set of 7 tumors from patients with a good clinical outcome (free from distant metastases for

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 24/248
Development of the MammaPrint
27
2
at least 5 years after diagnosis) and 12 tumors from patients with a poor clinical outcome
(distant metastases within 5 years of diagnosis) were analyzed. The 70-gene profile
accurately predicted disease outcome in 17 out of the 19 patients, thereby confirming the
initial performance of the prognostic classifier.
Although the first results were very promising, one major comment on the development
of the 70-gene profile was the small sample size of both the training and the test sets.
Supervised analysis of a relatively small sample size, in combination with the enormous
number of parameters (genes) can result in what is called ‘overfitting’.16 Since the classifier
is developed and optimized to classify the tumors in the training set accurately, the model
will fit this training set but could predict disease outcome imprecisely in an independent
sample set. Therefore, well-designed validation studies were necessary to confirm these
earlier findings.
First Retrospective Validation Series Confirms the Prognostic Value of the 70-gene
Signature
The first validation of the 70-gene profile was performed by Van de Vijver and colleagues,
on a consecutive series of 295 breast cancer tumors; 144 tumors from lymph node-positive
and 151 tumors from lymph node-negative breast cancer patients.7 Sixty-one lymph node-
negative patients were also part of the previous series used to develop the prognostic
profile. All patients were diagnosed between 1984 and 1995 at the NKI and under the
age of 53 at diagnosis. Tumors were primary invasive breast carcinomas less than 5 cm,treated with locoregional therapy alone (56%), or in combination with adjuvant systemic
treatment (44%) consisting of chemotherapy alone (31%), hormonal therapy alone (7%),
or a combination (7%). The median follow-up was 7.8 years for the 207 patients without
metastasis as first event and the median time to distant metastases was 2.7 years. The
median follow-up among all 295 patients was 6.7 years.
For all 234 samples that were not part of the previous study, the correlation coefficient of
the average level of expression of the 70 genes with the previously established good profile
was calculated. Tumors with a correlation coefficient above the previously determined
threshold (above 0.4) were assigned to the good-profile group. For the 61 patients whowere included in the previous study, a threshold of 0.55 was used to correct for overfitting.
The profile accurately distinguished a good-prognosis group (of 115 tumors) with a 10-year
overall survival of 95% (±2.6%) from a poor-prognosis group (of 180 tumors) with a 10-
year overall survival of 55% (±4.4%). The 70-gene profile was associated with established
prognostic factors such as age, tumor grade and estrogen receptor (ER) status. Remarkably,
the 70-gene profile did not seem to depend on the lymph node status, since the 144
tumors from lymph node-positive patients were equally distributed over the poor- and
good-prognosis groups. In the multivariate analysis of the risk of distant metastases as first
event, the poor-prognosis signature, large tumor size, presence of vascular invasion and no

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 25/248
Chapter 2
28
chemotherapy treatment were the only significant independent factors for the prediction
of the likelihood of developing distant metastases. With an overall hazard ratio of 4.6, the
70-gene profile was by far the most powerful predictor of distant metastases (95% CI 2.3-
9.2; p < 0.001).
To assess the value of this new prognosticator in a clinical context, the 70-gene profile
was compared to the St. Gallen and NIH criteria used at that time. 17,18 The 70-gene profile
assigned 40% of the patients in the good-prognosis or low-risk group, compared with only
15% according to the St. Gallen consensus guidelines and 7% according to the NIH criteria.
Furthermore, patients identified as being at low risk (good prognosis) by the 70-gene profile
were more likely to remain free of distant metastases, compared with patients classified as
being at low risk according to the St. Gallen or the NIH criteria. On the other hand, patients
identified as being at high risk (poor prognosis) by the 70-gene profile had a higher risk of
developing distant metastases than the high-risk patients classified by the St. Gallen or NIH
criteria. The misclassification of patients using the clinicopathological criteria is even more
clearly perceptible when the high-risk group, according to the NIH (140 out of 151 lymph
node-negative breast cancer patients), is subdivided using the 70-gene classifier. This NIH
high-risk group includes 53 out of 140 patients with a good 70-gene prognosis and indeed
a good clinical outcome, indicating a better prediction of disease outcome when using the
70-gene profile.
In this validation series, the 70-gene profile had a high negative predictive value in all
subgroups; 97% for the new lymph node-negative patients; 96% for the lymph node-
positive patients; and 96% for all new patients, respectively. Due to the setting of thethreshold in the previous study, the profile was built to have a minimum of misclassified
patients with a poor disease outcome. Consequently, the positive predictive value was
only 38% for all new patients. Although this would still lead to overtreatment, the absolute
number of patients unnecessarily exposed to chemotherapy would still be reduced by
25-30%, compared to treatment selection based on the clinicopathological criteria, since
the total proportion of poor-prognosis patients identified by the 70-gene profile is much
smaller than the proportion of high-risk patients according to the St. Gallen or NIH criteria.
Moreover, the overall selection of patients who should receive chemotherapy and patients
who can safely be spared this treatment seems to be far more accurate.An important criticism of this first validation was that the series included 61 patients from
the study on which the classifier was established. Although this validation already showed
a significant prognostic value in patients that were not included in the previous study when
analyzed separately (OR 15.3; 95% CI 1.8-127; p = 0.003), this was further substantiated in
a recently published independent validation study performed by the TRANSBIG research
consortium.19 This independent validation also addressed the question whether the 70-
gene profile, which was developed and so far validated on a selected group of patients
(young patients with stage I or II tumors, from a single institution), could be applied to a
larger proportion of breast cancer patients.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 26/248
Development of the MammaPrint
29
2
Independent Multi-center Validation Established the Prognostic Value of the 70-gene
Profile
In the study from the TRANSBIG consortium, recently published in the JNCI, the 70-gene
profile was independently validated in 302 patients from 5 different European hospitals.19
Patients were up to 61 years at diagnosis, diagnosed before 1999, with a lymph node-
negative T1 or T2 breast carcinoma and had not received any adjuvant systemic therapy.
The median follow-up was 13.6 years.
The frozen tumor samples were sent to Agendia, a spin-off company of the NKI in
Amsterdam, where RNA was isolated and the microarray analysis was performed. The
samples were hybridized on the MammaPrint™, which is a custom-made microarray slide,
assessing the mRNA expression of the previously identified 70 genes in triplicate. A tumor
was classified as high risk if the correlation coefficient for the average expression of the
70-gene profile was under 0.4. Importantly, researchers at Agendia were blinded to the
clinical data while performing the genomic test. Clinical data from these patients were
collected, audited by two independent auditors and sent to an independent statistical
partner in Brussels. The researchers collecting the clinical data were blinded for the
genomic test results. Furthermore, a central pathology review was performed in Milan to
decrease the potential heterogeneity of results from different laboratories (ER status and
grade were centrally assessed in 80% of samples). Only the independent statistical office
had simultaneous access to both clinical and genomic data and performed the correlation
analysis. This independent validation confirmed that the 70-gene profile is a strong prognostic
factor for overall survival and time to distant metastases, with hazard ratios of 2.79 (95%
CI 1.60-4.87) and 2.32 (95% CI 1.35-4.0), respectively. The prognostic value of the 70-gene
profile remained statistically significant after adjustment for other risk classifications, using
clinicopathological criteria with known prognostic value, such as the St. Gallen consensus
guidelines, the Nottingham Prognostic Index and the prognostic evaluation tool Adjuvant!
Online. This last tool is a software program (www.adjuvantonline.com) which can calculate
a 10-year survival probability based on the patient’s age, co-morbidities, tumor size, grade
and ER status.20
The prognostic model is constructed using the risk estimates based on theobserved overall survival from thousands of breast cancer patients, recorded in the SEER
database, and was recently validated on more than 4000 breast cancer patients from British
Columbia.21 To distinguish a low-risk group from a high-risk group using Adjuvant!, the
TRANSBIG consortium decided the following: a low-risk group would be defined as patients
with a 10-year breast cancer survival of at least 88% for estrogen receptor (ER)-positive
patients and at least 92% for ER-negative patients. The rationale for these 2 different cutoffs
is the assumption that ER-positive patients would now all receive hormonal treatment
(with an estimated average absolute 10-year survival benefit of 4%) and patients in this
validation series were all untreated.19

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 27/248
Chapter 2
30
After adjustment for the clinical risk groups defined by Adjuvant!, the hazard ratios for
overall survival and time to distant metastases given by the 70-gene profile were 2.13
(95% CI 1.19-3.82) and 2.63 (95% CI 1.45-4.79), respectively. Moreover, patients in the
good-prognosis group according to the 70-gene profile had a 10-year survival rate of
88% and 89%, respectively, for low and high clinical risk as classified by Adjuvant!. On the
other hand, patients in the poor-prognosis group defined by the 70-gene profile had a
10-year survival rate of 69%, for both low and high clinical risk defined by Adjuvant!. These
findings suggest that the 70-gene profile predicts disease outcome independently of the
clinicopathological criteria.
The median follow-up time in the original series was less than half that of this validation
series (6.7 years versus 13.6 years, respectively). Therefore, the 70-gene profile hazard ratios
were also calculated with arbitrary censoring of all observations at different time points.
A strong time dependency of the 70-gene profile was observed, with adjusted HR of
4.68 and 16.99 at 5 years, and 3.5 and 3.46 at 10 years for time to distant metastases and
overall survival, respectively, suggesting a better prediction of early distant metastases (i.e.
occurring during the first five years) by the 70-gene profile. The different duration of follow-
up could be a plausible explanation for the discrepancy in hazard ratios between the first
validation series and this independent validation series.
The results of this independent validation strengthen the previous findings that the 70-
gene profile is a strong independent prognostic marker in early stage breast cancer, also in
patients up to the age of 61. The substantiation of the prognostic value in this independent
validation study was a prerequisite for the initiation of a large prospective validation study,the MINDACT trial.
In the meantime, two other prognostic gene expression signatures were developed, using
the Affymetrix microarray platform: the 76-gene Veridex/Rotterdam signature22 and the
Genomic Grading Index.23
To decide which signature would be the best tool to move forward with in the large,
prospective MINDACT trial, the TRANSBIG consortium performed the retrospective
validation of these two signatures using the same methodology and the same patient
population as described for the 70-gene profile. The results have shown that the
three signatures performed in quite a similar way, all being superior to the classicalclinicopathological evaluation and all possess a strong time dependency (are better
predictors of early relapse).22 Since no significant differences were seen in the performances
of the three signatures and the 70-gene profile test is robust, with a good interlaboratory
reproducibility, and available for patient diagnostic testing, even as an FDA approved test,24
the TRANSBIG consortium has decided to move forward with this tool in the MINDACT trial
(Table 1).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 28/248
Development of the MammaPrint
31
2
Table 1. Summary of development and validation of the 70-gene profile.
Nature paper8 NEJM paper7 TRANSBIG paper19
Purpose Development of breast
cancer prognosis 70-gene
profile
Validation of the 70-gene
profile in consecutive series
of breast cancer patients
Independent European
validation of the 70-gene
profile
Patient & tumor
characteristics
n = 78,
< 55 years,
pT1-2,
node-negative,
50% ER-positive
n = 295,
< 53 years,
pT1-2,
node-negative/node-
positive,
77% ER-positive
n = 302,
< 61 years,
pT1-2,
node-negative,
70% ER-positive
Year of diagnosis 1983-1996 1984-1995 < 1999
Adjuvantsystemic
treatment
Chemotherapy 4%hormonal therapy 3%
Chemotherapy 31%hormonal therapy 7%
both 7%
No adjuvant systemictreatment
Follow-up 8.7 years (mean) in the
good- prognosis group
6.7 years (median) 13.6 years (median)
Good profile 35 (45%) 115 (39%) 111 (37%)
Comments Multivariate OR of 18
(95% CI: 3.3-94; p = 1.4 *
10-4) for distant metastases
< 5 years
DMFS by 70-gene profile
at 10 years: poor-prognosis
profile 55% (±4.4), good-
prognosis profile 95%
(±2.6).
Multivariate HR for distant
metastases as first event 4.6
(95% CI: 2.3-9.2; p < 0.001)
(poor versus good profile)
DMFS by 70-gene profile
at 10 years: poor-prognosis
profile 69%, good-
prognosis profile 88%.
Univariate HR for overall
survival 2.79
(95% CI: 1.60-4.87; p < 0.001)
Strong time dependency
ER, estrogen receptor; OR, odds ratio; HR, hazard ratio; DMFS, distant metastases-free survival; CI, confidence
interval.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 29/248
Chapter 2
32
Implementation of 70-gene Profile in Daily Clinical Practice Requires Adjustments to
Standard Procedures
In addition to thorough validation studies, the implementation of a new test in daily clinical
practice should also be feasible, before it can be applied in a prospective trial. One major
obstacle for the implementation of microarray techniques such as the 70-gene profile is
the requirement for good quality RNA. Since RNA is very unstable, the tumor tissue must
be preserved either by snap freezing or in a special preservation fluid based on RNAlater®
(Qiagen), rather than in paraffin. The logistics for the collection of fresh frozen tissue is
complex and varies from hospital to hospital. Therefore, performing microarray analysis,
especially on a real-time basis, can cause some logistical problems such as insufficient
freezing procedures, or transport-related issues. Thus, close collaboration between
pathologists, surgeons and oncologists is of paramount importance.
To investigate whether MammaPrint™ could be implemented in daily clinical practice,
the Netherlands Cancer Institute (with financial support from the Dutch Health Care
Insurance Board) performed a multi-center feasibility study: the RASTER study (Figure 1).
The first aim of this study was to assess the feasibility of collecting good quality tissue
from several community hospitals in the Netherlands to be used to perform the 70-gene
profile analysis.25 In this RASTER study, the so-called Constructive Technology Assessment
(CTA) was used as a tool to facilitate the introduction of the 70-gene profile in daily
clinical practice by evaluating aspects of the dynamics of its implementation, such as
communication, logistics, juridical-ethical matters and cost effectiveness.26 The results ofthese evaluations will be used in decision-making concerning the large-scale application
of the 70-gene profile in daily clinical practice and related guidelines. Other aims of the
RASTER study were to determine the proportion of good- and poor-profile patients and
to establish the concordance between the risk assessment defined by the 70-gene profile
and the one defined by the Dutch breast cancer guidelines, which are based on common
clinicopathological criteria.25
Lymph node-negative breast cancer patients under the age of 61, with a T1 or T2 tumor,
were eligible. A tumor sample from the excised specimen was obtained from all patients,
using a 6 mm biopsy punch, and placed in the commercially available preservationfluid at room temperature. Subsequently, the sample was sent by conventional mail to
the NKI, were it was frozen in liquid nitrogen and stored at -80°C until processing. The
MammaPrint™ was performed at Agendia and patients were classified into good- and poor-
prognosis groups. Preliminary results show the feasibility of collecting good quality tissue
for microarray analysis from several community hospitals. A minority of the samples were
lost due to processing errors, such as initial storage in formalin resulting in an insufficient
RNA quality.25,27 The study ended in December 2006 and the final results are expected in
due course.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 30/248
Development of the MammaPrint
33
2
Figure 1. RASTER study design.
From Sauter G and Simon R. Predictive Molecular Pathology. N Engl J Med 347(25): 1995-1996, 2002.Copyright © 2002 Massachusetts Medical Society. All rights reserved. Adapted with permission,
2007.
The Prospective Validation of the 70-gene Profile in a Large Randomized Clinical
Trial: the MINDACT Study
The 70-gene profile has been extensively validated in a retrospective series. Furthermore,
the logistics concerning fresh frozen tissue collection were tested and adjusted wherenecessary. The final step before the implementation of the 70-gene profile in clinical
practice is its prospective validation in the MINDACT trial. This trial is a multicentric large
prospective randomized study, comparing the 70-gene profile with currently used tools for
selecting lymph node-negative breast cancer patients for adjuvant systemic treatment. The
primary aim of the study is to show that patients defined as at low risk using the 70-gene
profile but who are at high risk according to the current clinicopathological criteria can be
safely spared chemotherapy, without deterioration of the clinical outcome. The study will
enroll 6,000 node-negative breast cancer patients who will have their risk assessed by both
the 70-gene profile and the currently used clinicopathological criteria through an updated
Good signature
Low risk
Poor signature
High risk DNA Microarray
70 genes
Dutch Health Care Insurance Board (CVZ)/ NKI
‘Raster trial’
Tumor RNA
Unfixed sample of
tumor tissue
Surgical removal oftumor tissue
Labeled tumorcDNA or cRNA
Labeled control
cDNA or cRNA

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 31/248
Chapter 2
34
version of Adjuvant! Online. We estimate that about 55% will be classified as at high risk by
both methods and these patients will be offered adjuvant chemotherapy; about 10% will be
classified as at low risk by both methods and will not be offered adjuvant chemotherapy. The
patients with a discordant risk assessment (approx. 35%), i.e. a high genomic risk (according
to the 70-gene profile) and a low clinical risk (according to Adjuvant! software) or vice versa
(low genomic risk and high clinical risk) will be randomized for the treatment decision tool.
In other words, 50% of those patients will receive adjuvant treatment according to their
genomic risk and 50% will be treated according to their clinical risk (Figure 2).
Other objectives of the study are related to the type of adjuvant systemic treatment. A
second randomization will compare an anthracycline-based regimen to a docetaxel-
capecitabine regimen, which might be associated with increased efficacy and reduced
long-term side-effects, particularly cardiotoxicity and leukemia. A third randomization,
which will be offered to all postmenopausal hormone receptor-positive patients, will
compare 2 years of tamoxifen followed by 5 years of letrozole to 7 years of letrozole
upfront (Figure 2). Women aged 18-70 years with an operable invasive breast carcinoma and
a negative sentinel node or axillary clearance are eligible. An overview of the MINDACT
trial was recently published in Nature Clinical Practice of Oncology, explaining in detail the
rationale behind the study design.28
An additional and important effort has been made to perform not only the analysis
of the 70-gene profile, but whole genome arrays for all 6,000 eligible patients. This will
potentially allow for the discovery of new genomic profiles with prognostic or predictive
value and eventually new drug targets. Fresh frozen tissue, paraffin-embedded tissue andblood samples from all 6,000 patients will be stored in an independent biobank repository,
representing an invaluable resource for future research.
The Collection of Fresh Frozen Tissue for the MINDACT Trial
Although microarray experiments are becoming more and more standardized, operator
and technical variability are well known to influence the measurement of gene expression
levels. For all samples in the MINDACT trial, RNA isolation, quality controls and microarray
analysis will be performed at Agendia, Amsterdam, to avoid the bias of potentialinterlaboratory reproducibility. Consequently, tumor samples from all over the world will
be shipped to the Netherlands within a fixed timeframe. Additionally, since one of the aims
of the MINDACT trial is the establishment of a biological material bank for future research,
also in the field of proteomics, frozen tumor samples and blood samples will be collected
from all patients. Preservation of the tumor samples in RNAlater® might influence several
processes in the tissue, such as the level of proteins, therefore, temporary preservation
in RNAlater®, as tested in the RASTER study, is not suitable and material frozen in liquid
nitrogen will be mandatory for the MINDACT trial.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 32/248
Development of the MammaPrint
35
2
To test the logistics of collection, freezing and shipment of the samples, the authors
performed a logistics pilot study in 6 European hospitals. For this feasibility study, patients
with early stage breast cancer under the age of 71 were eligible. All patients signed an
informed consent to donate a piece of tumor tissue for research. The pathologist obtained
a representative tumor sample within one hour of surgery, using a 6mm biopsy punch,
according to a standardized procedure. The tumor samples were snap frozen in liquid
nitrogen and stored at -80°C until shipment. All samples were shipped on dry ice by a
specifically contracted courier specialized in transportation of frozen material at -80 °C. At
Agendia, the percentage of tumor cells in the samples was determined as described by Van
‘t Veer and colleagues.8 When the sample was representative of the tumor ( i.e. tumor cell
≥ 50%), RNA was isolated and, after measurement of its quality and quantity, the 70-gene
profile was performed. The primary endpoint of this logistics pilot study was the success
rate of hybridization. Preliminary results show that, in general, it is feasible to collect and
ship good quality fresh frozen tumor samples from several locations throughout Europe to
Amsterdam. The procedures (of tissue collection, freezing and transportation) tested in this
study formed the basis of the standard operating procedures written for the MINDACT trial.
The final results of this pilot study will be published in 2007.
Future Prospects
The MINDACT study will determine the clinical relevance of the 70-gene profile and its
prognostic value compared to the currently available prognostic clinicopathologicalcriteria. Moreover, as tumor and blood material and whole genome microarray data will
be collected from all patients, a valuable bank of material will be established, providing an
opportunity for the identification of predictive gene expression profiles and potential drug
targets. Nowadays, the choice among treatment options is based upon patient and tumor
characteristics, such as age and estrogen receptor status, but overall it is extrapolated from
the percentage of risk reduction measured in a large population to the individual patient.
In the future, we might be able to identify the genomic fingerprint of each individual tumor,
telling us not only if a given patient needs adjuvant systemic treatment, but also which
treatment will have the best response and which treatment should be avoided because ofpotentially serious side-effects.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 33/248
Chapter 2
36
Figure 2. MINDACT study design.Abbreviations: R-T = Treatment decision randomization; CT = Chemotherapy
Acknowledgements
The studies mentioned in this article were supported by the European Commission
Framework Programme VI, the Center of Biomedical Genetics, the Dutch Health Care
Insurance Board, the Dutch National Genomic Initiative - Cancer Genomics Program, the
Breast Cancer Research Foundation and the European Organisation for Research and Treatment of Cancer (EORTC) - Breast Cancer Group. S. Mook was partially supported by the
traineeship program of TRANSBIG network. The authors thank the numerous individuals
who have contributed to the studies mentioned in this review, especially those from
the TRANSBIG consortium and the EORTC, and to all the patients who have and still are
participating in these studies.
Conflicts of Interest
Dr. L.J. Van ’t Veer is a named inventor on a patent application for MammaPrint™ and reports
holding equity in Agendia BV.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 34/248
Development of the MammaPrint
37
2
References
1. Goldhirsch A, Glick JH, Gelber RD, et al . Meeting highlights: International expert consensus on the
primary therapy of early breast cancer 2005. Ann Oncol 2005; 16: 1569-1583.
2. Carlson RW and McCormick B. Update: NCCN breast cancer clinical practice guidelines. J Natl Compr Canc
Netw 2005; 3 Suppl 1: S7-11.
3. NCCN Clinical Practice Guidelines in Oncology. Breast Cancer V.I.2007. www.nccn.org 2007.
4. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for
early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet
2005; 365: 1687-1717.
5. West M, Blanchette C, Dressman H, et al . Predicting the clinical status of human breast cancer by using
gene expression profiles. Proc Natl Acad Sci USA 2001; 98: 11462-11467.
6. Wang Y, Klijn JG, Zhang Y, et al. Gene-expression profiles to predict distant metastasis of lymph-node-
negative primary breast cancer. Lancet 2005; 365: 671-679.
7. Van de Vijver MJ, He YD, Van ‘t Veer LJ, et al . A gene-expression signature as a predictor of survival in
breast cancer. N Engl J Med 2002; 347: 1999-2009.
8. Van ‘t Veer LJ, Dai H, Van de Vijver MJ, et al . Gene expression profiling predicts clinical outcome of breast
cancer. Nature 2002; 415: 530-536.
9. Sotiriou C, Neo SY, McShane LM, et al . Breast cancer classification and prognosis based on gene
expression profiles from a population-based study. Proc Natl Acad Sci USA 2003; 100: 10393-10398.
10. Sorlie T, Perou CM, Tibshirani R, et al . Gene expression patterns of breast carcinomas distinguish tumor
subclasses with clinical implications. Proc Natl Acad Sci USA 2001; 98: 10869-10874.
11. Paik S, Shak S, Tang G, et al . A multigene assay to predict recurrence of tamoxifen-treated, node-negative
breast cancer. N Engl J Med 2004; 351: 2817-2826.
12. Jansen MP, Foekens JA, Van Staveren IL, et al . Molecular classification of tamoxifen-resistant breast
carcinomas by gene expression profiling. J Clin Oncol 2005; 23: 732-740.
13. Huang E, Cheng SH, Dressman H, et al . Gene expression predictors of breast cancer outcomes. Lancet
2003; 361: 1590-1596.
14. Chang JC, Wooten EC, Tsimelzon A, et al . Gene expression profiling for the prediction of therapeutic
response to docetaxel in patients with breast cancer. Lancet 2003; 362: 362-369.
15. Hughes TR, Mao M, Jones AR, et al . Expression profiling using microarrays fabricated by an ink-jetoligonucleotide synthesizer. Nat Biotech 2001; 19: 342-347.
16. Simon R, Radmacher MD, Dobbin K, McShane LM. Pitfalls in the use of DNA microarray data for
diagnostic and prognostic classification. J Natl Cancer Inst 2003; 95: 14-18.
17. Eifel P, Axelson JA, Costa J, et al . National Institutes of Health Consensus development conference
statement: Adjuvant therapy for breast cancer, November 1-3, 2000. J Natl Cancer Inst 2001; 93: 979-989.
18. Goldhirsch A, Glick JH, Gelber RD, Coates AS, Senn HJ. Meeting highlights: International consensus
panel on the treatment of primary breast cancer. J Clin Oncol 2001; 19: 3817-3827.
19. Buyse M, Loi S, Van ‘t Veer L, et al . Validation and clinical utility of a 70-gene prognostic signature for
women with node-negative breast cancer. J Natl Cancer Inst 2006; 98: 1183-1192.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 35/248
Chapter 2
38
20. Ravdin PM, Siminoff LA, Davis GJ, et al . Computer program to assist in making decisions about adjuvant
therapy for women with early breast cancer. J Clin Oncol 2001; 19: 980-991.
21. Olivotto IA, Bajdik CD, Ravdin PM, et al . Population-based validation of the prognostic model ADJUVANT!
for early breast cancer. J Clin Oncol 2005; 23: 2716-2725.
22. Desmedt C, Piette F, Loi S, et al . Strong time dependence of the 76-gene prognostic signature for node-
negative breast cancer patients in the TRANSBIG multicenter independent validation series. Clin Cancer
Res 2007; 13: 3207-3214.
23. Sotiriou C, Wirapati P, Loi S, et al . Gene expression profiling in breast cancer: understanding the molecular
basis of histologic grade to improve prognosis. J Natl Cancer Inst 2006; 98: 262-272.
24. Couzin J. Diagnostics: Amid debate, gene-based cancer test approved. Science 2007; 315: 924.
25. Bueno de Mesquita JM, Van De Vijver MJ, Peterse JL, et al . Feasibility of gene expression profiling in
community hospitals; preliminary results of a pilot study in N0 breast cancer patients (abstract 309).
Breast Cancer Res Treat 2005 2005; 94 (Suppl 1): A 309.
26. Douma KFL, Karsenberg K, Bueno de Mesquita JM, Hummel JM, Van Harten WH. Methodology of
constructive technology assessment in health care. Int J Technol Assess in Health Care 2007; 23: 162-168.
27. Van de Vijver M. Gene-expression profiling and the future of adjuvant therapy. Oncologist 2005; 10: 30-34.
28. Bogaerts J, Cardoso F, Buyse M, et al . Gene signature evaluation as a prognostic tool: challenges in the
design of the MINDACT trial. Nat Clin Pract Oncol 2006; 3: 540-551.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 36/248
Chapter 3
Daily clinical practice of fresh tumor tissue
freezing and gene expression profiling;
logistics pilot study preceding
the MINDACT trial
Stella Mook
Hervé Bonnefoi
Giancarlo Pruneri
Denis Larsimont
Janusz Jaskiewicz
Maria D Sabadell
Gaëten MacGrogan
Laura J. Van ’t VeerFatima Cardoso
Emiel J.Th. Rutgers
Eur J Cancer 2009; 45: 1201-1208.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 37/248
Chapter 3
42
Abstract
Purpose
The 70-gene prognosis-signature is a prognostic tool for early breast cancer analysis.
In addition to scientific evidence, implementation of the signature in clinical trials and daily
practice requires logistical feasibility. The aim of our study was to test logistics for gene
expression profiling on fresh frozen tumor tissue in the preparation for the prospective,
multinational Microarray In Node-negative Disease may Avoid ChemoTherapy (MINDACT)
trial.
Methods
Sixty-four patients were included in six European hospitals. Fresh frozen tumor samples
were shipped on dry ice to Agendia B.V., where RNA was isolated and subsequently
hybridized on the 70-gene prognosis-signature (MammaPrint™).
Results
Tumor samples were obtained in 60 of 64 patients. Among the 60 samples, 11 contained
insufficient tumor cells (< 50%) and three contained insufficient RNA quality. All 46 samples
eligible for genomic profiling were successfully hybridized, and the results were reportedon average within 4-5 d.
Conclusion
Gene expression profiling on fresh frozen tissue is feasible in daily clinical practice.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 38/248
Logistics of gene expression profiling
43
3
Introduction
In the past 20 years, important advances have been made in the knowledge of the biology
of breast cancer. Using new high-throughput techniques, such as microarray-based
gene expression profiling, both prognostic and predictive profiles were established, and
breast cancer was re-classified based on molecular characteristics.1-16 One of these gene
expression classifiers is the 70-gene prognosis-signature (MammaPrint™).2,3 This 70-gene
dichotomous classifier can accurately distinguish breast tumors with a high metastatic
capacity from tumors with a low risk of developing distant metastases, by measuring the
expression level of 70 genes in tumor tissue. Several retrospective validation studies have
confirmed its prognostic value.3,17-20
Implementation of gene expression profiles requires logistical feasibility, in addition to
scientific evidence provided by validation studies. An essential part of this logistics is the
procurement of fresh frozen tissue as source of high-quality RNA. Traditional fixation of
fresh tissue in formaldehyde results in degradation of RNA and cross-linking, which makes
it unsuitable for comprehensive microarray analysis.21 Moreover, RNA becomes heavily
fragmented during storage of paraffin-embedded tissue.22 In addition, slow freezing of
samples promotes the formation of ice crystals, which can also provoke RNA damage.23
Consequently, collection of snap-frozen tissue or fresh tissue preserved in RNA preservation
fluid, such as RNARetain™ (Asuragen Inc., TX, USA),24 is at present mandatory to obtain high-
quality RNA and successful gene expression profiling. Recently, Bueno-de-Mesquita and
colleagues described the successful implementation of RNARetain™ tissue preservationand centralized MammaPrint™ testing for 16 community hospitals in the Netherlands for
the prospective RASTER trial.24 Evaluation of logistics of frozen tissue collection, centralized
microarray testing and swift reporting of results in the preparation of a multinational
multicentre clinical trial is described here.
In 2007, the MINDACT trial (Microarray In Node-negative Disease may Avoid ChemoTherapy;
EORTC 10041/ BIG 3-04) started to prospectively evaluate the 70-gene prognosis-signature
as a risk assessment and decision-making tool.25-27 This trial will enroll 6000 breast cancer
patients throughout Europe, who will have their risk of disease recurrence assessed by
both traditional clinicopathological criteria and the 70-gene prognosis-signature. Sincedecision-making for adjuvant treatment is based on both the risk assessments, the 70-
gene prognosis-signature test result has to be available within a fixed timeframe suitable
for daily clinical practice. Moreover, to avoid interlaboratory variability, which may
artificially influence gene expression levels, all samples are obtained and frozen at local
sites and shipped to Agendia B.V., Amsterdam, for RNA isolation and microarray analysis.
Consequently, participation in the MINDACT trial demands personnel at local hospitals who
will collect and freeze tumor samples. These local procedures, frozen sample shipment and
sample analysis within a fixed timeframe entail complex logistics that requires a thorough
organization.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 39/248
Chapter 3
44
In the preparation for the MINDACT trial, we conducted a pilot study to test the logistics
for gene expression profiling in a multicentre and multinational setting. The first aim of
this pilot study was to test and if necessary to improve the logistics to collect good-quality
fresh frozen tissue at individual hospitals for microarray testing. The second aim was to
determine the proportion of samples that was hybridized successfully. The last aim was to
define Standard Operating Procedures (SOPs) for the tissue logistics in the MINDACT trial.
Together with the Dutch RASTER trial,24 this pilot study provided crucial information for the
feasibility of the MINDACT trial.
Patients and Methods
This logistics pilot study was coordinated by the Netherlands Cancer Institute (NKI) and was
conducted in six European hospitals. The study was approved by the institutional ethical
review board of each participating hospital, and all patients gave their written informed
consent before surgery, for the donation of a piece of tumor tissue to test the logistics for
genomic profiling.
Patients
Women under the age of 71 years at diagnosis with a unifocal, unilateral pT1-pT2, invasive
breast carcinoma and a clinically negative axillary lymph node status were eligible forinclusion. Patients with carcinoma in situ were eligible, provided that invasive cancer was
present. Patients who received neoadjuvant therapy were not included. Each hospital
included at least eight patients.
On-site training
Before the start of the study, the study coordinator organized on-site instruction
meetings in each participating hospital. These instruction meetings were attended by
a multidisciplinary team, i.e. breast surgeons, medical oncologists, pathologists, datamanagers and research nurses. During this instruction visit, the logistical scheme was
discussed and incorporated in the local standard procedures. Additionally, all study-
specific standard procedures were explained in detail in a manual of operations and were
summarized on provided pocket summaries, to support standardized procedures for tissue
collection, freezing and shipment.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 40/248
Logistics of gene expression profiling
45
3
Figure 1A. Biopsy puncher for standardized tumor sampling.
B. Tumor specimen after sampling, using the 6 mm biopsy puncher (by courtesy of J.F. Egger).
C. Hematoxylin and eosin (H&E) stained section of the tumor specimen (shown in B). After
sampling, intact morphology is shown, and appropriate grading and staging of the tumor are
allowed (by courtesy of J.F. Egger).
A
B
C

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 41/248
Chapter 3
46
Pre-assembled kits
The study coordinator provided hospitals with pre-assembled sample kits for each patient,
consisting of all case report forms (CRFs), a 6 mm biopsy puncher (Figure 1A) and a printed
sticker sheet with a unique identification number (Sample ID), suitable for freezing in liquid
nitrogen and prolonged storage at -80°C.
Tumor sampling
After surgical resection, tumor specimens were immediately transported from the
operating room to the pathology department in a tumor container without fixatives, e.g.
formalin. To ensure standardized tumor sampling, 6 mm biopsy punchers were provided
(Figure 1A). The pathologist obtained a tumor sample within 1 h of surgery, using this biopsy
puncher. Samples were placed in an Eppendorf tube, labeled with a sample ID sticker.
For tumors smaller than 1 cm (at macroscopic examination), a 3 mm biopsy puncher was
allowed to obtain a sample. Obviously, standard diagnostic pathology examination had
priority over the procurement of a research sample, i.e. the pathologist only obtained a
tumor sample for gene expression profiling when he/she judged that there was a sufficient
amount of tumor tissue.
Snap-freezing and storage
Eppendorf tubes containing tumor samples were snap-frozen by submerging the tubes
in liquid nitrogen for at least 1 min. After snap-freezing of the sample, the total time from
transportation of tissue to the pathology department till freezing of the samples was
recorded. Samples were stored in a -80°C freezer until shipment.
Shipment
Frozen samples were shipped on dry ice by a contracted courier, specialized in
transportation of frozen material. Samples were shipped as ‘Biological Substance CategoryB UN 3373’ (Exempt Human Specimen) in the applicable packaging material provided by
the courier, i.e. an inner sealed plastic bag with absorbent material, an outer packaging
and a polystyrene box with dry ice. Packaging and shipment complied with International
Air Transport Association (IATA) criteria (http://www.iata.org). Samples were shipped as a
batch of three samples or once in every 3 weeks, to reduce costs. Samples were shipped
and delivered at Agendia B.V., Amsterdam, within 1 working day after collection at the local
hospitals. Samples collected on Friday were delivered on Monday. The amount of dry ice
was maintained during the weekend, to prevent thawing of the samples.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 42/248
Logistics of gene expression profiling
47
3
Microarray analyses
Upon receipt of the samples at Agendia B.V., outer and inner packaging and Eppendorf
tubes were checked for damage and for the presence of an appropriate sticker with unique
sample ID. Samples were processed for microarray analysis, and the number of days required
to generate a 70-gene prognosis-signature result was registered. Frozen sections were cut
and stained with hematoxylin and eosin (H&E), before and after cutting the sections for
RNA isolation, to confirm the presence of tumor and to determine tumor cell percentage.
If the mean tumor cell percentage was < 50%, again two frozen sections were cut and
stained with H&E before and after cutting the sections for RNA isolation. Samples with less
than 50% tumor cells determined in duplicate were excluded from further analysis. RNA
isolation, amplification and labeling were performed at Agendia Laboratories, as described
previously.2,28 RNA quality was assessed using the Agilent bioanalyzer. Samples without
sample ID stickers or samples with damaged packaging material, less than 50% tumor cells
or insufficient RNA quality (RIN < 7) were excluded from further processing.
A total of 200 ng of tumor RNA was co-hybridized with a standard reference to a custom-
designed microarray (MammaPrint™), including eight identical subarrays, each containing
oligonucleotide probes for the 70 genes in triplicate.28 The standard reference sample
consisted of pooled RNA of 105 primary breast tumors selected from patients of the
retrospective validation series.3 For this feasibility study, results were only presented
as successful hybridization or exclusion, hence no good- or poor prognosis-signature
was reported. Consequently, all patients included in this feasibility study were treatedaccording to the standard national guidelines. The above-mentioned standard procedures
for the collection of good-quality fresh frozen tumor tissue for gene expression profiling
are shown in Figure 3, left panel.
Results
Between November 2005 and November 2006, 68 patients were enrolled in six hospitals
throughout Europe. Among the 68 patients, four were excluded (one patient had withdrawninformed consent, one patient was aged > 71 years and two had no detectable malignancy).
All 64 eligible patients underwent the surgery. Baseline characteristics are shown in Table 1.
The pathologist was able to obtain a tumor sample in 60 patients (94%): 55 samples were
obtained using a 6 mm biopsy puncher and five samples were obtained using a 3 mm
biopsy puncher. Among the 60 tumor samples, 14 samples were inadequate (11 samples
contained less than 50% tumor cells and three samples had insufficient RNA quality),
whereas all 46 adequate samples were successfully hybridized on the MammaPrint™. None
of the samples were lost due to processing errors, such as initial storage in formalin. In 4
of the 64 eligible patients no tumor sample was obtained; three patients had tumors that

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 43/248
Chapter 3
48
were too small to obtain a tumor sample and in one case the pathologist forgot to take a
tumor sample. A summary is given in Figure 2.
Remarkably, all 3 mm samples were representative and hybridized successfully. There was
no significant differences in tumor size between the samples that were inadequate because
of insufficient tumor cells and samples that were hybridized successfully (mean diameter
21 mm versus 19 mm; p = 0.7) (Table 1). The median time to freeze a tumor sample was 20 min
(range 5-235 min). For three samples that had poor RNA quality, the freezing time was <
20 min. The median time to generate and report a 70-gene prognosis-signature result from
the time of arrival at Agendia laboratories was 4 working days (range 3-14; mean 5.2).
Table 1. Baseline characteristics
Successful hybridization No hybridization P
N % N %
Age ns
≤ 50 years 16 35 4 29
51 - 60 years 14 30 3 21
61 - 70 years 16 35 7 50
Tumor size ns
pT1 (≤ 20mm) 29 66 7 54
pT2 (> 20mm) 15 34 6 46
Histology
Invasive ductal 38 83 8 57
Others 6 13 5 36
Missing 2 4 1 7
Grade ns
Grade 1 7 15 2 14
Grade 2 22 48 7 50
Grade 3 14 30 3 22
Missing 3 7 2 14
Estrogen receptor status ns
Positive 36 78 9 64
Negative 6 13 2 14
Missing 4 9 3 22
Lymph node status ns
Positive 13 28 3 22
Negative 31 68 10 71
Missing 2 4 1 7
Total 46 100 14 100
Missing value were not used for calculation of p-values.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 44/248
Logistics of gene expression profiling
49
3
F i g u r e
2 .
F l o w d i a g r a m o
f p a t i e n
t s e n r o l l e d a n d t u m o r s a m p l e s .
I n c l u s i o n
N = 6 8
E l i g i b l e
N = 6 4
S u r g e r y
N = 6 4
N o s a m p l e
n = 4 ( 4 / 6 4 = 6 % )
P r o c u r e m e n t o f
s a m p l e
n = 6 0 ( 6 0 / 6 4 = 9 4 % )
S h i p m e n t
n = 6 0 ( 6 0 / 6 4 = 9 4 % )
6 m m B i o p s y p u n c h e r
n = 5 5 ( 5 5 / 6 4 = 8 6 % )
3 m m B i o p s y p u n c h e r
n = 5 ( 5 / 6 4 = 8 % )
E x c l u d e d : < 5 0 %
t u m o r c e l l s
n = 1 1 ( 1 1 / 6 4 = 1 7 % )
E x c l u d e d : I n s u f f i c i e n t
R N A q u a l i t y
n = 3 ( 3 / 6 4 = 5 % )
R N A o b t a i n e d
n = 4 1 ( 4 1 / 6 4 = 6 4 % )
R N A o b t a i n e d
n = 5 ( 5 / 6 4 = 8 % )
H y b r i d i z a t i o n
s u c c e s s f u l
n =
4 6 ( 4 6 / 4 6 = 1 0 0 % )
T u m o r t o o s m a l l t o
o b t a i n s a m p l e
n = 3 ( 3 / 6 4 = 5 % )
F o r g o t t e n t o t a k e
s a m p l e
n = 1 ( 1 / 6 4 = 2 % )
E x c l u s i o n ( n = 4 )
−
N o m a l i g n a n c y d e t e c t e d ( n = 2 )
−
W i t h d r a w n i n f o r m e d c o n s e n
t ( n = 1 )
−
A g e d > 7 1 y e a r s ( n = 1 )

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 45/248
Chapter 3
50
Figure 3. Flow chart of standardized procedures for obtaining good-quality fresh frozen tumor
samples for microarray analyses (left panel) and adaptations to local standard procedures (right
panel).
Procedures Adaptations
Signed informed consent
Surgery
Transfer of tumor specimen in DRY tumorcontainer from OR to pathology department
Procurement of tumor sample within 1 hour
of surgery, following standard procedures
Tumor sampling using 6 mm biopsy puncher
Tumor sample in Eppendorf tube, labeled
with ID sticker
Submerge Eppendorf tube with tumor
sample in liquid nitrogen for at least 1
minute
Storage of tumor sample in -80°C freezer
Inform OR personnel that patient
participates in study
Tumor container WITHOUT fixative (e.g.formaline), labeled with study number
Time limit for tissue processing
− Selection of representative, non-sclerotic,
non-necrotic tumor area for sampling
− Availability biopsy puncher
Availability of stickers suitable for freezing in
liquid nitrogen and storage at -80°C
Availability of liquid nitrogen and personal
protective equipment at pathology
department
Availability of -80°C freezer

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 46/248
Logistics of gene expression profiling
51
3
Discussion
Our study showed that collection and shipment of fresh frozen tumor tissue for gene
expression profiling are feasible in a multicentre and multinational practice setting, with
a success rate of 72% (46 out of 64). Provided that the pathologist was able to obtain a
tumor sample, the success rate increased to 77% (46 out of 60). When RNA was obtained, all
samples were successfully hybridized and a gene expression signature result was obtained
in 100% (46 out of 46). The main reason for sample failure was a non-representative tumor
sample; 18% (11 out of 60) of the samples contained < 50% tumor cells. This proportion of
non-representative samples is in agreement with the proportion reported by a previous
feasibility study.24
The pathologist obtains a sample after macroscopic evaluation of the tumor specimen
(Figure 1B). As shown in Figure 1C , tumor sampling does not alter morphology and allows
appropriate grading and staging of the tumor. The best area for sampling is the periphery
of the tumor, given that the central part is often sclerotic or necrotic and lack tumor
cells. However, sampling in the periphery of the tumor could increase the amount of
surrounding stroma in the sample. The balance between a sufficient amount of tumor cells
and a limited amount of stromal tissue can be improved in part by training and repetition.
Additionally, recent research has shown that samples containing > 30% tumor cells are
suitable for reliable 70-gene prognosis-signature read-out (Amendment 1, MINDACT trial;
EORTC 10041/ BIG 3-04). As a consequence, the cut-off for tumor cell percentage in the
MINDACT trial has been lowered to 30%, and hence sample inclusion will be increased. Inour study, inclusion of samples containing 30-50% tumor cells would have resulted in five
additional hybridizations (51 out of 60 = 85% success rate).
Although H&E stained sections of the material sampled for profiling were used to determine
if the sample contained a certain amount of malignant tissue, a tumor in itself can be very
heterogeneous.29 To test if the biopsy sample was also representative for the tumor in its
entirety, we compared the final pathology report with the genomic test result. In this pilot
study, the profile was associated with grade and estrogen receptor status (ER) ( p < 0.001),
which is in good agreement with previous validation studies, that have shown a strong
association between the profile and grade, ER status and disease outcome.3,17-20
Although gene expression profiling is becoming more and more standardized, operator
and technical variability are well known to influence the measurement of gene expression
levels.30-32 To avoid potential interlaboratory bias, all samples in the MINDACT will be
shipped on dry ice to Agendia, Amsterdam, where quality controls, RNA isolation and gene
expression analysis will be performed. Consequently, frozen tumor samples have to be
shipped from all over the world to Amsterdam within a fixed timeframe. In this pilot study,
samples were shipped once in every 3 weeks or as a batch, therefore time from sample
arrival at Agendia till reporting of the genomic test was measured, instead of the interval
between surgery and genomic test result. In our study, all tumor samples were delivered

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 47/248
Chapter 3
52
within one working day. Furthermore, a 70-gene prognosis-signature result was available
after a median of 4 d, thereby showing the feasibility of implementation of this signature
in clinical trials and daily practice, with regard to the needed timeframe for clinical decision
making.
Recently, Bueno de Mesquita and colleagues have shown that the collection of fresh tumor
tissue is feasible in community hospitals in the Netherlands. 24 In contrast to our study,
tumor samples were placed in a commercially available preservation fluid (RNARetain™) at
room temperature, and were sent by conventional mail to the Netherlands Cancer Institute,
where samples were subsequently frozen in liquid nitrogen. Although preservation of
tumor samples in RNARetain™ does not influence gene expression measurements,33,34 it is
unclear whether it might influence levels of proteins. Since one of the aims of MINDACT is
the establishment of a biological materials bank for future research, including proteomics,
temporarily preservation of tissue in RNARetain™ as done by Bueno de Mesquita and
colleagues is not suitable, and tumor tissue immediately frozen in liquid nitrogen was
chosen. The complex logistics involved in the collection and shipment of fresh frozen
tissue demands a thorough and detailed organization with adjustments to local standard
procedures. The major adjustments are shown in Figure 3, right panel. These adjustments
formed the basis of the standard operating procedures (SOPs) written for MINDACT.35
In conclusion, through detailed standard operating procedures, provision of necessary
devices and close collaboration between surgeons, medical oncologists, pathologists,
research nurses, data-managers and scientists, successful implementation of the logistics
for gene expression profiling on fresh frozen tissue is feasible.
Conflicts of interest statement
Laura J. Van ’t Veer is a named inventor on a patent application for MammaPrint™ and
reports holding equity in Agendia B.V.
Acknowledgements
This study was financially supported by a grant of the EORTC Breast Cancer Group. Weare indebted to the women who participated in this study. We thank J.F. Egger (Geneva
University Hospitals, Geneva, Switzerland); M.J. Piccart (Institute Jules Bordet, Brussels,
Belgium); G. Viale, A. Goldhirsh, M. Colleoni (European Institute of Oncology and University
of Milan, Milan, Italy); J. Jassem, K. Jaskiewicz (Medical University of Gdansk, Gdansk,
Poland); J. Baselga, F. Rojo (Vall d’Hebron University Hospital, Barcelona, Spain); L. Mauriac
(Institute Bergonié, Bordeaux, France) and all other doctors, nurses, and data managers for
their generous participation. We are indebted to Jillian Harrison, EORTC and Annuska Glas
from Agendia B.V. for their expert advice and to Marjanka Schmidt for critically reading the
manuscript.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 48/248
Logistics of gene expression profiling
53
3
References
1. Perou CM, Sorlie T, Eisen MB, et al . Molecular portraits of human breast tumours. Nature 2000; 406: 747-
752.
2. Van ‘t Veer LJ, Dai H, Van de Vijver MJ, et al . Gene expression profiling predicts clinical outcome of breast
cancer. Nature 2002; 415: 530-536.
3. Van de Vijver MJ, He YD, Van ‘t Veer LJ, et al . A gene-expression signature as a predictor of survival in
breast cancer. N Engl J Med 2002; 347: 1999-2009.
4. Chang JC, Wooten EC, Tsimelzon A, et al . Gene expression profiling for the prediction of therapeutic
response to docetaxel in patients with breast cancer. Lancet 2003; 362: 362-369.
5. Paik S, Shak S, Tang G, et al . A multigene assay to predict recurrence of tamoxifen-treated, node-negative
breast cancer. N Engl J Med 2004; 351: 2817-2826.
6. Chang HY, Nuyten DSA, Sneddon JB, et al . Robustness, scalability, and integration of a wound-response
gene expression signature in predicting breast cancer survival. Proc Natl Acad Sci USA 2005; 102: 3738-3743.
7. Gianni L, Zambetti M, Clark K, et al . Gene expression profiles in paraffin-embedded core biopsy tissue
predict response to chemotherapy in women with locally advanced breast cancer. J Clin Oncol 2005; 23:
7265-7277.
8. Hannemann J, Oosterkamp HM, Bosch CA, et al . Changes in gene expression associated with response
to neoadjuvant chemotherapy in breast cancer. J Clin Oncol 2005; 23: 3331-3342.
9. Iwao-Koizumi K, Matoba R, Ueno N, et al . Prediction of docetaxel response in human breast cancer by
gene expression profiling. J Clin Oncol 2005; 23: 422-431.
10. Rouzier R, Perou CM, Symmans WF, et al . Breast cancer molecular subtypes respond differently to
preoperative chemotherapy. Clin Cancer Res 2005; 11: 5678-5685.
11. Wang Y, Klijn JG, Zhang Y, et al . Gene-expression profiles to predict distant metastasis of lymph-node-
negative primary breast cancer. Lancet 2005; 365: 671-679.
12. Hess KR, Anderson K, Symmans WF, et al . Pharmacogenomic predictor of sensitivity to preoperative
chemotherapy with paclitaxel and fluorouracil, doxorubicin, and cyclophosphamide in breast cancer.
J Clin Oncol 2006; 24: 4236-4244.
13. Potti A, Dressman HK, Bild A, et al . Genomic signatures to guide the use of chemotherapeutics. Nat Med
2006; 12: 1294-1300.
14. Sotiriou C, Wirapati P, Loi S, et al . Gene expression profiling in breast cancer: understanding the molecularbasis of histologic grade to improve prognosis. J Natl Cancer Inst 2006; 98: 262-272.
15. Thuerigen O, Schneeweiss A, Toedt G, et al . Gene expression signature predicting pathologic complete
response with gemcitabine, epirubicin, and docetaxel in primary breast cancer. J Clin Oncol 2006; 24: 1839-
1845.
16. Bonnefoi H, Potti A, Delorenzi M, et al . Validation of gene signatures that predict the response of breast
cancer to neoadjuvant chemotherapy: a substudy of the EORTC 10994/BIG 00-01 clinical trial. Lancet Oncol
2007; 8: 1071-1078.
17. Buyse M, Loi S, Van ‘t Veer L, et al . Validation and clinical utility of a 70-gene prognostic signature for
women with node-negative breast cancer. J Natl Cancer Inst 2006; 98: 1183-1192.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 49/248
Chapter 3
54
18. Bueno de Mesquita JM, Linn SC, Keijzer R et al. Validation of 70-gene prognosis signature in node-
negative breast cancer. Breast Cancer Res Treat 2009; 117: 483–495.
19. Mook S, Schmidt MK, Viale G, et al . The 70-gene prognosis-signature predicts disease outcome in breast
cancer patients with 1-3 positive lymph nodes in an independent validation study. Breast Cancer Res Treat
2009; 116: 295-302.
20. Wittner BS, Sgroi DC, Ryan PD, et al . Analysis of the MammaPrint breast cancer assay in a predominantly
postmenopausal cohort. Clin Cancer Res 2008; 14: 2988-2993.
21. Masuda N, Ohnishi T, Kawamoto S, Monden M, Okubo K. Analysis of chemical modification of RNA from
formalin-fixed samples and optimization of molecular biology applications for such samples. Nucleic Acids
Res 1999; 27: 4436-4443.
22. Cronin M, Pho M, Dutta D, et al . Measurement of gene expression in archival paraffin-embedded tissues:
development and performance of a 92-gene reverse transcriptase-polymerase chain reaction assay.
Am J Pathol 2004; 164: 35-42.
23. Vonsattel JP, Aizawa H, Ge P, et al . An improved approach to prepare human brains for research. J
Neuropathol Exp Neurol 1995; 54: 42-56.
24. Bueno de Mesquita JM, Van Harten WH, Retel VP, et al . Use of 70-gene signature to predict prognosis of
patients with node-negative breast cancer: a prospective community-based feasibility study (RASTER).
Lancet Oncol 2007; 8: 1079-1087.
25. Bogaerts J, Cardoso F, Buyse M, et al . Gene signature evaluation as a prognostic tool: challenges in the
design of the MINDACT trial. Nat Clin Pract Oncol 2006; 3: 540-551.
26. Mook S, Van’t Veer LJ, Rutgers EJ, Piccart-Gebhart MJ, Cardoso F. Individualization of therapy using
Mammaprint: from development to the MINDACT Trial. Cancer Genomics Proteomics 2007; 4: 147-155.
27. Cardoso F, Van’t Veer L, Rutgers E, et al . Clinical application of the 70-gene profile: the MINDACT trial. J
Clin Oncol 2008; 26: 729-735.
28. Glas AM, Floore A, Delahaye LJ, et al . Converting a breast cancer microarray signature into a high-
throughput diagnostic test. BMC Genomics 2006; 7: 278-287.
29. Camp RL, Charette LA, Rimm DL. Validation of tissue microarray technology in breast carcinoma. Lab
Invest 2000; 80: 1943-1949.
30. Bammler T, Beyer RP, Bhattacharya S, et al . Standardizing global gene expression analysis between
laboratories and across platforms. Nat Methods 2005; 2: 351-356.
31. Dobbin KK, Beer DG, Meyerson M, et al . Interlaboratory comparability study of cancer gene expressionanalysis using oligonucleotide microarrays. Clin Cancer Res 2005; 11: 565-572.
32. Irizarry RA, Warren D, Spencer F, et al . Multiple-laboratory comparison of microarray platforms. Nat Methods
2005; 2: 345-350.
33. Florell SR, Coffin CM, Holden JA, et al . Preservation of RNA for functional genomic studies: a
multidisciplinary tumor bank protocol. Mod Pathol 2001; 14: 116-128.
34. Mutter GL, Zahrieh D, Liu C, et al . Comparison of frozen and RNALater solid tissue storage methods for
use in RNA expression microarrays. BMC Genomics 2004; 5: 88-94.
35. Leyland-Jones BR, Ambrosone CB, Bartlett J, et al . Recommendations for collection and handling of
specimens from group breast cancer clinical trials. J Clin Oncol 2008; 26: 5638-5644.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 50/248
Chapter 4
The 70-gene prognosis signature predicts
early metastasis in breast cancer patients
between 55 and 70 years of age
Stella Mook
Marjanka K. Schmidt
Britta Weigelt
Bas Kreike
Inge Eekhout
Marc J. Van de Vijver
Annuska M. Glas
Arno FlooreEmiel J.Th. Rutgers
Laura J. Van ’t Veer
Ann Oncol 2010; 21: 717-722.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 51/248
Chapter 4
58
Abstract
Background
The majority of breast cancer patients are postmenopausal women who are increasingly
being offered adjuvant chemotherapy. Since the beneficial effect of chemotherapy in
postmenopausal patients predominantly occurs in the first 5 years after diagnosis, a
prognostic marker for early events can be of use for adjuvant treatment decision-making.
The aim of this study was to evaluate the prognostic value of the 70-gene prognosis-
signature for early events in postmenopausal patients.
Methods
Frozen tumor samples from 148 patients aged 55-70 years were selected (T1-2, N0) and
classified by the 70-gene prognosis signature (MammaPrint™) into good or poor prognosis.
Eighteen percent received hormonal therapy.
Results
Breast cancer-specific survival (BCSS) at 5 years was 99% for the good-prognosis signature
versus 80% for the poor-prognosis signature group ( p = 0.036). The 70-gene prognosis
signature was a significant and independent predictor of BCCS during the first 5 years offollow-up with an adjusted hazard ratio of 14.4 (95% confidence interval 1.7-122.2; p = 0.01)
at 5 years.
Conclusion
The 70-gene prognosis signature can accurately select postmenopausal patients at low
risk of breast cancer-related death within 5 years of diagnosis and can be of clinical use in
selecting postmenopausal women for adjuvant chemotherapy.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 52/248
The 70-gene signature in postmenopausal patients
59
4
Introduction
Approximately two-thirds of the newly diagnosed breast cancer patients are ≥ 55
years of age.1 These postmenopausal women are increasingly being offered adjuvant
chemotherapy despite the more favorable biological characteristics of their tumors and
their known favorable breast cancer-specific outcome in general.2-5 The Early Breast Cancer
Trialists’ Collaborative Group meta-analysis has shown that the benefit from chemotherapy
is influenced by age, with less benefit in older patients. Moreover, those data have shown
that the time course of chemotherapy efficacy differs between pre- and postmenopausal
patients; the benefit of chemotherapy in postmenopausal breast cancer patients occurs
predominantly in the first 5 years, while in premenopausal patients, the benefit sustains
throughout the first 10 years.6 Therefore, a prognostic marker that can accurately identify
postmenopausal patients who are at low risk of developing an early breast cancer-
related event can be of clinical use for selecting postmenopausal patients for adjuvant
chemotherapy. One of the prognostic markers in the field of breast cancer is the 70-gene
prognosis signature (MammaPrint™), which can accurately identify patients who have a
good prognosis and therefore might be safely spared chemotherapy.7-11 This signature has
been developed in a predefined subset of patients, i.e. women under the age of 55 years at
diagnosis with stage I or II, node-negative breast cancer. Therefore, the aim of our study was
to evaluate the prognostic value of the 70-gene prognosis signature in postmenopausal
women with node-negative breast cancer. Specifically, we investigated whether the
signature could select postmenopausal patients who are at low risk of developing anearly breast cancer-related event and thus can be safely spared chemotherapy, without
jeopardizing disease outcome.
Methods
Patient selection
A consecutive series of patients treated at the Netherlands Cancer Institute-Antoni vanLeeuwenhoek Hospital (NKI-AVL) from 1984 to 1996 were selected according to the
following criteria: female, unilateral T1 or T2 primary invasive breast carcinoma, negative
nodal status, aged between 55 and 71 years at diagnosis, no adjuvant chemotherapy and
fresh frozen tumor material available in the comprehensive NKI-AVL tissue bank. Patients
without complete axillary staging, patients with prior malignancies (except for non-
melanoma skin cancer and dysplasia of the cervix), bilateral synchronous breast tumors or
patients treated with neoadjuvant therapy were not included.
All patients (n = 148) had been treated by modified radical mastectomy or breast
-conserving surgery, including axillary lymph node dissection, followed by radiotherapy

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 53/248
Chapter 4
60
if indicated. Twenty-seven patients (18%) received endocrine therapy, which consisted of
tamoxifen for a median duration of 2.0 years (range 0.06-7.0 years). Patients were treated
according to consensus guidelines, taking into account patients’ will and consent. The
study was approved by the ethical review board of the NKI-AVL.
Tumor samples, RNA extraction and gene expression analysis
Frozen tumor samples were evaluated for MammaPrint™ (FDA 510(K) cleared) at Agendia’s
laboratories (ISO17025 certified and CLIA accredited; Amsterdam, the Netherlands)
blinded to clinical data, as previously described.7,12 Briefly, frozen sections were stained with
hematoxylin and eosin; only samples that contained at least 30% tumor cells were used
for RNA isolation. Labeled complementary RNAs were hybridized together with a standard
breast cancer reference pool to the custom-designed MammaPrint™ microarray. 12 Tumors
were classified according to their cosine correlation coefficient with the MammaPrint™
template. Tumors with a correlation coefficient above the threshold were classified as
good prognosis signature, whereas all other tumors were classified as poor prognosis
signature.7,12
Clinicopathological and follow-up data
Clinical data were retrieved from medical patient records, blinded to the 70-gene prognosis
signature. Follow-up was completed until October 2007. End points considered were timefrom surgery to distant metastasis as first event [distant metastasis-free survival (DMFS)]
and breast cancer-specific survival (BCSS), defined as the time from surgery to breast cancer-
related death. For the analysis of DMFS, we considered distant metastasis as first event as
failure; patients were censored on the date of local or regional recurrence, development
of a second primary, including contralateral breast cancer, death from any cause or date
of last follow-up visit. Tumor grade was defined according to Bloom-Richardson. Estrogen
receptor (ER) expression was estimated using ER messenger RNA levels as determined by
the microarray.8
Clinical risk was evaluated using Adjuvant! software version 8.0 (available at www.adjuvantonline.com). Adjuvant! calculates 10-year survival probability based on patient’s
age, co-morbidities (set to ‘average for age’), tumor size, tumor grade, ER-status and
number of positive axillary lymph nodes.13,14 Patients were classified as having low clinical
risk when the predicted 10-year BCSS was > 88% for ER-positive tumors and > 92% for ER-
negative tumors, respectively.9

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 54/248
The 70-gene signature in postmenopausal patients
61
4
Statistical analyses
Analyses were carried out using SPSS version 15.0 (SPSS Inc., Chicago, IL). Cox proportional
hazards regression analyses were used to calculate hazard ratios (HRs) and their 95%
confidence intervals (CIs). HRs for the risk groups as defined by the 70-gene signature were
estimated with stratification for clinical risk as defined by Adjuvant! (adjusted HRs).
Additionally, HRs for the risk groups as defined by Adjuvant! were estimated with
stratification for genomic risk as defined by the 70-gene prognosis signature. The impact
of duration of follow-up on HRs was analyzed by censoring observations at increasing time
points.
Results
The 70-gene prognosis signature (MammaPrint™) risk classification was assessed in tumor
tissues of a consecutive series of 148 postmenopausal patients with early-stage, lymph
node-negative, invasive breast cancer. Tumor samples of 173 patients fulfilled the selection
criteria, of which 25 contained insufficient tumor cells (n = 22) or had insufficient RNA
quality (n = 3). All 148 samples eligible for genomic profiling were successfully hybridized.
There was no difference in tumor or patient characteristics between the 25 samples that
could not be hybridized and the 148 analyzed samples with regard to age, tumor size,
histology, overall survival and BCSS (data not shown). The median duration of follow-upwas 12.5 years (range 0.4-20.2) for the 114 patients who did not die of breast cancer and
7.2 years (range 0.8-17.7) for the 34 patients who died of breast cancer. During follow-up,
83 patients had at least one event, among which were 42 distant metastases including 36
distant metastases as first event and 57 deaths of which 34 were breast cancer-related.
Twelve of the 34 breast cancer-related deaths occurred within 5 years after diagnosis.
Classification by 70-gene prognosis signature and disease outcome
The 70-gene prognosis signature classified 91 (61%) patients as good prognosis, whereas57 (39%) patients were classified as poor prognosis. A good prognosis signature was
associated with smaller, well-differentiated and ER -positive tumors (Table 1).
Patients classified as good prognosis by the signature had a 5-year DMFS probability of
93% [standard error (SE) 3%], compared with 72% (SE 6%) in the poor-prognosis signature
group (Figure 1A). DMFS at 5 years was significantly worse in the poor-prognosis signature
group, with a univariate HR of 4.6 (95%CI 1.8-12.0; p = 0.001). Over the entire follow-up
period, the HR for DMFS was 1.8 (95% CI 0.9-3.5; p = 0.07).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 55/248
Chapter 4
62
Table 1. Baseline characteristics and association between clinicopathological characteristics
and the 70-gene prognosis profile
70-gene prognosis signature
Good prognosis
signature (n=91)
Poor prognosis
signature (n=57)
P value
Characteristics No. % No. %
Age (years) 0.25
< 60 26 28.6 24 42.1
60 - 64 34 37.4 15 26.3
65 - 71 31 34.1 18 31.6
Surgery 0.32
Breast conserving surgery 46 50.5 24 42.1
Mastectomy 45 49.5 33 57.9
Tumor size 0.007
pT1 (≤ 20 mm) 59 64.8 24 42.1
pT2 (> 20-50 mm) 32 35.2 33 57.9
Histological tumor type 0.02
Invasive ductal carcinoma 67 73.6 52 91.2
Invasive lobular carcinoma 17 18.7 0 0
Mixed IDC ILC 4 4.4 3 5.3
Other 3 3.3 2 3.5
Histological grade < 0.001
Grade I 52 57.1 3 5.3
Grade II 28 30.8 15 26.3
Grade III 11 12.1 39 68.4
Estrogen-receptor status < 0.001
Negative 3 3.3 29 50.9
Positive 88 96.7 28 49.1
Adjuvant endocrine therapy 0.86
No 74 81.3 47 82.5
Yes 17 18.7 10 17.5
IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma.
The 5-year BCSS probability was 99% (SE 1%) for the good-prognosis signature group and
80% (SE 5%) for the poor-prognosis signature group (Figure 1B). In addition, the difference
in BCSS between the poor–prognosis signature group and the good-prognosis signature
group over the entire follow-up period was significant with a univariate HR of 2.0 (95% CI
1.0-4.0; p = 0.04). This difference was most pronounced at 5 years, with a univariate HR of
19.1 (95%CI 2.5-148; p = 0.005) (Figure 2A).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 56/248
The 70-gene signature in postmenopausal patients
63
4
Figure 1.
Kaplan-Meier curves by 70-gene prognosis signature.
A. Time to distant metastases as first event.
B. Breast cancer-specific survival
Time (years)
121086420
D i s t a n t m e t a s t a s i s - f r e e s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
91
57
86
2344 37 34 31
77 67 51 43 28
17 Poor signature
Good signature
Log rank p = 0.07
72 ± 6%
93 ± 3%
80 ± 5%
67 ± 7%
Time (years)
121086420
B r e a s t c a n c e r - s p e c i fi c s
u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
91
57
89
2852 46 42 36
86 80 68 61 48
23 Poor signature
Good signature
80 ± 5%
69 ± 6%
99 ± 1%
90 ± 4%
Log rank p = 0.036
A
B

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 57/248
Chapter 4
64
Clinical risk assessment and discordance with 70-gene prognosis signature
Using the predefined cut-off, Adjuvant! classified 74 patients (50%) as clinical low risk and
74 patients (50%) as clinical high risk. Concordance was observed between Adjuvant! and
the 70-gene prognosis signature for 62 (42%) low-risk/good prognosis patients, whereas
45 patients (30%) were classified as high-risk/poor prognosis according to both risk
assessments. The clinical risk assessment was discordant with the genomic prognosis for
41 patients (28%); 12 (8%) were classified as clinical low risk and poor prognosis signature
and 29 (20%) were classified as clinical high risk though good prognosis signature.
Prediction of early breast cancer-specific death: time dependency
Since the benefit of chemotherapy in postmenopausal patients is predominantly seen in
the first 5 years and given the long follow-up time in this study compared with the original
validation study (11.6 versus 6.7 years, respectively), we calculated unadjusted HRs for the
signature and clinical risk assessment with censoring of all observations at increasing time
points (Figure 2, panels A and B). Remarkably, the 70-gene prognosis signature was a strong
predictor for early breast cancer-specific death (BCSD) with the strongest prognostic
value at 5 years as shown by the highest HR (HR 19.1; 95% CI 2.5-148; p = 0.005), whereas
the clinical risk classification predicted disease outcome more evenly with a tendency to
predict better after 5 years, with the strongest prognostic capacity at 10 years (HR 6.2;
95% CI 2.1-18.0; p = 0.001). To further evaluate the clinical utility of the 70-gene prognosissignature, we adjusted its performance for the clinical risk assessment, which showed that
the signature is a powerful predictor of early BCSD independent of the clinical risk, with an
adjusted HR at 5 years of 14.4 (95% CI 1.7-122; p = 0.01) (Figure 2, panel C ). The reverse analysis,
i.e. HRs for the clinical risk classification adjusted for the gene signature, showed that the
clinical risk classification is a prognostic factor of BCSD after 10 years independent of the
signature, with an adjusted HR of 4.4 (95% CI 1.4-13.6; p = 0.01) for BCSS at 10 years (Figure
2, panel D).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 58/248
The 70-gene signature in postmenopausal patients
65
4
6,6
13,5 15,4 19,112,4
3,92,6
2,0 2,0
0,1
1,0
10,0
100,0
2 3 4 5 7 10 12,5 15 None
A. 70-gene prognosis-signature
4,1
8,3
4,2 5,3 4,8
6,24,6 4,3 3,6
0,1
1,0
10,0
100,0
B. Adjuvant! online
2,0
3,5
1,6 1,9 2,0
4,4 3,8 4,13,2
0,1
1,0
10,0
100,0
D. Adjuvant! adjusted for signature
4,98,4
12,6 14,49,4
2,21,6 1,2 1,3
0,1
1,0
10,0
100,0
C. Signature adjusted for Adjuvant!
15% 26% 29% 35%
47%
74%85%
94% 100%
2 3 4 5 7 10 12,5 15 None
Cumulativeproportion
of events
Censoring time (years)
Figure 2.
Hazard ratios (HRs) for breast cancer-specific death at increasing censoring times.
A). Univariate HRs for poor-prognosis signature versus good-prognosis signature groups.
B). Univariate HRs for clinical high-risk versus clinical low-risk groups as calculated by Adjuvant!.
C). HRs for 70-gene prognosis signature adjusted for clinical risk. D). HRs clinical risk assessment
by Adjuvant! adjusted for prognosis signature.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 59/248
Chapter 4
66
Discussion
The present validation study shows that the 70-gene prognosis signature, which was
developed in premenopausal patients with early -stage breast cancer, is also a prognostic
factor in postmenopausal women, with especially strong prognostic capacity in the first
5 years after diagnosis. Since the beneficial effect of chemotherapy in postmenopausal
women mainly occurs in the first 5 years after diagnosis,6,15 accurate identification of
early events by the 70-gene prognosis signature can be of great value in selecting
postmenopausal patients for adjuvant chemotherapy.
In a previous validation study, Buyse et al .9 showed a strong time dependency of the signature.
Since we were especially interested in predicting early events which might be prevented by
chemotherapy, we also investigated the effect of duration of follow-up on the prognostic
value of the signature. The prognostic value of the signature was most pronounced within
the first 5 years of diagnosis, even after adjustment for clinicopathological risk classification
by Adjuvant! (Figure 2, panel C ). These results demonstrate the additional value of the 70-gene
prognosis signature over and above the clinical risk assessment in predicting early BCSD.
First, the signature enlarged the group of low-risk/ good prognosis patients as compared
with the clinical risk classification (from 50% to 61%). Secondly, despite this increase in
the low -risk group, the signature accurately classified 11 of 12 (92%) patients who died of
breast cancer within 5 years of diagnosis as poor prognosis (Figure 3), compared with 10 of 12
(83%) correctly classified by Adjuvant!.
Although our study confirmed that the signature can correctly predict early BCSD, lateBCSD was less accurately predicted by the signature (Figure 3), resulting in misclassification
of 15 BCSD after 5 years of diagnosis (compared with seven misclassified by Adjuvant!).
Remarkably, all 15 patients who were classified as good signature but died of breast cancer
after 5 years had ER-positive tumors, and only one patient received endocrine therapy.
Consequently, endocrine treatment could potentially have prevented at least part of these
late BCSDs (31% reduction of annual breast cancer death rate by adjuvant tamoxifen). 6
In our series, the 27 patients who received hormonal therapy were equally distributed
between the good- and the poor-prognosis signature groups. Moreover, the median
duration of hormonal therapy was only 2 years (according to Dutch treatment guidelinesin the years of diagnosis concerned), instead of the current standard treatment of at least
5 years. Separate analyses of the 121 hormonal therapy-naive patients showed that the
70-gene prognosis signature was also a predictor for early BCSD in untreated patients
between 55 and 71 years of age (adjusted HR at 5 years 10.8; 95% CI 1.2-94.7; p = 0.03).
The strong time dependency of the signature can be explained by the fact that the
signature was built to identify patients with distant metastases within 5 years. Moreover,
it supports the hypothesis that different biological mechanisms are involved in early and
late disease recurrences.16,17 ER-negative, high-grade tumors are more likely to metastasize
during the early years after diagnosis, whereas ER-positive, low-grade tumors more often
cause late recurrences.18

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 60/248
The 70-gene signature in postmenopausal patients
67
4
Figure 3.
Breast cancer-specific deaths by 70-gene prognosis signature. Each circle represents a patient
who died of breast cancer.
In our study, 61% of the patients were classified as good prognosis by the signature. In
previous validation studies, the 70-gene signature consistently classified ~40% to 50% of
the (predominantly premenopausal) patients as good prognosis.8-11 The increase in patients
classified as good prognosis in our series could be the reflection of the intrinsic low-risk
nature of breast cancer and mammographic screening in postmenopausal women.2-4
Recently, an independent validation study of the 70-gene prognosis signature in
predominantly postmenopausal women was published.19
In contrast to our study, themajority of their study population was classified as high risk (73% versus 39% in our series). This
discrepancy in risk classification can be attributed to differences in baseline characteristics,
i.e. more poorly differentiated tumors in their series. On the other hand, disease outcome
in our series is worse compared with the outcome in the series of Wittner et al .,19 which
can be caused by the difference in proportion of patients who received adjuvant systemic
therapy (18% hormonal therapy in our series versus 45% chemo- and/or hormonal therapy
in Wittner’s series).
Several other prognostic profiles have been studied, among which are the 76-gene profile
and the 21-recurrence score.20,21 Both profiles have been developed and so far validated in
0 5 10 15
Breast cancer-specific deaths
Poor signature
Good signature
Time (years)

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 61/248
Chapter 4
68
a mixed population of pre- and postmenopausal women.22,23 To our knowledge, this is the
first study that evaluates the prognostic value of a prognostic signature in an exclusively
postmenopausal patient series. Recently, Anders et al . 5 showed a significant difference in
gene expression patterns between tumors from pre- and postmenopausal breast cancer
patients. However, our study indicates that disease outcome in pre- and postmenopausal
patients can be determined by common denominators, which are captured by the 70-gene
signature.
In conclusion, our study indicates that application of the 70-gene prognosis signature in
breast cancer patients between 55 and 71 years of age could result in a more accurate
allocation of adjuvant systemic therapy. A poor prognosis signature would imply
chemotherapy treatment to prevent early breast cancer deaths, and patients with ER-
positive tumors should receive endocrine therapy to prevent late events. Furthermore,
given the results from the ATAC (Arimidex, Tamoxifen, Alone or in Combination) and
(Breast International Group) BIG 1-98 trial indicating that aromatase inhibitors (AIs) are
more effective in preventing early recurrences compared with tamoxifen, patients with
ER-positive tumors classified as poor prognosis by the signature might be candidates for
up-front AI treatment.24-26 This last question will also be addressed in the endocrine therapy
randomization of the MINDACT (Microarray for Node Negative and 1 to 3 Positive Node
Disease may Avoid Chemotherapy) trial; patients with hormone receptor-positive tumors
(good and poor prognosis signature) will be randomized between 2 years of tamoxifen
followed by 5 years of letrozole versus 7 years of letrozole up front, therefore endocrine
responsiveness can be related to the 70-gene prognosis signature.27,28
Funding
European Commission Framework Program VI-TRANSBIG (LSHC-CT-2004-503426); Dutch
National Genomics Initiative-Cancer Genomics Center (CGC 2008-2012); Agendia BV.
Acknowledgements
We are indebted to Mahasti Saghatchian and Marleen Kok for helpful discussions andcritically reading the manuscript.
Disclosures
LJvV and MJvdV are named inventor on a MammaPrint™ patent. LJvV reports holding
equity in Agendia BV. AF and AMG are employees of Agendia BV.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 62/248
The 70-gene signature in postmenopausal patients
69
4
References
1. Ries LAG, Melbert D, Krapcho M et al. SEER Cancer Statistics Review, 1975-2005. Bethesda, MD: National
Cancer Institute 2008; http://seer.cancer.gov/csr/1975_2005/, based on November 2007 SEER data
submission, posted to the SEER web site. Last accessed 28 November, 2008.
2. Anderson WF, Chatterjee N, Ershler WB, Brawley OW. Estrogen receptor breast cancer phenotypes in
the Surveillance, Epidemiology, and End Results database. Breast Cancer Res Treat 2002; 76: 27-36.
3. Diab SG, Elledge RM, Clark GM. Tumor characteristics and clinical outcome of elderly women with
breast cancer. J Natl Cancer Inst 2000; 92: 550-556.
4. Fisher B, Wickerham DL, Brown A, Redmond CK. Breast cancer estrogen and progesterone receptor
values: their distribution, degree of concordance, and relation to number of positive axillary nodes. J
Clin Oncol 1983; 1: 349-358.
5. Anders C, Hsu D, Broadwater G, et al . Young age at diagnosis correlates with worse prognosis and defines
a subset of breast cancers with shared patterns of gene expression. J Clin Oncol 2008; 26: 3324-3330.
6. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for
early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet
2005; 365: 1687-1717.
7. Van ‘t Veer LJ, Dai H, Van de Vijver MJ, et al . Gene expression profiling predicts clinical outcome of breast
cancer. Nature 2002; 415: 530-536.
8. Van de Vijver MJ, He YD, Van ‘t Veer LJ, et al . A gene-expression signature as a predictor of survival in
breast cancer. N Engl J Med 2002; 347: 1999-2009.
9. Buyse M, Loi S, Van ‘t Veer L, et al . Validation and clinical utility of a 70-gene prognostic signature for
women with node-negative breast cancer. J Natl Cancer Inst 2006; 98: 1183-1192.
10. Mook S, Schmidt MK, Viale G, et al . The 70-gene prognosis-signature predicts disease outcome in breast
cancer patients with 1-3 positive lymph nodes in an independent validation study. Breast Cancer Res Treat
2009; 116: 295-302.
11. Bueno de Mesquita JM, Linn SC, Keijzer R et al. Validation of 70-gene prognosis signature in node-
negative breast cancer. Breast Cancer Res Treat 2009; 117: 483–495.
12. Glas AM, Floore A, Delahaye LJ, et al . Converting a breast cancer microarray signature into a high-
throughput diagnostic test. BMC Genomics 2006; 7: 278-287.
13. Ravdin PM, Siminoff LA, Davis GJ, et al . Computer program to assist in making decisions about adjuvanttherapy for women with early breast cancer. J Clin Oncol 2001; 19: 980-991.
14. Olivotto IA, Bajdik CD, Ravdin PM, et al . Population-based validation of the prognostic model ADJUVANT!
for early breast cancer. J Clin Oncol 2005; 23: 2716-2725.
15. Demicheli R, Miceli R, Moliterni A, et al . Breast cancer recurrence dynamics following adjuvant CMF is
consistent with tumor dormancy and mastectomy-driven acceleration of the metastatic process. Ann
Oncol 2005; 16: 1449-1457.
16. Klein CA, Blankenstein TJ, Schmidt-Kittler O, et al . Genetic heterogeneity of single disseminated tumour
cells in minimal residual cancer. Lancet 2002; 360: 683-689.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 63/248
Chapter 4
70
17. Schmidt-Kittler O, Ragg T, Daskalakis A, et al . From latent disseminated cells to overt metastasis: genetic
analysis of systemic breast cancer progression. Proc Natl Acad Sci USA 2003; 100: 7737-7742.
18. Saphner T, Tormey DC, Gray R. Annual hazard rates of recurrence for breast cancer after primary
therapy. J Clin Oncol 1996; 14: 2738-2746.
19. Wittner BS, Sgroi DC, Ryan PD, et al . Analysis of the MammaPrint breast cancer assay in a predominantly
postmenopausal cohort. Clin Cancer Res 2008; 14: 2988-2993.
20. Paik S, Shak S, Tang G, et al . A multigene assay to predict recurrence of tamoxifen-treated, node-negative
breast cancer. N Engl J Med 2004; 351: 2817-2826.
21. Wang Y, Klijn JG, Zhang Y, et al . Gene-expression profiles to predict distant metastasis of lymph-node-
negative primary breast cancer. Lancet 2005; 365: 671-679.
22. Esteva FJ, Sahin AA, Cristofanilli M, et al . Prognostic role of a multigene reverse transcriptase-PCR assay
in patients with node-negative breast cancer not receiving adjuvant systemic therapy. Clin Cancer Res
2005; 11: 3315-3319.
23. Foekens JA, Atkins D, Zhang Y, et al . Multicenter validation of a gene expression-based prognostic
signature in lymph node-negative primary breast cancer. J Clin Oncol 2006; 24: 1665-1671.
24. Coates AS, Keshaviah A, Thurlimann B, et al . Five years of letrozole compared with tamoxifen as initial
adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update
of study BIG 1-98. J Clin Oncol 2007; 25: 486-492.
25. Mauriac L, Keshaviah A, Debled M, et al . Predictors of early relapse in postmenopausal women with
hormone receptor-positive breast cancer in the BIG 1-98 trial. Ann Oncol 2007; 18: 859-867.
26. Forbes JF, Cuzick J, Buzdar A, et al . Effect of anastrozole and tamoxifen as adjuvant treatment for early-
stage breast cancer: 100-month analysis of the ATAC trial. Lancet Oncol 2008; 9: 45-53.
27. Bogaerts J, Cardoso F, Buyse M, et al . Gene signature evaluation as a prognostic tool: challenges in the
design of the MINDACT trial. Nat Clin Pract Oncol 2006; 3: 540-551.
28. Mook S, Van’t Veer LJ, Rutgers EJ, Piccart-Gebhart MJ, Cardoso F. Individualization of therapy using
Mammaprint: from development to the MINDACT Trial. Cancer Genomics Proteomics 2007; 4: 147-155.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 64/248
Chapter 5
The 70-gene prognosis-signature predicts
disease outcome in breast cancer patients
with 1-3 positive lymph nodes in an
independent validation study
Stella Mook
Marjanka K. Schmidt
Giuseppe Viale
Giancarlo Pruneri
Inge Eekhout
Arno Floore
Annuska M. Glas
Jan BogaertsFatima Cardoso
Martine Piccart-Gebhart
Emiel J.Th. Rutgers
Laura J. Van ’t Veer
On behalf of the TRANSBIG consortium
Breast Cancer Res Treat 2009; 116: 295-302

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 65/248
Chapter 5
74
Abstract
Purpose
The 70-gene prognosis signature has shown to be a valid prognostic tool in node-negative
breast cancer. Although axillary lymph node status is considered to be one of the most
important prognostic factors, still 25–30% of node-positive breast cancer patients will
remain free of distant metastases, even without adjuvant systemic therapy. We therefore
investigated whether the 70-gene prognosis signature can accurately identify patients
with 1-3 positive lymph nodes who have an excellent disease outcome.
Methods
Frozen tumor samples from 241 patients with operable T1-3 breast cancer, and 1-3 positive
axillary lymph nodes, with a median follow-up of 7.8 years, were selected from 2 institutes.
Using a customized microarray, tumor samples were analyzed for the 70-gene tumor
expression signature. In addition, we reanalyzed part of a previously described cohort (n =
106) with extended follow-up.
Results
The 10-year distant metastasis-free (DMFS) and breast cancer specific survival (BCSS)probabilities were 91% (SE 4%) and 96% (SE 2%), respectively for the good prognosis
signature group (99 patients), and 76% (SE 4%) and 76% (SE 4%), respectively for the poor
prognosis signature group (142 patients). The 70-gene signature was significantly superior
to the traditional prognostic factors in predicting BCSS with a multivariate hazard ratio (HR)
of 7.17 (95% CI 1.81 to 28.43; p = 0.005).
Conclusions
The 70-gene prognosis signature outperforms traditional prognostic factors in predictingdisease outcome in patients with 1-3 positive nodes. Moreover, the signature can accurately
identify patients with an excellent disease outcome in node-positive breast cancer, who
may be safely spared adjuvant chemotherapy.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 66/248
The 70-gene signature in pN1 breast cancer
75
5
Introduction
Axillary lymph node status is historically one of the most important prognostic factors
in breast cancer, with deterioration in disease outcome as the number of positive nodes
increases.1-3 Consequently, patients with axillary lymph node metastases are considered as
having a poor prognosis and hence are most likely to benefit from adjuvant chemotherapy,
with an absolute benefit of 6-15% at 5 years.4 However, up to 25-30% of node-positive
patients will remain free of distant metastases even without adjuvant systemic therapy.4,5
Thus, adjuvant treatment decision-making based on nodal status is only moderately
accurate and results in overtreatment, with unnecessary exposure to treatment toxicity.
Identifying robust and reliable prognostic factors that can select those node-positive
patients who do not require adjuvant chemotherapy is essential to reduce overtreatment.
One of the new prognostic markers which has been validated for lymph node-negative
breast cancer is the 70-gene prognosis signature (MammaPrint™).6-8 The original
retrospective validation study demonstrated that the signature was also a significant
prognostic factor in 144 node-positive patients.8 The aim of this study is to further
substantiate the prognostic value of the 70-gene signature in patients with 1-3 positive
nodes in a new independent dataset, and to assess its relation to standard prognostic
markers. Specifically, we investigated whether the 70-gene signature can select patients
with 1-3 positive nodes with an excellent survival, who might be safely spared adjuvant
chemotherapy.
Methods
Patients
Patients were selected from the Netherlands Cancer Institute-Antoni van Leeuwenhoek
hospital (NKI-AVL), Amsterdam, The Netherlands (n = 213, consecutive series) and the
European Institute of Oncology (EIO), Milan, Italy (n = 79, consecutive series), according
to the following criteria: unilateral T1, T2 or operable T3 invasive breast carcinoma, withmetastases in 1-3 axillary lymph nodes; frozen tumor tissue available; no prior malignancies,
no bilateral synchronous breast tumors, and no neoadjuvant therapy. Micrometastases
(tumor deposits > 0.2 and ≤ 2.0 mm) were considered as positive lymph nodes. Patients
were diagnosed between 1994 and 2001 and were under the age of 71 years at diagnosis.
Patients were treated with mastectomy or breast-conserving surgery, including dissection
of the axillary lymph nodes (ALND), followed by radiotherapy and adjuvant systemic
therapy if indicated. Adjuvant systemic therapy was administered according to national
guidelines, taking into account patients’ preferences and consent (Table 1). The proportion
of adjuvant systemic therapy in our study was similar to all patients at NKI who fulfilled

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 67/248
Chapter 5
76
the above mentioned selection criteria except for the availability of frozen tumor tissue in
the same time period (data not shown). The study received approval of the medical ethical
committee of NKI-AVL.
To allow more extensive analyses, follow-up data of all patients with 1-3 positive nodes
from the previously described series by Van de Vijver,8 were updated, blinded to the 70-
gene prognosis signature.9
Tumor samples, RNA extraction and gene expression analysis
Frozen tumor samples were processed in Agendia’s laboratories (Amsterdam, the
Netherlands), for RNA isolation, amplification and labeling as previously described.7,10
Samples were available for RNA isolation if they contained at least 30% tumor cells on
hematoxylin/eosin stained sections. Of the 292 samples processed, 10 were rejected on
the basis of RNA quality and 41 because of insufficient tumor cells. The 51 rejected samples
were obtained from slightly smaller tumors than the 241 samples that were hybridized
(mean tumor size 19 mm versus 23 mm; p = 0.04). However, there were no differences in age,
tumor grade, ER status, systemic treatment and proportion alive after 10 years.
To assess the mRNA expression level of the 70 genes, RNA was hybridized to a custom-
designed array (MammaPrint™) blinded to clinical data, at Agendia’s ISO17025-certified and
CLIA accredited laboratories. Tumors were classified as 70-gene good or poor prognosis
signature as described previously.6-8,10
Clinicopathological data
Clinical data were retrieved from medical records, blinded to the 70-gene prognosis
signature. Endpoints considered were time from surgery to distant metastasis as first
event (DMFS), and breast cancer specific survival (BCSS), defined as time from surgery to
breast cancer-related death. For the analysis of distant metastasis-free survival (DMFS)
we considered distant metastases as first event as failure; patients were censored on date
of local or regional recurrence, development of second primary including contralateral
breast cancer, death from any cause or date of last follow-up visit. Tumor grading wasdefined according to the Bloom-Richardson method. Estrogen receptor (ER) status and
progesterone receptor (PR) status were determined by immunohistochemistry and
interpreted positive if more than 10% of the cells stained. For patients treated at NKI-AVL,
HER2/NEU immunohistochemistry status was retrieved from the original pathology report.
For patients treated at EIO, HER2/NEU status was determined by immunohistochemistry; in
case of 2+ scores FISH analyses were used to determine amplification (ratio ≥ 2.2).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 68/248
The 70-gene signature in pN1 breast cancer
77
5
Clinical risk assessment by Adjuvant!
To assess the 70-gene prognosis signature in a clinical context, it was compared with
the clinicopathological risk as predicted by Adjuvant! The Adjuvant! Software version 8.0
(available at www.adjuvantonline.com) calculated 10-year survival probability based on
patient’s age, co-morbidities, tumor size, tumor grade, ER-status and number of positive
axillary lymph nodes.11,12 Patients were considered as having low clinical risk when the 10-
year BCSS as predicted by Adjuvant! was more than 88% for ER-positive tumors, and more
than 92% for ER-negative tumors, respectively.6
Statistical analyses
Analyses were performed using SPSS version 15.0 (SPSS Inc, Chicago, IL) and EPICURE
(Epicure release 2.0.Seattle: HiroSoft International Corporation, 1996). Kaplan-Meier
survival plots and log-rank tests were used to assess the difference in DMFS and BCSS of the
predicted good and poor prognosis groups. Cox proportional hazards regression analyses
were used to calculate uni- and multivariate hazard ratios (HR) and their 95% confidence
intervals (95% CI). In multivariate Cox regression analyses traditional clinicopathological
variables were used. An interaction term of gene signature and chemotherapy, within a
multivariate Cox regression model was tested for significance by the likelihood ratio test.
P -values are two-sided.
Results
The 70-gene prognosis signature (MammaPrint™) was assessed in tumor tissue of an
independent series of 241 invasive breast cancer patients with 1-3 positive lymph nodes.
Among the 241 patients, 99 (41%) were classified as good prognosis signature, whereas 142
(59%) patients were classified as poor prognosis signature. Patients with a poor prognosis
signature were more frequently diagnosed at EIO, and had more often received adjuvant
chemotherapy and less often received endocrine therapy. Moreover, tumors classified aspoor prognosis signature were larger and more often poorly differentiated, ER- and PR
negative, and HER2/NEU receptor positive (Table 1).
After a median follow-up of 7.8 years (range, 0.01-12.3) 66 patients had at least one event,
including 13 local recurrences, 9 regional recurrences, 6 contralateral breast cancers, 9
second primary cancers, 43 distant metastases, including 35 distant metastases as first
event, and 39 deaths of which 33 breast cancer-related deaths.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 69/248
Chapter 5
78
T
a b l e 1 .
A s s o c i a t i o n b e t w e e n c l i n
i c o p a t h o l o g i c a l c h a r a c t e r i s t i c s a
n d t h e 7 0 - g e n e p r o g n o s i s s i g n a
t u r e f o r t h e n e w v a l i d a t i o n s e r i e s ( n =
2 4 1 ) .
7 0 - g e n e p r o g n o s i s s i g n a t u r e
G o o d p r o g n o s i s s i g n
a t u r e ( n = 9 9 )
P o o r p r o g n o
s i s s i g n a t u r e ( n = 1 4 2 )
P
v a l u e *
C h a r a c t e r i s t i c s
N o .
%
N o .
%
H o s p i t a l
< 0
. 0 0 1
N K I - A V L
8 4
8 4
. 8
9 0
6 3
. 4
E I O
1 5
1 5
. 2
5 2
3 6
. 6
A g e ( y e a r s )
0 . 1
8
< 4 0
6
6 . 1
1 7
1 2
. 0
4 0 -
4 9
4 1
4 1
. 4
6 1
4 3
. 0
5 0 -
5 9
3 9
3 9
. 4
4 7
3 3
. 0
6 0 -
7 0
1 3
1 3
. 1
1 7
1 2
. 0
S u r g e r y
0 . 1
7
B C T
5 4
5 4
. 5
9 0
6 3
. 4
M a s t e c t o m y
4 5
4 5
. 5
5 2
3 6
. 6
A x i l l a r y p r o c e d u r e
0 . 4
2
A L N D
6 2
6 2
. 6
9 6
6 7
. 6
S L N P & A L N D
3 7
3 7
. 4
4 6
3 2
. 4
N o d a l s t a t u s
0 . 9
3
1 p o s i t i v e n o d e
4 9
4 9
. 5
7 4
5 2
. 1
2 p o s i t i v e n o d e s
3 5
3 5
. 4
4 2
2 9
. 6
3 p o s i t i v e n o d e s
1 5
1 5
. 1
2 6
1 8
. 3
T u m o r s i z e ( p T N M )
0 . 0
1
p T 1 ( ≤ 2 0 m m )
5 8
5 8
. 6
5 9
4 1
. 5
p T 2 ( > 2 0 - 5
0 m m )
4 0
4 0
. 4
8 1
5 7
. 1
p T 3 ( > 5 0 m m )
1
1 . 0
2
1 . 4
H i s t o l o g i c a l t u m o r t y p e
< 0
. 0 0 1
D u c t a l
7 2
7 2
. 8
1 3 2
9 3
. 0
L o b u l a r
1 2
1 2
. 1
3
2 . 1
M i x e d
1 4
1 4
. 1
3
2 . 1
O t h e r
1
1 . 0
4
2 . 8
H i s t o l o g i c a l g r a d e
< 0
. 0 0 1
G o o d
4 5
4 6
. 4
1 2
8 . 5
M o d e r a t e
4 6
4 7
. 4
5 3
3 7
. 3
P o o r
6
6 . 2
7 7
5 4
. 2
U n k n o w n
2
0

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 70/248
The 70-gene signature in pN1 breast cancer
79
5
7 0 - g e n e p r o g n o s i s s i g n a t u r e
G o o d p r o g n o s i s s i g n
a t u r e ( n = 9 9 )
P o o r p r o g n o s i s s i g n a t u r e ( n = 1 4 2 )
P
v a l u e *
C h a r a c t e r i s t i c s
N o .
%
N o .
%
E s t r o g e n - r e c e p t o r s t a t u s
< 0
. 0 0 1
N e g a t i v e
4
4 . 0
4 6
3 2
. 4
P o s i t i v e
9 5
9 6
. 0
9 6
6 7
. 6
P r o g e s t e r o n e - r e c e p t o r s t a t u s
< 0
. 0 0 1
N e g a t i v e
1 6
1 6
. 5
7 2
5 0
. 7
P o s i t i v e
8 1
8 3
. 5
7 0
4 9
. 3
U n k n o w n
2
0
H E R 2 / N E U r e c e p t o r s t a t u s
< 0
. 0 0 1
N e g a t i v e
9 5
9 7
. 9
1 0 3
7 4
. 6
P o s i t i v e
2
2 . 1
3 5
2 5
. 4
U n k n o w n
2
4
A d j u v a n t s y s t e m i c t r e a t m e n t
0 . 4
1
N o n e
7
7 . 3
3
2 . 3
C h e m o t h e r a p y o n l y
1 0
1 0
. 4
4 3
3 2
. 3
E n d o c r i n e t h e r a p y o n l y
5 0
5 2
. 1
4 1
3 0
. 8
B o t h
2 9
3 0
. 2
4 6
3 4
. 6
U n k n o w n
3
9
A d j u v a n t c h e m o t h e r a p y
< 0
. 0 0 1
N o
5 7
5 9
. 4
4 4
3 3
. 1
Y e s
3 9
4 0
. 6
8 9
6 6
. 9
U n k n o w n
3
9
A d j u v a n t e n d o c r i n e t h e r a p y
0 . 0
0 5
N o
1 7
1 7
. 7
4 6
3 4
. 6
Y e s
7 9
8 2
. 3
8 7
6 5
. 4
U n k n o w n
3
9
A
b b r e v i a t i o n s : N K I - A V L
, N e t h e r l a n d s
C a n c e r I n s t i t u t e - A n t o n i v a n L e e u w e n h o e k h o s p i t a l ; E I O
, E u r o p e a n I n s t i t u
t e o f O n c o l o g y ; B C T
, b r e a s t - c o n s e r v
i n g t h e r a p y ;
A
L N D
, a x i l l a r y l y m p h n o d e d i s s e c t i o n
; S L N P
, s e n t i n e l l y m p h n o d e p r o c e d u
r e .
*
M i s s i n g v a l u e s w e r e n o t u s e d f o r c a l c u l a t i o n o f p
– v a l u e s .

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 71/248
Chapter 5
80
Figure 1. Kaplan-Meier curves by 70-gene prognosis signature among the 241 patients.
A) Breast cancer specific survival.
B) Distant metastasis-free survival (distant metastasis as first event).
Time (years)
1086420
B r e a s t c a n c e r - s p e c i fi c s u r v i v a
l
1.0
0.8
0.6
0.4
0.2
0.0
99
142
96
10137 127 105 58
95 83 53 15
Poor prognosis-signature
Good prognosis-signatureNumbers at
risk
99%
96%
Log-rank p < 0.001
88%
76%
Time (years)
1086420
D i s t a n t m e t a s t a s e s - f r e e s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
99
142
96
8119 105 84 47
93 77 49 12
Poor prognosis-signature
Good prognosis-signatureNumbers at
risk
Log-rank p = 0.001
98%
80%
76%
91%
A
B

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 72/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 73/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 74/248
The 70-gene signature in pN1 breast cancer
83
5
factor with an HR of 0.31 (95% CI 0.12-0.80; p = 0.02); the 70-gene signature and number of
positive nodes (3 versus 1) tended to be prognostic factors with HRs of 2.99 (95% CI 0.996-
8.99; p = 0.051) and 2.29 (95% CI 0.99-5.29; p = 0.053), respectively.
Adjuvant! classified 32 patients (13%) as clinical low risk and 209 patients (87%) as clinical
high risk, using the pre-defined cut-off (See methods). The clinical risk assessment was
discordant with the genomic risk by the 70-gene prognosis signature for 77 patients (32%);
5 were classified as clinical low risk and poor prognosis signature; 72 were classified as
clinical high risk and good prognosis signature. Remarkably, in the 27 patients defined as
both 70-gene good prognosis and clinical low risk none of the patients developed distant
metastases nor died (Figure 2). Moreover, when the clinical high risk group (n = 209) was
stratified by signature risk, the 10-year BCSS probability was 94% (SE 3%) for the good
prognosis signature group and 76% (SE 4%) for the poor prognosis signature group,
respectively [HR of 4.12 (95% CI 1.45-11.76; p = 0.008)]. This shows the additional value of
the 70-gene prognosis signature up to and above the Adjuvant! risk assessment.
Interestingly, the 70-gene signature was also predictive for BCSS in the 101 chemotherapy
naïve patients (HR 7.33; 95% CI 1.61-33.49; p = 0.01), 128 chemotherapy-treated patients (HR
4.70; 95% CI 1.09-20.17; p = 0.04) ( Supplementary Figure 3), 63 endocrine therapy naïve patients
(HR ∞ (infinity); 95% CI 2.97-∞; p = 0.001), and 166 endocrine therapy-treated patients (HR
3.63; 95% CI 1.21-10.94; p = 0.02). Moreover, the 70-gene signature accurately predicted
BCSS in the 191 patients with ER-positive tumors (HR 9.75; 95% CI 2.26-42.01; p = 0.002). The
group of 50 ER-negative patients of whom 4 were classified as good prognosis signature,
and the 10 adjuvant untreated patients, were too small to analyze separately.Among the 241 patients, 29 had solely micrometastatic axillary lymph node involvement
(22 patients in 1 node, 6 in 2 nodes, and 1 in 3 nodes, respectively) and 18 patients had
micrometastatic involvement in addition to macrometastases. The 70-gene signature
maintained its prognostic value when nodes with micrometastases were excluded
(multivariate HR for BCSS 6.68; 95% CI 1.65-27.08; p = 0.008).
The previously described validation of the 70-gene signature by Van de Vijver et al ., included
144 node-positive patients with no restriction to number of positive nodes. 8 To be able to
do more extensive analyses we selected all patients with only 1-3 positive nodes from this
series (n = 106).8
Follow-up was updated from a median of 7.4 years to 10.3 years (range, 1.6to 21.2 years).9 This patient series was significantly different from our here described new
series, with regard to age (median age 45 versus 50 years, respectively; p < 0.001), axillary
procedure (all ALND), adjuvant systemic therapy and survival probabilities ( Supplementary
Tables 3 and 4). Most differences can be attributed to the fact that these patients were selected
to be younger than 53 years and were diagnosed at earlier calendar years (before 1995)
when sentinel lymph node procedure was not available, and adjuvant systemic treatment
guidelines were not as comprehensive as today. The 10-year BCSS probability was 98% (SE
2%) for the good prognosis profile (43 patients), and 64% (SE 6%) for the poor prognosis
profile group (63 patients), respectively. In this series a poor prognosis signature was also

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 75/248
Chapter 5
84
associated with shorter BCSS, with a univariate HR of 6.60 (95% CI 1.97-22.10; p = 0.002) and
a multivariate HR (adjusted for the same variables as listed in table 2) of 3.63 (95% CI 0.88-
14.96; p = 0.07).
Figure 2. Kaplan-Meier curves by 70-gene prognosis signature and clinical risk groups among
the 241 patients. A) Breast cancer-specific survival. B) Distant metastasis-free survival (distant
metastasis as first event).
Time (years)
1086420
1.0
0.8
0.6
0.4
0.2
0.0
B r e a s t
c a n c e r - s p e c i fi c s u r v i v a l
Patients Events Risk g roup
5
72
27
137
1
4
0
28
Prognosis-signature good, clinical low risk
Prognosis-signature poor, clinical high risk
Prognosis-signature poor, clinical low risk
Prognosis-signature good, clinical high risk
Time (years)
1086420
1.0
0.8
0.6
0.4
0.2
0.0
D i s t a n t m e t a s t a s e s - f r e e s u r v i v a l
Patients Events Risk g roup
5
72
27
137
1
6
0
28
Prognosis-signature good, clinical low risk
Prognosis-signature poor, clinical high risk
Prognosis-signature poor, clinical low risk
Prognosis-signature good, clinical high risk
A
B

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 76/248
The 70-gene signature in pN1 breast cancer
85
5
Discussion
The present study demonstrates that molecular diagnostics can identify a group of low
risk patients within node-positive breast cancer patients who are traditionally viewed as
high risk for recurrence by conventional histopathological evaluation. As such, this study
underscores the added value of molecular diagnostics and more specifically of the 70-gene
prognosis signature in the tailoring of treatment for the individual patient.
The 70-gene prognosis signature, which was developed using tumors of lymph node-
negative patients, first demonstrated its prognostic power in node-positive breast cancer
in the paper by Van de Vijver et al ..8 In this study, patients with one up to any number of
positive nodes were included. Nevertheless, our present results are in good agreement
with this previous publication: the HR for DMFS of 4.13 (95% CI 1.72-9.96; p = 0.002) in our
series is similar to the prognostic value of the signature in the 151 node-positive patients
from the Van de Vijver study (HR for DMFS 4.5; 95% CI 2.0-10.2; p < 0.001).8
In our new independent validation series both the 70-gene prognosis signature and
traditional clinicopathological factors were predictive for BCSS. However, the multivariate
analyses clearly demonstrate that the 70-gene signature remained the most powerful
predictor for BCSS, even after adjustment for the clinicopathological factors, showing the
added value of the signature.
The signature performed as a significant prognostic factor for DMFS (DM as first event)
in the univariate analysis and retained this capacity at borderline significance when
adjusted for clinicopathological variables. For DMFS with distant metastasis as any eventthe signature remained a strong independent predictor (HR 3.83; 95% CI 1.40-10.47; p =
0.009). In addition, in a pooled multivariate analysis of our new independent series and
the 106 patients from the Van de Vijver study with extended follow-up, the HR for DMFS
(as first event) for the signature remained consistent at 2.79 (95% CI 1.29-6.02; p = 0.009)
( Supplementary Table 5A).
As a consequence of adjuvant treatment guidelines, a substantial proportion of patients
in this validation series (128 of 241 patients) received adjuvant chemotherapy, with or
without hormonal therapy. Patients classified as poor prognosis by the 70-gene signature
more often received adjuvant chemotherapy (67% versus 41%, respectively; p < 0.001). Tumor characteristics in the poor signature group, i.e. more ER-negative and poorly
differentiated, are generally believed to be associated with a higher likelihood of response
to chemotherapy.4 Moreover, Albain et al. recently presented data on the 21-gene recurrence
score (RS) in lymph node-positive patients, showing that node-positive patients classified
as high RS have more benefit from chemotherapy in addition to tamoxifen.13 The larger
efficacy of chemotherapy in combination with the larger proportion of chemotherapy-
treated patients in the poor prognosis signature group would imply that the prognostic
value of the 70-gene signature would potentially be higher in an untreated group. To
further investigate this, we performed subgroup analyses in the chemotherapy-treated

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 77/248
Chapter 5
86
and untreated group, and confirmed similar prognostic power in each subgroup (HRs 4.85
and 5.99, respectively). To determine potential heterogeneity of the prognostic value of
the signature among the chemotherapy-treated and untreated group, we also performed
a multivariate analysis including an interaction variable between the signature and
chemotherapy. In this multivariate analysis of our series and the 106 patients from the
Van de Vijver study combined, the 70-gene prognosis signature maintained its prognostic
value for BCSS (HR 5.50; 95% CI 1. 47-20.62; p = 0.01), while the interaction term did not
reach significance ( p = 0.95), showing no signal of potential difference in prognostic value
in the two groups ( Supplementary Table 5B).
The clinical utility of the 70-gene signature depends on its potential value in addition to
traditional prognostic factors. Therefore, we compared the signature to clinicopathological
risk assessment, by Adjuvant!.11,12 As anticipated, Adjuvant! classified the majority of these
node-positive patients as high clinical risk (87%). Interestingly, the 70-gene prognosis
signature classified 72 (34%) clinical high risk patients as good prognosis and indeed the
disease outcome in this discordant group (clinical high risk, good prognosis signature)
was remarkably good, with a 10-year BCSS of 94%, indicating that the use of this signature
could result in a substantial reduction of patients who would be recommended for
chemotherapy, without jeopardizing outcome.
Although several prognostic markers have been studied in breast cancer, the majority of
these markers have not been studied in node-positive breast cancer,14,15 or lack prognostic
value in node-positive disease.16 Some previously identified markers do have prognostic
value in node-positive breast cancer, however, since they do not identify a substantialgroup of patients with an excellent disease outcome, the clinical relevance as prognostic
marker for this node-positive patients’ group seems to be limited.13,17,18 The only other
signature that could identify a low risk group with a sufficiently good outcome within node-
positive patients was the wound signature.9 Since this wound signature is not available as a
diagnostic test, its value for clinical practice seems to be limited at this moment.
The strong prognostic power of the signature with respect to distant metastases
(hematogenous spread), regardless of nodal involvement, suggests that the molecular
mechanism of hematogenous metastases leading to distant metastases is different from
that of lymphogenic metastases leading to regional metastases.19
As stated by Fisher‘lymph node metastases seem to be only ‘‘indicators’’ and not ‘‘instigators’’ of metastatic
disease’.20 With the strong prognostic information provided by the 70-gene signature,
axillary staging might become less important for guiding adjuvant treatment. Since the
signature accurately classifies as many as 41% of patients with 1-3 positive nodes as good
prognosis, application of the 70-gene prognosis signature could result in a safe reduction
of chemotherapy treatment in up to 41% of these patients. The distant relapse rate of 3% at
10 years in chemotherapy-untreated patients who were classified as good prognosis by the
70-gene signature (data not shown), further substantiate that withholding chemotherapy
in this group seems justified, and implies a major change in the treatment of node-positive
breast cancer.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 78/248
The 70-gene signature in pN1 breast cancer
87
5
This independent retrospective validation study provides additional strong evidence that
the 70-gene signature is a powerful predictor of disease outcome in patients with 1-3
positive nodes, both in chemotherapy-treated and untreated patients. Based on the results
of this study the inclusion criteria of the MINDACT trial (EORTC 10041 BIG 3-04), which is
currently prospectively validating the 70-gene signature in node-negative patients, will be
enlarged to include patients with 1-3 positive nodes.21 Furthermore, our validation study
shows that the signature adds independent prognostic information to that provided by
traditional clinicopathological factors and can accurately identify patients with node-
positive breast cancer and an excellent disease outcome, which would allow a more
tailored approach for adjuvant systemic therapy in this patient group.
Acknowledgements
The authors would like to thank Hugo Horlings for providing immunohistochemistry
data and Dimitry Nuyten for updating the clinical data for the Van de Vijver series and
Michael Hauptman for helping with part of the statistical analyses. We are indebted to
Sjoerd Rodenhuis, Rene Bernards, Marleen Kok and Philippe Bedard for critically reading
the manuscript. This study was supported by the European Commission Framework
Programme VI-TRANSBIG, the Dutch National Genomics Initiative-Cancer Genomics Center,
and an unrestricted research grant from Agendia B.V.
Conflicts of Interest
Laura J Van ‘t Veer is a named inventor on a patent application for MammaPrint™ and
reports holding equity in Agendia B.V. Arno Floore and Annuska M Glas are employees of
Agendia B.V..

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 79/248
Chapter 5
88
References
1. Carter CL, Allen C, Henson DE. Relation of tumor size, lymph node status, and survival in 24,740 breast
cancer cases. Cancer 1989; 63: 181-187.
2. Page DL. Prognosis and breast cancer. Recognition of lethal and favorable prognostic types. Am J Surg
Pathol 1991; 15: 334-349.
3. Rosen PP, Groshen S, Saigo PE, Kinne DW, Hellman S. Pathological prognostic factors in stage I (T1N0M0)
and stage II (T1N1M0) breast carcinoma: a study of 644 patients with median follow-up of 18 years.
J Clin Oncol 1989; 7: 1239-1251.
4. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for
early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet
2005; 365: 1687-1717.
5. Joensuu H, Pylkkanen L, Toikkanen S. Long-term survival in node-positive breast cancer treated by
locoregional therapy alone. Br J Cancer 1998; 78: 795-799.
6. Buyse M, Loi S, Van ‘t Veer L, et al. Validation and clinical utility of a 70-gene prognostic signature for
women with node-negative breast cancer. J Natl Cancer Inst 2006; 98: 1183-1192.
7. Van ‘t Veer LJ, Dai H, Van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast
cancer. Nature 2002; 415: 530-536.
8. Van de Vijver MJ, He YD, Van ‘t Veer LJ, et al. A gene-expression signature as a predictor of survival in
breast cancer. N Engl J Med 2002; 347: 1999-2009.
9. Chang HY, Nuyten DSA, Sneddon JB, et al. Robustness, scalability, and integration of a wound-response
gene expression signature in predicting breast cancer survival. Proc Natl Acad Sci USA 2005; 102: 3738-3743.
10. Glas AM, Floore A, Delahaye LJ, et al. Converting a breast cancer microarray signature into a high-
throughput diagnostic test. BMC Genomics 2006; 7: 278-287.
11. Olivotto IA, Bajdik CD, Ravdin PM, et al. Population-based validation of the prognostic model
ADJUVANT! for early breast cancer. J Clin Oncol 2005; 23: 2716-2725.
12. Ravdin PM, Siminoff LA, Davis GJ, et al. Computer program to assist in making decisions about adjuvant
therapy for women with early breast cancer. J Clin Oncol 2001; 19: 980-991.
13. Albain K, Barlow W, Shak S., et al. Prognostic and predictive value of the 21-gene recurrence score assay
in postmenopausal, node-positive, ER-positive breast cancer (S8814, INT0100). San Antonio Breast
Cancer Symposium 2007 (abstract no 10).14. Desmedt C, Piette F, Loi S, et al. Strong time dependence of the 76-gene prognostic signature for node-
negative breast cancer patients in the TRANSBIG multicenter independent validation series. Clin Cancer
Res 2007; 13: 3207-3214.
15. Foekens JA, Atkins D, Zhang Y, et al. Multicenter validation of a gene expression-based prognostic
signature in lymph node-negative primary breast cancer. J Clin Oncol 2006; 24: 1665-1671.
16. Ma XJ, Hilsenbeck SG, Wang W, et al. The HOXB13:IL17BR expression index is a prognostic factor in
early-stage breast cancer. J Clin Oncol 2006; 24: 4611-4619.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 80/248
The 70-gene signature in pN1 breast cancer
89
5
17. Look MP, van Putten WL, Duffy MJ, et al. Pooled analysis of prognostic impact of urokinase-type
plasminogen activator and its inhibitor PAI-1 in 8377 breast cancer patients. J Natl Cancer Inst 2002; 94:
116-128.
18. Sorlie T, Tibshirani R, Parker J, et al. Repeated observation of breast tumor subtypes in independent
gene expression data sets. Proc Natl Acad Sci USA 2003; 100: 8418-8423.
19. Weigelt B, Wessels LF, Bosma AJ, et al. No common denominator for breast cancer lymph node
metastasis. Br J Cancer 2005; 93: 924-932.
20. Fisher B. The evolution of paradigms for the management of breast cancer: a personal perspective.
Cancer Res 1992; 52: 2371-2383.
21. Bogaerts J, Cardoso F, Buyse M, et al. Gene signature evaluation as a prognostic tool: challenges in the
design of the MINDACT trial. Nat Clin Pract Oncol 2006; 3: 540-551.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 81/248
Chapter 5
90
Supplements Chapter 5
Supplementary table 3. Clinical and pathological characteristics of new validation series (NKI-
EIO; n=241) and of the 106 patients selected from the Van de Vijver study (Ref. Van de Vijver et
al, NEJM 2002).
NKI-EIO
n = 241
Van de Vijver
n = 106 P value*
Characteristics No. % No. %
Age (years) < 0.001
Mean (SD) 50 (7) 45 (5)
<40 23 9.5 16 15.0
40 - 49 102 42.4 68 64.2
50 - 59 86 35.7 22 20.860 - 70 30 12.4 0 .0
Surgery 0.48
BCT 144 59.8 59 55.7
Mastectomy 97 40.2 47 44.3
Axillary procedure < 0.001
ALND 158 65.6 106 100.0
SLNP & ALND 83 34.4 0 .0
Nodal status 0.78
1 positive node 123 51.0 58 54.7
2 positive nodes 77 32.0 27 25.5
3 positive nodes 41 17.0 21 19.8
Tumor size (pTNM) 0.23
pT1 (≤ 20mm) 117 48.5 65 61.3
pT2 (> 20 - 50mm) 121 50.3 41 38.7
pT3 (> 50mm) 3 1.2 0 .0
Histological tumor type NA
Ductal 204 84.6 0 .0
Lobular 15 6.2 0 .0
Mixed 17 7.1 0 .0
Other 5 2.1 0 .0
Unknown 0 106 100.0Histological grade 0.07
Good 57 23.8 35 33.0
Moderate 99 41.5 41 38.7
Poor 83 34.7 30 28.3
Unknown 2 0
Estrogen-receptor status 0.56
Negative 50 20.7 18 18.0
Positive 191 79.3 82 82.0
Unknown 0 6

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 82/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 83/248
Chapter 5
92
Supplementary table 4. Association between clinicopathological characteristics and the 70-
gene prognosis-signature for 106 patients selected from the Van de Vijver study (Ref. Van de
Vijver NEJM 2002).
70-gene prognosis-signature
Good prognosis signature
(n=43)
Poor prognosis signature
(n=63) P value*
Characteristics No. % No. %
Age (years) 0.89
<40 4 9.3 12 19.1
40 - 49 32 74.4 36 57.1
50 - 55 7 16.3 15 23.8
Surgery 0.98
BCT 24 55.8 35 55.6Mastectomy 19 44.2 28 44.4
Axillary procedure NA
ALND 43 100.0 63 100.0
SLNP & ALND 0 .0 0 .0
Nodal status 0.82
1 positive node 24 55.8 34 54.0
2 positive nodes 11 25.6 16 25.4
3 positive nodes 8 18.6 13 20.6
Tumor size (pTNM) 0.14
pT1 (≤ 20mm) 30 69.8 35 55.6
pT2 (> 20 - 50mm) 13 30.2 28 44.4
Histological tumor type NA
Unknown 43 100.0 63 100.0
Histological grade < 0.001
Good 24 55.8 11 17.5
Moderate 18 41.9 23 36.5
Poor 1 2.3 29 46.0
Estrogen-receptor status 0.03
Negative 3 7.5 15 25.0
Positive 37 92.5 45 75.0
Unknown 3 3
Progesterone-receptor status < 0.001
Negative 4 10.0 28 46.7
Positive 36 90.0 32 53.3
Unknown 3 3
HER2/NEU receptor status 0.27
Negative 34 89.5 49 80.3
Positive 4 10.5 12 19.7
Unknown 5 2

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 84/248
The 70-gene signature in pN1 breast cancer
93
5
70-gene prognosis-signature
Good prognosis signature(n=43)
Poor prognosis signature(n=63)
P value*
Adjuvant systemic treatment 0.28
None 6 14.0 13 20.6
Chemotherapy only 26 60.4 37 58.8
Endocrine therapy only 4 9.3 9 14.3
Both 7 16.3 4 6.3
Adjuvant chemotherapy 0.20
No 10 23.3 22 34.9
Yes 33 76.7 41 65.1
Adjuvant endocrine therapy 0.55
No 32 74.4 50 79.4
Yes 11 25.6 13 20.6
Abbreviations: BCT, breast-conserving therapy; ALND, axillary lymph node dissection; SLNP, sentinel lymph
node procedure.
* Missing values were not used for calculation of p- values.
Supplementary table 4. Continued

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 85/248
Chapter 5
94
Supplementary table 5. Multivariate Cox-regression analyses for new validation series and 106
patients of Van de Vijver study combined; n=320.
a. Multivariate analysis for DM as first event n=320*
Variable P Value Hazard Ratio (95% CI)
Age (years) 0.11 0.97 (0.93 - 1.01)
No. of positive nodes 0.05
2 versus 1 0.48 0.77 (0.38 – 1.58)
3 versus 1 0.05 1.88 (1.01 – 3.49)
Tumor size (> 20 mm versus ≤ 20 mm) 0.16 1.52 (0.85 – 2.73)
Histological grade 0.14
Moderate versus good 0.83 1.10 (0.46 – 2.62)
Poor versus good 0.13 2.08 (0.81 – 5.35)Estrogen-receptor status 0.60 1.19 (0.62 – 2.30)
HER2/NEU receptor status 0.98 0.99 (0.51 – 1.92)
Surgery (mastectomy versus BCT) 0.33 1.31 (0.76 – 2.26)
Chemotherapy 0.03 0.50 (0.27 – 0.94)
Endocrine therapy 0.001 0.36 (0.19 – 0.67)
Prognosis-signature (poor versus good) 0.009 2.79 (1.29 – 6.02)
b. Multivariate analysis for BCSS including an interaction term n=320*
Variable P Value Hazard Ratio (95% CI)
Age (years) 0.35 0.98 (0.94 – 1.02)
No. of positive nodes 0.002
2 versus 1 0.28 0.65 (0.29 – 1.42)
3 versus 1 0.006 2.34 (1.28 – 4.27)
Tumor size (> 20 mm versus ≤ 20 mm) 0.90 1.04 (0.57 – 1.91)
Histological grade 0.14
Moderate versus good 0.77 0.87 (0.34 – 2.23)
Poor versus good 0.27 1.73 (0.66 – 4.60)
Estrogen-receptor status 0.79 0.91 (0.48 – 1.74)
HER2/NEU receptor status 0.90 1.04 (0.54 – 2.02)
Surgery (mastectomy versus BCT) 0.29 1.35 (0.77 – 2.38)
Chemotherapy 0.41 0.50 (0.10 – 2.63)
Endocrine therapy 0.01 0.42 (0.22 – 0.81)
Prognosis-signature (poor versus good) 0.01 5.50 (1.47 – 20.62)
Prognosis-signature * chemotherapy 0.95 0.95 (0.17 – 5.39)
Abbreviations: CI, confidence interval; BCT, breast-conserving therapy.
* Multivariate model included 320 patients due to missing values in 27 patients.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 86/248
The 70-gene signature in pN1 breast cancer
95
5
Supplementary figure 3. Kaplan-Meier curves by 70-gene prognosis-signature for breast
cancer specific survival among the 241 patients.
A) Chemotherapy naïve patients (n=101)
B) Chemotherapy-treated patients (n=128).
Time (years)
1086420
B r e a s t c a n c e r - s p e c i fi c s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
57
44
55
343 41 32 19
54 49 31 6
Poor prognosis-signature
Good prognosis-signatureNumbers at
risk
Log-rank p = 0.003
Time (years)
1086420
B r e a s t c a n c e r - s p e c i fi c s
u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
39
89
38
686 78 65 31
38 31 19 8
Poor prognosis-signature
Good prognosis-signatureNumbers at
risk
Log-rank p = 0.02
A
B

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 87/248
Chapter 6
Metastatic potential of T1 breast cancer
can be predicted by the 70-gene
MammaPrint signature
Stella Mook*
Michael Knauer*
Jolien M. Bueno de Mesquita
Valesca P. Retel
Jelle Wesseling
Sabine C. Linn
Laura J. Van ‘t Veer
Emiel J.Th. Rutgers* Contributed equally
Ann Surg Oncol 2010; 17:1406-1413

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 88/248
Chapter 6
98
Abstract
Background
Mammographic screening and increased awareness has led to an increase in the detection
of T1 breast tumors that are generally estimated as having low risk of recurrence after
locoregional treatment. However, even small tumors can metastasize, which leaves us
with the question for the necessity of adjuvant treatment. Therefore, additional prognostic
markers are needed to tailor adjuvant systemic treatment for these relatively low-risk
patients. The aim of our study was to evaluate the accuracy of the 70-gene MammaPrint™
signature in T1 breast cancer.
Materials and Methods
We selected 964 patients from previously reported studies with pT1 tumors (≤ 2 cm).
Frozen tumor samples were hybridized on the 70-gene signature array at the time of the
initial study and classified as having good prognosis or poor prognosis.
Results
The median follow-up was 7.1 years (range 0.2–25.2). The 10-year distant metastasis-free
(DMFS) and breast cancer specific survival (BCSS) probabilities were 87% (SE 2%) and91% (SE 2%), respectively, for the good prognosis-signature group (n = 525), and 72% (SE
3%) and 72% (SE 3%), respectively, for the poor prognosis signature group (n = 439). The
signature was an independent prognostic factor for BCSS at 10 years (multivariate hazard
ratio [HR] 3.25 [95% confidence interval, CI, 1.92–5.51; p < 0.001]). Moreover, the 70-gene
MammaPrint™ signature predicted DMFS at 10 years for 139 patients with pT1ab cancers
(HR 3.45 [95% CI 1.04-11.50, P = 0.04]).
Conclusions
The 70-gene MammaPrint™ signature is an independent prognostic factor in patients with
pT1 tumors and can help to individualize adjuvant treatment recommendation in this
increasing breast cancer population.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 89/248
The 70-gene signature in pT1 breast cancer
99
6
Introduction
Primary tumor size, in addition to axillary lymph node status, is considered to be one of
the most important prognostic factors in breast cancer, with small tumor size being an
indicator of good prognosis.1-5 However, even small tumors can metastasize, suggesting
that the ability to metastasize is an early and inherent genetic property. 6,7 Adjuvant
treatment decisions based on tumor size alone are only moderately accurate and could
result in undertreatment of T1ab and overtreatment of T1c tumors. The need for adjuvant
systemic therapy after locoregional therapy for patients with small tumors is unresolved.8,9
Currently used treatment guidelines give different recommendations for pT1ab and pT1c
tumors and often the advice ‘consider chemotherapy’ is given, without providing specific
advice for the use of prognostic factors.10-12
With the widespread introduction of breast cancer screening programs and increased
awareness, the proportion of patients presenting with small tumors is ever increasing;
therefore, robust and reliable prognostic factors that can identify patients who are at high
risk of developing distant metastases despite their small tumor are needed.13-15 In previous
validation studies, the 70-gene MammaPrint™ signature accurately distinguished patients
with a good prognosis from those with a poor prognosis in both node-negative and node-
positive breast cancer.16-21 The aim of our study was to evaluate the prognostic value of the
70-gene signature in small pT1 tumors. In addition, we investigated whether the 70-gene
signature could provide clinical utility; that is, if it was able to identify a subgroup of patients
with pT1ab tumors with a poor prognosis as indication for chemotherapy and a subgroupof patients with a pT1c tumor and a good prognosis as indication for no adjuvant treatment
or endocrine therapy only. We merged databases from previous studies to overcome the
underrepresentation of pT1 tumors.16-18,20-23
Methods
Patients
For this study we selected patients with pT1 tumors from previously reported studies.16-18,20-23
Selection criteria for the initially reported studies are depicted in Supplementary Figure 1. For 2
series (i.e., 295-series and RASTER-series) the follow-up was updated since initial publication
(median updated follow-up 10.3 and 2.4 years, respectively).16,22 Each of the series were
consecutive selections from the comprehensive institutional tissue banks. Patients in series
1, 4, 5, and 6 received adjuvant systemic therapy according to national guidelines applicable
at that time.16,18,20,21,24Patients from series 2 and 7 were selected based on adjuvant systemic
therapy received, that is, no adjuvant systemic therapy for patients in series 2 and adjuvant
tamoxifen monotherapy for patients in series 7.17,23 Patients from series 3 (prospective

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 90/248
Chapter 6
100
RASTER trial) were treated according to the national Dutch guideline and the result of the
70-gene signature.22,24 There were 15 patients, all classified as poor prognosis-signature
(1.6%), who received adjuvant trastuzumab. All individual studies were approved by the
ethical committee of the respective hospitals.
70-gene MammaPrint™ signature
Frozen tumor samples were processed at Agendia’s laboratories (Amsterdam, the
Netherlands), for RNA isolation, amplification, and labeling as previously described.7,25
Samples were eligible for RNA isolation if they contained at least 30–50% tumor cells on
hematoxylin/eosin stained sections. To assess the mRNA expression level of the 70 genes,
RNA was hybridized to a custom-designed array (MammaPrint™), blinded to clinical data,
at Agendia’s ISO17025-certified and CLIA accredited laboratories. Tumors were classified
as 70-gene good or poor prognosis signature at time of the initial series as described
previously.16-18,20-23 On average, the 70-gene signature could be performed in 81% of the
patients, which is in accordance with our previously published feasibility study.26 When
sufficient RNA could be extracted, the success rate of hybridization was 100%. For detailed
information about dropout of patients because of tumor cell content or RNA quality, we
refer to the initial publications.
Endpoints
Endpoints considered were time from surgery to distant metastasis (DMFS), and breast
cancer specific survival (BCSS), defined as time from surgery to breast cancer-related death.
For the analysis of distant metastasis-free survival (DMFS) we considered distant metastases
as failure; patients were censored on date of death from causes other than breast cancer or
date of last follow-up visit. For the analysis of BCSS, patients were censored on date of last
follow-up or date of death from causes other than breast cancer. Clinicopathological data
were collected as previously reported, and databases were pooled for our current study (M.
Knauer, unpublished).
Statistical analyses
Associations between 70-gene signature and classical clinicopathological factors were
studied using chi-square and Mann–Whitney tests. Kaplan–Meier survival analyses and
log-rank tests were used to assess the difference in distant metastasis-free survival (DMFS)
and breast cancer-specific survival (BCSS) of the predicted good- and poor prognosis
groups by the signature. Cox proportional hazard analyses were used to calculate
univariate and multivariate hazard ratios (HR) and their 95% confidence intervals (95% CI).
Multivariate Cox proportional hazard analyses included the 70-gene signature and known

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 91/248
The 70-gene signature in pT1 breast cancer
101
6
clinicopathological prognostic factors. We missed information about grade (n = 10), nodal
status (n = 8), ER status (n = 1), and adjuvant systemic therapy (n = 4) for a small proportion
of the patients. These patients were excluded for the multivariate Cox proportional hazard
analyses. HRs for DMFS and BCSS at 10 years were calculated with right-censoring follow-
up > 10 years, because timing of collection of follow-up data differed for the 7 series.
Hazard ratios with their 95% CI for the 7 patient series were displayed on forest plots and
tested for heterogeneity using a chi-square test with 6 degrees of freedom. All p-values are
two-sided. Analyses were performed using SPSS version 15.0 (SPSS Inc, Chicago, IL) and
Revman 5 (Review Manager) (www.cc-ims.net/revman).
Results
A total of 964 patients with pT1 tumors were selected from the 7 studies ( Supplementary Figure 1).16-18,20-23 Among the 964 patients, 139 patients (14%) had a pT1ab tumor, 825 patients (86%)
had a pT1c tumor, 693 patients (72%) had node-negative breast cancer, and 263 patients
(27%) had node-positive breast cancer. During follow-up (median 7.1 years; range 0.2-25.2
years) 154 patients developed distant metastases and 155 patients died, of whom 130 of
breast cancer.
The signature classified 525 tumors (54%) as good prognosis and 439 (46%) tumors as
poor prognosis. A poor prognosis signature was associated with younger age at diagnosis,
invasive ductal carcinoma, poorly differentiated, ER negative and HER2 positive tumors.In addition, patients with a 70-gene poor prognosis tumor more often received adjuvant
systemic therapy (Table 1).
DMFS and BCSS were significantly better in the good prognosis group ( Figure 1A and B). The
probability of remaining free of distant metastases at 5 and 10 years were 95% (SE 1%)
and 87% (SE 2%), respectively for the good prognosis-signature group, and 80% (SE 2%)
and 72% (SE 3%), respectively for the poor prognosis-signature group (Figure 1A). A poor
prognosis-signature was associated with worse DMFS at 10 years, with a univariate hazard
ratio (HR) of 2.70 (95% CI 1.88-3.88; p < 0.001). The 5- and 10-year BCSS probabilities were
99% (SE 1%) and 91% (SE 2%), respectively, for the good prognosis group and 88% (SE 2%)and 72% (SE 3%), respectively, for the poor prognosis-signature group, with a univariate HR
of 4.22 (95% CI 2.70-6.60; p < 0.001) at 10 years (Figure 1B). Forest plots of univariate hazard
ratios for the signature in each individual series showed no significant heterogeneity for
the prognostic value of the signature for both DMFS (chi square = 6.18; p = 0.4) and BCSS
(chi square = 5.99; p = 0.4) ( Supplementary Figure 2).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 92/248
Chapter 6
102
Table 1. Association between clinicopathological characteristics and the 70-gene signature.
Good prognosis profile Poor prognosis profile P -value*
Surgery 0.09BCT 402 76.6% 315 71.8%
Mastectomy 123 23.4% 124 28.2%
Age <0.001
≤ 50 yrs 282 53.7% 290 66.1%
> 50 yrs 243 46.3% 149 33.9%
Histology <0.001
IDC 435 82.9% 399 90.9%
ILC 54 10.3% 17 3.9%
Others 36 6.8% 23 5.2%
Tumor size 0.13pT1a/b 84 16.0% 55 12.5%
pT1c 441 84.0% 384 87.5%
Nodal status 0.69
Node negative 380 73.1% 313 71.8%
Node positive 140 26.9% 123 28.2%
Unknown 5 3
Grade <0.001
Grade 1 224 43.0% 56 12.9%
Grade 2 248 47.6% 164 37.9%
Grade 3 49 9.4% 213 19.2%
Unknown 4 6
Estrogen-receptor status <0.001
Positive 513 97.7% 295 67.4%
Negative 12 2.3% 143 32.6%
Unknown 0 1
HER2 status <0.001
Negative 402 95.7% 253 77.6%
Positive 18 4.3% 73 22.4%
Unknown 105 113
Adjuvant systemic therapy <0.001
None 357 68.3% 195 44.6%
HT only 113 21.6% 79 18.1%
CT only 22 4.2% 76 17.4%
HT & CT 31 5.9% 87 19.9%
Unknown 2 2
Total 525 100.0% 439 100.0%
* Missing data were not used for calculation of p-values
BCT, breast-conserving therapy; IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma; ER, estrogen
receptor; HT, hormonal therapy; CT, chemotherapy.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 93/248
The 70-gene signature in pT1 breast cancer
103
6
Figure 1. Kaplan-Meier curves and univariate hazard ratio (HR) for distant metastasis-free
survival (DMFS) and breast cancer-specific survival (BCSS) by 70-gene prognosis-signature for
964 patients with pT1 breast tumors (A and B), for 139 patients with pT1ab tumors (C and D), and
for 825 patients with pT1C tumors (E and F).
Time (years)
1086420
D i s t a n t m e t a s t a s e s - f r e e s u
r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
525
439
456
117384 261 221 172
336 290 234 169
Poor prognosis-signature
Good prognosis-signatureNumbers at
risk
Log-rank p < 0.001
HR at 10 yrs: 2.70 (95% CI 1.88-3.88); p < 0.001
95%
80%
87%
72%
1086420
B r e a s t c a n c e r - s p e c i fi c s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
525
439
460
124400 284 239 183
344 300 252 179
Poor prognosis-signature
Good prognosis-signatureNumbers at
risk
Log-rank p < 0.001
99%
88%
72%
91%
HR at 10 yrs: 4.22 (95% CI 2.70-6.60); p < 0.001
Time (years)
Time (years)
1086420
D i s t a n t m e t a s t a s e s - f r e e s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
84
55
67
1049 28 22 16
49 37 33 25
Poor prognosis-signature
Good prognosis-signatureNumbers atrisk
Log-rank p = 0.016
98%
86%
90%
76%
HR at 10 yrs: 3.45 (95% CI 1.04-11.50); p = 0.04
1086420
B r e a s t c a n c e r - s p e c i fi c s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
84
55
69
1051 28 24 17
50 39 34 25
Poor prognosis-signature
Good prognosis-signatureNumbers atrisk
Time (years)
Log-rank p = 0.06
100%
90%
88%
73%
HR at 10 yrs: 3.12 (95% CI 0.91-10.67); p = 0.07
Time (years)
1086420
D i s t a n t m e t a s t a s e s - f r e e s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
441
384
388
107335 234 199 156
287 253 201 144
Poor prognosis-signature
Good prognosis-signatureNumbers at
risk
Log-rank p < 0.001
95%
80%
86%
72%
HR at 10 yrs: 2.61 (95% CI 1.78-3.82); p < 0.001
1086420
B r e a s t c a n c e r - s p e c i fi c s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
441
384
392
114350 256 215 168
294 261 218 154
Poor prognosis-signature
Good prognosis-signatureNumbers at
risk
Time (years)
Log-rank p < 0.001
99%
88%
92%
72%
HR at 10 yrs: 4.42 (95% CI 2.73-7.17); p < 0.001
A
C
E
B
D
F

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 94/248
Chapter 6
104
Univariate analysis showed that besides the 70-gene signature, age, histology, tumor
grade, ER status, HER2 status, and type of surgery were significant predictors for DMFS at 10
years. The 70-gene signature, age, tumor grade, ER status, and HER2 status were significant
predictors for BCSS at 10 years ( Supplementary table 1). In a multivariate model, the 70-gene
signature was the strongest predictor for DMFS, with an adjusted HR of 2.43 (95% CI 1.56-
3.77; p < 0.001). In addition to the signature, nodal status and adjuvant systemic therapy
were independent significant predictors for DMFS. For BCSS, again the signature, nodal
status, and adjuvant chemotherapy were independent prognostic factors with adjusted
HRs of 3.25 (95% CI 1.92-5.51; p < 0.001), 1.70 (95% CI 1.12-2.57; p = 0.01) and 0.41 (95% CI
0.22-0.75; p = 0.004), respectively (Table 2).
Table 2. Multivariate Cox proportional hazard analyses for distant metastasis-free survival and
breast cancer-specific survival at 10 years.
VariableDistant metastases
Breast cancer-specific
survival
HR CI P-value HR CI P-value
MammaPrint (poor versus good signature) 2.43 1.56-3.77 <0.001 3.25 1.92-5.51 < 0.001
Age (years) 0.99 0.97-1.01 0.31 0.98 0.96-1.01 0.16
Histology
ILC (versus IDC) 1.41 0.70-2.83 0.33 1.70 0.81-3.57 0.16
Other (versus IDC) 0.39 0.12-1.26 0.12 0.46 0.14-1.48 0.19
Tumor size (11-20 mm versus ≤10 mm) 1.07 0.59-1.97 0.82 0.88 0.46-1.67 0.69
Nodal status (negative versus positive) 1.61 1.13-2.29 0.01 1.70 1.12-2.57 0.01
Grade
Grade 2 (versus grade 1) 1.28 0.77-2.11 0.34 1.31 0.72-2.39 0.38
Grade 3 (versus grade 1) 1.65 0.93-2.92 0.09 1.53 0.79-2.96 0.21
ER status (negative versus positive) 0.92 0.58-1.46 0.72 1.36 0.85-2.17 0.20
HER2/NEU status
Positive (versus negative) 1.19 0.69-2.04 0.53 1.48 0.84-2.61 0.18
Unknown (versus negative) 0.75 0.48-1.19 0.22 0.94 0.57-1.55 0.80
Surgery (mastectomy versus BCT) 1.38 0.95-1.99 0.09 1.23 0.82-1.85 0.32
Hormonal therapy (versus no hormonal therapy) 0.55 0.34-0.89 0.02 0.61 0.34-1.07 0.09
Chemotherapy (versus no chemotherapy) 0.50 0.29-0.84 0.01 0.41 0.22-0.75 0.004
Multivariate models included 941 patients due to missing values for nodal status, grade, and/or ER status
in 23 patients.
IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma; ER, estrogen receptor; BCT, breast-
conserving therapy; HR, hazard ratio; CI 95%, confidence interval.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 95/248
The 70-gene signature in pT1 breast cancer
105
6
Besides our initial selection of patients with tumors ≤ 20 mm, we divided our study cohort
into patients with pT1ab tumors (≤ 10 mm) (n = 139) and patients with pT1c tumors (11-20
mm) (n = 825). Of the patients with a pT1ab tumor, 40% were classified as having a 70-gene
poor prognosis tumor. The DMFS in these 55 patients was significantly worse compared
with the DMFS in patients with a good prognosis signature tumor during the entire follow-
up (log rank p = 0.016) and at 10 years (HR 3.45 [95% CI 1.04-11.50; p = 0.044]). The same
trend was seen for BCSS at 10 years, albeit borderline significant (Figure 1, panel C and D). The
number of events was too small to calculate adjusted HRs in patients with pT1ab tumors.
In patients with a pT1c tumor the 70-gene signature was a prognostic factor for both DMFS
and BCSS at 10 years (HR 2.61 [95% CI 1.78-3.82; p < 0.001] and 4.42 [95% CI 2.73-7.17; p <
0.001], respectively) (Figure 1, panel E and F ).
Among the 964 patients in our study cohort, 552 patients (57%) received no adjuvant
systemic therapy, 408 patients (42%) received endocrine- and/or chemotherapy and for
4 patients (1%) adjuvant systemic therapy was unknown. The 70-gene signature retained
its prognostic value in adjuvantly untreated patients, with adjusted HRs of 2.54 (95% CI
1.49-4.34; p = 0.001) and 3.47 (95% CI 1.83-6.60; p < 0.001) for DMFS and BCSS, respectively
( Supplementary Figure 3). In addition, the 70-gene MammaPrint™ signature was an independent
prognostic factor in 788 patients with ER positive tumors for both DMFS and BCSS, with
adjusted HRs of 2.51 (95% CI 1.60-3.95; p < 0.001) and 3.43 (95% CI 1.98-5.95; p < 0.001),
respectively.
Discussion
Our study showed that the 70-gene MammaPrint™ signature that has been validated as
an independent prognostic factor in node-negative and node-positive breast cancer is
also an independent prognostic factor in patients with small breast tumors. The signature
accurately distinguished patients with a good outcome from those with a poor outcome in
our study cohort of patients with pT1 tumors. Interestingly, our results showed that even
a considerable proportion of small tumors have a substantial metastatic capacity, which
can be identified by the 70-gene signature (28% distant relapse rate at 10 years in tumorsclassified as poor prognosis by the signature). Therefore, the 70-gene signature can be of
use in daily clinical practice to optimize and individualize treatment decision-making in
this growing breast cancer population of patients with pT1 tumors.
Historical tumor banks contain particularly large tumors, which is in contrast to the actual
increase in proportion of small tumors diagnosed, due to mammographic screening.
As a consequence, most studies of potential prognostic markers to date included fewer
than 10% of tumors smaller than 10 mm.7,27-29 To overcome this potential problem of
underrepresentation of small tumors in repositories we selected patients with pT1 tumors
from previous studies. One of the potential limitations of our pooled database is therefore

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 96/248
Chapter 6
106
the heterogeneity of our study population, especially with regard to years of diagnosis and
adjuvant systemic therapy. However, there was no evidence of significant heterogeneity
among the various series that provided pT1 cases for our study, for both DMFS and BCSS
( Supplementary Figure 2). Another potential bias with regard to adjuvant systemic therapy in
our study cohort is the fact that patients from the more recent prospective RASTER trial
were partially treated based on the outcome of the 70-gene signature.22 However, when
we excluded these patients from our series (n = 301) the 70-gene prognosis signature
retained its independent prognostic value with adjusted HRs for DMFS and BCSS of 2.32
(95% CI 1.48-3.63; p < 0.001) and 3.09 (95% CI 1.82-5.24; p < 0.001), respectively. Patients
with pT1 tumors selected from series 1 included 31 patients whose data were used in the
development of the 70-gene signature, thereby potentially causing an overestimation of
the prognostic value of the signature.7 Excluding these patients from our analyses resulted
in similar adjusted HR for both DMFS and BCSS at 10 years (2.24 [1.41-3.54; p = 0.001] and
3.10 [1.79-5.37; p < 0.001] respectively).
Our study cohort contained 139 patients with pT1ab tumors, and in this small group of
patients with pT1ab tumors 15 distant metastases (DM) and 11 breast cancer-specific
deaths (BCSD) occurred. The 70-gene signature was able to distinguish patients with pT1ab
tumors who developed DM from those who did not (log rank p = 0.016 and HR 3.45, p
= 0.044). For BCSS the same trend was observed, but did not, however, reach statistical
significance, which is most likely because of the low number of events in combination
with the relatively small patient population with pT1ab tumors. The results of our study
suggest that the 70-gene signature can select patients with pT1ab tumors with a higherrisk of developing DM (24% at 10 years), who thus might be candidates for adjuvant
systemic therapy. In addition, the signature can identify patients with a pT1c tumor with
a relatively low risk of developing DM (14% at 10 years), who might be sufficiently treated
with endocrine therapy, as the large majority (98%) is ER positive. Since adjuvant systemic
treatment recommendation for patients with small tumors is a matter of debate, our results
provide evidence that selecting patients with pT1 tumors using the 70-gene signature
could be relevant for adjuvant systemic therapy recommendation. For patients with pT1ab
tumors the data suggest the same, though we will have to await results of further studies.
With the current development of RNA extraction from FNA and core biopsies for microarraygene expression analyses, gene expression profiles will become available to a larger extent
for patients with very small tumors.30
Hanrahan and colleagues showed that, in addition to a relatively wide range of observed
relapse-free survival rates in patients with pT1abN0 tumors, histological grade, ER negative
tumor, younger age at diagnosis (<50 years), lymphovascular invasion (LVI), high Ki-67,
HER2/NEU positivity, and larger tumor size were associated with poor outcome. 8,9 In our
database of patients with pT1 tumors, we confirmed the univariate prognostic value of age,
tumor grade, ER and HER2/NEU ( Supplementary Table 1). Among the 954 patients with known
tumor grade, 692 patients had a grade 1 or 2 tumor and 262 patients had a grade 3 tumor.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 97/248
The 70-gene signature in pT1 breast cancer
107
6
Patients with a grade 1–2 tumor had a significantly lower 10 -year distant relapse rate
compared with those with a grade 3 tumor (16 and 29%, respectively), with a univariate
HR of 2.24 (95% CI 1.54-3.08; p < 0.001) ( Supplementary Figure 4). However, the event rate in
patients considered to have a ‘good prognosis’ based on grade ( i.e., with grade 1-2 tumors)
was relatively large. Specifically, classification based on grade (i.e., grade 1-2 considered low
risk) resulted in misclassification of 43 additional DM and 41 additional BCSD, compared
with 4 additional misclassified DM and 3 BCSD when classified by the 70-gene signature.
Classification based on ER status, would result in a large ‘good-prognosis’ group (i.e., 84%
is ER positive), with a relatively high event rate in this group (19% DM at 10 years) (data
not shown). Therefore, ER status alone would not be useful to select patients with pT1
tumors for adjuvant systemic chemotherapy. These results show that while the proportion
of patients classified as having a ‘good prognosis’ by both grade and ER status increased
compared with the good prognosis group by the 70-gene signature, the prediction of
outcome becomes less accurate and an increased proportion of events were missed.
Moreover, results of multivariate analyses showed that the prognostic information that is
captured by ER and grade is not independent of other factors. In fact, only the 70-gene
signature, nodal status, and adjuvant systemic therapy were independent prognostic
factors for DMFS and BCSS in this study cohort.
Tumors identified as 70-gene signature low risk and grade 1/2 showed a considerable
proportion of events (51 DM and 32 BCSD, respectively). However, these misclassified
events occurred significantly later compared with the accurately classified events, 7.4 years
(SE 0.4) versus 3.1 years (SE 0.2), respectively, for DM ( p < 0.001) and 9.3 yrs (SE 0.5) versus 4.6 years (SE 0.3), respectively, for BCSD ( p < 0.001). Previous studies have already shown
a time dependency for the prognostic value of the 70-gene signature, and our results
support once more the hypothesis of a different biological mechanism for early and late
relapses.17,21 Moreover, our results show the still unmet need for markers to predict late
events. The accuracy of the 70-gene MammaPrint™ signature in predicting early events
coincides with the effect of chemotherapy, as that is known to be most beneficial in the
first 5-7 years after diagnosis and would thus potentially prevent the occurrence of early
metastasis in the poor prognosis group.31
As a consequence of adjuvant treatment guidelines, a substantial proportion of patients inthis validation series (216 of 964 patients, 22%) received adjuvant chemotherapy, with or
without hormonal therapy. Patients classified as poor prognosis by the 70-gene signature
more often received adjuvant chemotherapy (37 versus 10% in the good prognosis group,
respectively; p < 0.001). Tumor characteristics in the poor signature group, that is, more ER-
negative and poorly differentiated, are generally believed to be associated with a higher
likelihood of response to chemotherapy.31 Moreover, Bender and colleagues recently
showed that the benefit of chemotherapy was exclusively seen in patients classified as poor
prognosis by the 70-gene signature.32 This larger efficacy of chemotherapy in combination
with the larger proportion of chemotherapy-treated patients in the poor prognosis

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 98/248
Chapter 6
108
signature group would imply that the prognostic value of the 70-gene signature as shown
in our series is underestimated and would potentially be higher in an untreated group.
In conclusion, our study shows that the 70-gene signature is a strong and independent
prognostic factor for patients with pT1 tumors. In addition, we show that a considerable
proportion of small tumors has metastatic potential, supporting the idea that metastatic
capacity is an early genetic inheritance that can be revealed by the 70-gene signature.
Consequently, selecting patients with pT1 tumors based on the signature will result in a
more accurate allocation of adjuvant systemic therapy in this patient population.
Acknowledgements
We are indebted to Marleen Kok and Rutger Koornstra for providing part of the data used
for our analyses and to Annuska M. Glas and Arno Floore of Agendia BV for hybridization of
all tumor samples. We thank Marjanka K. Schmidt for helpful discussions.
Conflicts of Interest
Laura J Van ‘t Veer is named inventor on a 70 gene prognosis-signature patent. Laura J Van
‘t Veer reports holding equity in Agendia BV.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 99/248
The 70-gene signature in pT1 breast cancer
109
6
References
1. Carter CL, Allen C, Henson DE. Relation of tumor size, lymph node status, and survival in 24,740 breast
cancer cases. Cancer 1989; 63: 181-187.
2. Fitzgibbons PL, Page DL, Weaver D, et al . Prognostic factors in breast cancer. College of American
Pathologists Consensus Statement 1999. Arch Pathol Lab Med 2000; 124: 966-978.
3. Koscielny S, Tubiana M, Le MG, et al . Breast cancer: relationship between the size of the primary tumour
and the probability of metastatic dissemination. Br J Cancer 1984; 49: 709-715.
4. Page DL. Prognosis and breast cancer. Recognition of lethal and favorable prognostic types. Am J Surg
Pathol 1991; 15: 334-349.
5. Rosen PP, Groshen S, Saigo PE, Kinne DW, Hellman S. Pathological prognostic factors in stage I (T1N0M0)
and stage II (T1N1M0) breast carcinoma: a study of 644 patients with median follow-up of 18 years. J
Clin Oncol 1989; 7: 1239-1251.
6. Bernards R and Weinberg RA. A progression puzzle. Nature 2002; 418: 823.
7. Van ‘t Veer LJ, Dai H, Van de Vijver MJ, et al . Gene expression profiling predicts clinical outcome of breast
cancer. Nature 2002; 415: 530-536.
8. Hanrahan EO, Valero V, Gonzalez-Angulo AM, Hortobagyi GN. Prognosis and management of patients
with node-negative invasive breast carcinoma that is 1 cm or smaller in size (stage 1; T1a,bN0M0): a
review of the literature. J Clin Oncol 2006; 24: 2113-2122.
9. Hanrahan EO, Gonzalez-Angulo AM, Giordano SH, et al . Overall survival and cause-specific mortality of
patients with stage T1a,bN0M0 breast carcinoma. J Clin Oncol 2007; 25: 4952-4960.
10. Eifel P, Axelson JA, Costa J, et al . National Institutes of Health consensus development conference
statement: Adjuvant therapy for breast cancer, November 1-3, 2000. J Natl Cancer Inst 2001; 93: 979-989.
11. NCCN Clinical Practice Guidelines in Oncology. Breast Cancer V.1.2009. www.nccn.org 2009.
12. Goldhirsch A, Ingle JN, Gelber RD, et al . Thresholds for therapies: highlights of the St. Gallen International
Expert Consensus on the primary therapy of early breast cancer 2009. Ann Oncol 2009; 20:1319–1329.
13. Fracheboud J, Otto SJ, van Dijck JA, et al . Decreased rates of advanced breast cancer due to
mammography screening in The Netherlands. Br J Cancer 2004; 91: 861-867.
14. Connor RJ, Chu KC, Smart CR. Stage-shift cancer screening model. J Clin Epidemiol 1989; 42: 1083-1095.
15. Chu KC, Smart CR, Tarone RE. Analysis of breast cancer mortality and stage distribution by age for the
Health Insurance Plan clinical trial. J Natl Cancer Inst 1988; 80: 1125-1132.16. Van de Vijver MJ, He YD, Van ‘t Veer LJ, et al . A gene-expression signature as a predictor of survival in
breast cancer. N Engl J Med 2002; 347: 1999-2009.
17. Buyse M, Loi S, Van ‘t Veer L, et al . Validation and clinical utility of a 70-gene prognostic signature for
women with node-negative breast cancer. J Natl Cancer Inst 2006; 98: 1183-1192.
18. Bueno de Mesquita JM, Linn SC, Keijzer R et al. Validation of 70-gene prognosis signature in node-
negative breast cancer. Breast Cancer Res Treat 2009; 117: 483–495.
19. Wittner BS, Sgroi DC, Ryan PD, et al . Analysis of the MammaPrint breast cancer assay in a predominantly
postmenopausal cohort. Clin Cancer Res 2008; 14: 2988-2993.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 100/248
Chapter 6
110
20. Mook S, Schmidt MK, Viale G, et al . The 70-gene prognosis-signature predicts disease outcome in breast
cancer patients with 1-3 positive lymph nodes in an independent validation study. Breast Cancer Res Treat
2009; 116: 295-302.
21. Mook S, Schmidt MK, Weigelt B, et al . The 70-gene prognosis signature predicts early metastasis in
breast cancer patients between 55 and 70 years of age. Ann Oncol 2010; 21: 717-722.
22. Bueno de Mesquita JM, Van Harten WH, Retel VP, et al . Use of 70-gene signature to predict prognosis of
patients with node-negative breast cancer: a prospective community-based feasibility study (RASTER).
Lancet Oncol 2007; 8: 1079-1087.
23. Kok M, Koornstra RH, Mook S, et al . Additional value of the 70-gene signature and levels of ER and PR for
the prediction of outcome in tamoxifen-treated ER-positive breast cancer. 2009 submitted .
24. CBO Richtlijn Mammacarcinoom 2008. http://www.cbo.nl/product/richtlijnen/folder20021023121843/rl_mamma_08. pdf
25. Glas AM, Floore A, Delahaye LJ, et al . Converting a breast cancer microarray signature into a high-
throughput diagnostic test. BMC Genomics 2006; 7: 278-287.
26. Mook S, Bonnefoi H, Pruneri G, et al . Daily clinical practice of fresh tumour tissue freezing and gene
expression profiling; logistics pilot study preceding the MINDACT trial. Eur J Cancer 2009; 45: 1201-1208.
27. West M, Blanchette C, Dressman H, et al . Predicting the clinical status of human breast cancer by using
gene expression profiles. Proc Natl Acad Sci USA 2001; 98: 11462-11467.
28. Sorlie T, Perou CM, Tibshirani R, et al . Gene expression patterns of breast carcinomas distinguish tumor
subclasses with clinical implications. Proc Natl Acad Sci USA 2001; 98: 10869-10874.
29. Huang E, Cheng SH, Dressman H, et al . Gene expression predictors of breast cancer outcomes. Lancet
2003; 361: 1590-1596.
30. Andre F, Michiels S, Dessen P, et al . Exonic expression profiling of breast cancer and benign lesions: a
retrospective analysis. Lancet Oncol 2009; 10: 381-390.
31. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for
early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet
2005; 365: 1687-1717.
32. Bender RA, Knauer M, Rutgers EJ, et al . The 70-gene profile and chemotherapy benefit in 1,600 breast
cancer patients. ASCO Annual Meeting Proceedings 2009. J Clin Oncol 2009; 27 (Supplement; abstract no.
512).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 101/248
The 70-gene signature in pT1 breast cancer
111
6
Supplements Chapter 6
Supplementary Table 1. Univariate Cox-regression analyses for distant metastasis-free survival
and breast cancer-specific survival at 10 years.
Distant metastasesBreast cancer-specific
survival
Variable HR CI P -value HR CI P-value
MammaPrint (poor versus good signature) 2.70 1.88-3.88 <0.001 4.22 2.70-6.60 <0.001
Age (years) 0.98 0.96-0.996 0.02 0.97 0.95-0.99 0.004
Histology
ILC (versus IDC) 0.96 0.49-1.90 0.91 1.07 0.52-2.21 0.85
Other (versus IDC) 0.37 0.09-0.88 0.05 0.45 0.17-1.23 0.12
Tumor size (11-20 mm versus ≤10 mm) 1.49 0.82-2.69 0.19 1.23 0.66-2.29 0.52
Nodal status (negative versus positive) 1.07 0.94-1.21 0.29 0.94 0.77-1.16 0.58
Grade
Grade 2 (versus grade 1) 1.57 0.97-2.54 0.07 1.85 1.04-3.29 0.04
Grade 3 (versus grade 1) 2.89 1.79-4.67 <0.001 3.82 2.18-6.71 <0.001
ER status (negative versus positive) 1.78 1.19-2.65 0.005 2.86 1.91-4.29 <0.001
HER2/NEU status
Positive (versus negative) 1.67 1.00-2.78 0.05 2.43 1.42-4.14 0.001Unknown (versus negative) 0.89 0.60-1.32 0.56 1.22 0.80-1.87 0.35
Surgery (mastectomy versus BCT) 1.54 1.09-2.20 0.02 1.43 0.96-2.11 0.08
Hormonal therapy (versus no hormonal therapy) 0.73 0.49-1.08 0.11 0.67 0.42-1.05 0.08
Chemotherapy (versus no chemotherapy) 1.04 0.68-1.58 0.88 0.98 0.60-1.59 0.93
IDC, Invasive ductal carcinoma; ILC, invasive lobular carcinoma; ER, estrogen receptor; BCT, breast-conserving
therapy; HR, hazard ratio; CI, 95% confidence interval.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 102/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 103/248
The 70-gene signature in pT1 breast cancer
113
6
Supplementary figure 2. Forest plots of hazard ratios (HRs) and 95% confidence intervals (95%
CI) for each series in the poor prognosis versus good prognosis group by the 70-gene signature.
Squares = HRs; Lines = 95% CIs; Diamond = weighted total HR and 95% CI.
A. Distant metastasis-free survival at 10 years.
B. Breast cancer-specific survival at 10 years.
NEJM = 295 series17
; TRANSBIG = TRANSBIG series18
; RASTER = RASTER series23
; JBM validation= Bueno de Mesquita validation series19; LN 1-3 = Mook validation series 121; OVER 55 = Mook
validation series 222; TAM ADJ = Kok series24.
Study or Subgroup
1. NEJM
2. TRANSBIG3. RASTER
4. JBM validation
5. LN 1-3
6. OVER 55
7. TAM ADJ
Total (95% CI)
Heterogeneity: Chi² = 6.18, df = 6 (P = 0.40); I² = 3%
Test for overall effect: Z = 4.95 (P < 0.00001)
IV, Fixed, 95% CI
4.28 [1.97, 9.30]
2.63 [1.18, 5.87]1.44 [0.20, 10.22]
2.74 [0.89, 8.39]
6.56 [1.47, 29.32]
0.90 [0.24, 3.39]
1.99 [0.81, 4.90]
2.69 [1.82, 3.98]
Hazard Ratio Hazard Ratio
IV, Fixed, 95% CI
0.05 0.2 1 5 20
Good prognosissignature better
Poor prognosissignature better
Study or Subgroup
1. NEJM
2. TRANSBIG
3. RASTER
4. JBM validation
5. LN 1-3
6. OVER 55
7. TAM ADJ
Total (95% CI)
Heterogeneity: Chi² = 5.99, df = 6 (P = 0.42); I² = 0%Test for overall effect: Z = 5.29 (P < 0.00001)
IV, Fixed, 95% CI
13.93 [3.31, 58.60]
3.52 [1.53, 8.10]
84.61 [0.00, 988383129.70]
2.84 [0.83, 9.74]
11.03 [1.41, 86.23]
1.84 [0.41, 8.22]
2.59 [0.94, 7.17]
3.71 [2.28, 6.03]
Hazard Ratio Hazard Ratio
IV, Fixed, 95% CI
0.05 0.2 1 5 20Good prognosissignature better
Poor prognosissignature better
A
B

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 104/248
Chapter 6
114
Supplementary figure 3. Kaplan-Meier curves and univariate hazard ratio (HR) by 70-gene
prognosis-signature for patients who did not receive adjuvant systemic therapy (n=552).
A. Distant metastasis-free survival.
B. Breast cancer-specific survival.
Time (years)
1086420
D i s t a n t m e t a s t a s e s - f r e e s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
357
195
301
84177 145 131 103
200 171 140 117
Poor prognosis-signature
Good prognosis-signatureNumbers at
risk
Log-rank p < 0.001
96%
78%
86%
70%
HR at 10 yrs: 2.90 (95% CI 1.83-4.79); p < 0.001
1086420
B r e a s t c a n c e r - s p e c i fi c s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
357
195
304
88187 158 140 111
204 178 154 124
Poor prognosis-signature
Good prognosis-signatureNumbers at
risk
Time (years)
Log-rank p < 0.001
99%
85%
69%
91%
HR at 10 yrs: 4.67 (95% CI 2.67-8.18); p < 0.001
A
B

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 105/248
The 70-gene signature in pT1 breast cancer
115
6
Supplementary figure 4. Kaplan-Meier curves and univariate hazard ratio (HR) by grade 1/2
versus grade 3 (n=954, tumor grade was missing for 10 patients).
A. Distant metastasis-free survival.
B. Breast cancer-specific survival.
Time (years)
1086420
D i s t a n t m e t a s t a s e s - f r e e s u r v i v a
l
1.0
0.8
0.6
0.4
0.2
0.0
692
262
608
71222 145 121 97
442 380 300 208
Grade 3
Grade 1/2Numbers at
risk
Log-rank p < 0.001
92%
78%
84%
71%
HR at 10 yrs: 2.24 (95% CI 1.54-3.08); p < 0.001
1086420
B r e a s t c a n c e r - s p e c i fi c
s u r v i v a l
1.0
0.8
0.6
0.4
0.2
0.0
692
262
616
75234 162 132 102
456 397 324 221
Grade 3
Grade 1/2Numbers at
risk
Time (years)
Log-rank p < 0.001
97%
85%
72%
86%
HR at 10 yrs: 2.56 (95% CI 1.75-3.74); p < 0.001
A
B

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 106/248
Chapter 7
The predictive value of the 70-gene
signature for adjuvant chemotherapy in
early breast cancer
Michael Knauer
Stella Mook
Emiel J.T. Rutgers
Richard A. Bender
Michael Hauptmann
Marc J. Van de Vijver
Rutger H. Koornstra
Jolien M. Bueno de MesquitaSabine C. Linn
Laura J. Van ‘t Veer
Breast Cancer Res Treat 2010; 120: 655-661

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 107/248
Chapter 7
118
Abstract
Multigene assays have been developed and validated to determine the prognosis of
breast cancer. In this study, we assessed the additional predictive value of the 70-gene
MammaPrint™ signature for chemotherapy (CT) benefit in addition to endocrine therapy
(ET) from pooled study series. For 541 patients who received either ET (n = 315) or ET + CT
(n = 226), breast cancer-specific survival (BCSS) and distant disease-free survival (DDFS) at
5 years were assessed separately for the 70-gene high and low risk groups. The 70-gene
signature classified 252 patients (47%) as low risk and 289 (53%) as high risk. Within the
70-gene low risk group, BCSS was 97% for the ET group and 99% for the ET + CT group at 5
years with a non-significant univariate hazard ratio (HR) of 0.58 (95% CI 0.07–4.98; P = 0.62).
In the 70-gene high risk group, BCSS was 81% (ET group) and 94% (ET + CT group) at 5 years
with a significant HR of 0.21 (95% CI 0.07–0.59; P < 0.01). DDFS was 93% (ET) versus 99% (ET
+ CT), respectively, in the 70-gene low risk group, HR 0.26 (95% CI 0.03–2.02; P = 0.20). In
the high risk group DDFS was 76 versus 88%, HR of 0.35 (95% CI 0.17–0.71; P < 0.01). Results
were similar in multivariate analysis, showing significant survival benefit by adding CT in
the 70-gene high risk group. A significant and clinically meaningful benefit was observed
by adding chemotherapy to endocrine treatment in 70-gene high risk patients. This benefit
was not significant in low risk patients, who were at such low risk for recurrence and cancer-
related death, that adding CT does not appear to be clinically meaningful.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 108/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 109/248
Chapter 7
120
Patients and methods
Patients
A pooled database from seven previously reported studies, including 1637 patients with
known adjuvant treatment status (1637/1696, 97%) was developed. Patients who met the
following criteria were selected: unilateral stage pT1-3, N0-1, M0 invasive breast carcinoma
diagnosed between 1984 and 2006, surgical treatment with either breast-conserving
therapy or mastectomy with sentinel node biopsy or axillary lymph node dissection
followed by radiotherapy, if indicated.15 For this analysis, disease was staged according
to the 2002 UICC TNM-classification, 6th edition. All involved studies had been approved
by the respective institutional review boards. We evaluated all patients who had received
either ET alone or ET plus adjuvant CT (ET + CT). In the whole patient population, 90%
of patients were estrogen receptor (ER) positive and 69% of the study patients were
progesterone receptor (PR) positive. The studies by Van de Vijver et al.,6 Bueno de Mesquita
et al.,14,16 Mook et al.,17,18 and Kok et al. (personal communication) were included, resulting
in the inclusion of 30, 182, 29, 154, 27 and 119 patients from the database, respectively.
Differences in adjuvant CT benefit (CMF or anthracycline +/- taxane regimens) within
the 70-gene low risk and high risk patients were assessed. Of 226 patients treated with
adjuvant CT, 11 patients received CMF, 21 patients received taxane containing regimens,
and the vast majority of 194 patients received different anthracycline-containing regimens.
Time-to-event analyses using updated and centrally verified individual patient data wereperformed using a pooled database (Microsoft Access; Microsoft, Redmond, WA).
Microarray analysis
Frozen tumor samples from each patient were processed at Agendia’s laboratory
(Amsterdam, The Netherlands), for RNA isolation, amplification, and labeling as previously
described.5,19 Samples were eligible for RNA isolation, if they contained at least 30% tumor
cells on hematoxylin/eosin stained sections. To assess the mRNA expression level of the
70 genes, RNA was hybridized to a custom-designed array (MammaPrint™) at Agendia’sISO17025-certified, CLIA accredited, and FDA-cleared laboratory. Tumors were classified
as having a 70-gene high or low risk-signature at the time of initial series as described
previously, and were blinded to clinical data.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 110/248
Predictive value of the 70-gene signature
121
7
Statistical analyses
The endpoints evaluated were breast cancer-specific survival (BCSS), defined as time from
surgery to breast cancer-related death and distant disease-free survival (DDFS), defined as
time from surgery to any distant metastasis. For both outcomes, follow-up was censored
at 5 years, because firstly, most of the treatment effect of adjuvant CT is observed within 5
years and secondly to control for differences in median follow-up of the included studies.
Kaplan–Meier survival plots and log-rank tests were used to assess differences in BCSS
and DDFS for the 70-gene profile low and high risk groups. All P -values were two-sided
and considered statistically significant if less than 0.05. Adjusted uni- and multivariate
hazard ratios (HRs) and corresponding 95% confidence intervals (95% CIs) were derived
from Cox proportional hazards models. Co-variates used in adjusted models included age
at diagnosis, tumor size, number of positive lymph nodes, histological grade, ER and PR
status, hormonal therapy, and CT. Relative differences between treatment effects by 70-
gene risk groups were assessed by adding an interaction term to the model. All statistical
analyses were performed with SPSS 15.0 for Windows (SPSS Inc., Chicago, IL) and SAS 9.1
(SAS Institute Inc., Cary, NC).
Results
Five-hundred-forty-one patients with 0–3 positive lymph nodes from the pooled databasewere either treated with ET only or endocrine plus CT and, thus, met the inclusion criteria
for this study. The median follow-up for the study population was 7.1 years (range 0.1–25.2).
At 5 years of follow-up, 52 patients had developed distant metastases and 33 patients had
died of their disease. The 70-gene MammaPrint™ signature classified 252 patients (47%)
as low risk and 289 (53%) as high risk. Detailed patient characteristics are shown in Table 1.
Prognostic value of the 70-gene signature
BCSS and DDFS were significantly better in the 70-gene signature low risk group. The5-year BCSS probabilities were 97% for the low risk group and 87% for the high risk-
signature group, with a univariate HR of 4.81 (95% CI 1.98–11.67; P < 0.01). The probability
of remaining free of distant metastases at 5 years was 95% for the low risk-signature group
and 82% for the high risk-signature group with a univariate HR of 3.88 (95% CI 1.99–7.58;
P < 0.01).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 111/248
Chapter 7
122
Table 1. Summary of clinico-pathological characteristics of the study population.
Patients (n = 541) Characteristics n (%)
Age ≤ 50 years 231 (43%)
> 50 years 310 (57%)
Tumor size T1 279 (52%)
T2 254 (47%)
T3 7 (1%)
n.a. 1 (0.2%)
Lymph node status N0 265 (49%)
N1 276 (51%)
Histological grade Grade 1 134 (25%)
Grade 2 233 (43%)
Grade 3 163 (30%)
n.a. 11 (2%)
Estrogen receptor status Positive (≥ 10%) 484 (90%)
Progesterone receptor status Positive (≥ 10%) 371 (69%)
Her2-status Positive 59 (11%)
Adjuvant treatment ET only 315 (58%)
ET + CT 226 (42%)
70-gene MammaPrint signature Low risk 252 (47%)
High risk 289 (53%)
Abbreviations: n, number; n.a., not available; ET, endocrine therapy; CT, chemotherapy.
Adjuvant CT benefit for the 70-gene signature risk groups
In order to determine the predictive utility of the 70-gene signature, we assessed
differences in survival between patients who received either ET alone or ET combined withCT, separately within the 70-gene low risk and 70-gene high risk patient groups. Univariate
analysis demonstrated a significantly longer DDFS and BCSS in the 70-gene high risk group
for the patients receiving both CT and endocrine treatment, whereas such a significant
difference was not observed for the 70-gene low risk group. BCSS for the 70-gene low risk
group was 97% for the ET group and 99% for the ET + CT group, with a univariate HR of
0.58 (95% CI 0.07–4.98; P = 0.62). In the 70-gene high risk group, 5-year BCSS was 81% for
the ET group and 94% for the ET + CT group with a HR of 0.21 (95% CI 0.07–0.59, P < 0.01).
The corresponding Kaplan–Meier survival curves are shown in Figure 1A (BCSS) and for DDFS
in Figure 1B. In the 70-gene low risk group, DDFS probabilities at 5-years for the ET and the

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 112/248
Predictive value of the 70-gene signature
123
7
ET + CT groups were 93 versus 99%, respectively, with a HR of 0.26 (95% CI 0.03–2.02; P =
0.20). In the high risk group, survival was 76 versus 88% for the ET and the ET + CT groups,
respectively, with a HR of 0.35 (95% CI 0.17–0.71; P < 0.01).
Figure 1. A. Five-year breast cancer-specific survival by treatment within the 70-gene signature
groups (70-gene low risk on the left, high risk on the right).B. Five-year distant disease-free survival by treatment within the 70-gene signature groups (70-
gene low risk on the left, high risk on the right).
Abbreviations: BCSS, breast cancer-specific survival; DDFS, distant disease-free survival; n,
number; ET, endocrine therapy; ET + CT, endocrine + chemotherapy; HR, univariate hazard ratio.
To further evaluate treatment effects, we compared relative and absolute differences in
survival between patient groups receiving ET or ET + CT for both 70-gene risk groups. The
relative differences as determined by the interaction analysis resulted in a P -value of 0.45.
BCSS: M ammaPrint LOW RISK (n=252)
0 1 2 3 4 5
0
20
40
60
80
100
ET (n=174, 69%)
ET+CT (n=78, 31%)
99%
97%
HR = 0.58 (95% CI 0.07-4.98)
p = 0.62
Time (years)
P e r c e n t s u r v i v a l
BCSS: M ammaPrint HIGH RISK (n=289)
0 1 2 3 4 5
0
20
40
60
80
100
ET (n=141, 49%)
ET+CT (n=148, 51%)
94%
81%
HR = 0.21 (95% CI 0.07-0.59)
p < 0.01
Time (years)
P e r c e n t s u r v i v a l
DDFS: M ammaPrint LOW RISK (n=252)
0 1 2 3 4 5
0
20
40
60
80
100
ET (n=174, 69%)
ET+CT (n=78, 31%)
99%
93%
HR = 0.26 (95% CI 0.03-2.02)
p = 0.20
Time (years)
P e r c e n t s u r v i v a l
DDFS: MammaPrint HIGH RISK (n=289)
0 1 2 3 4 5
0
20
40
60
80
100
ET (n=141, 49%)
ET+CT (n=148, 51%)
88%
76%
HR = 0.35 (95% CI 0.17-0.71)
p < 0.01
Time (years)
P e r c e n t s u
r v i v a l
A
B

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 113/248
Chapter 7
124
In absolute numbers, the addition of CT for patients in the 70-gene low risk group could
prevent 3 events per 1000 patient years, resulting in a number needed to treat (NNT) of
333 (95% CI 78 harm to 83 benefit, i.e., there is similar chance that adding CT may result
in benefit or harm for this patient group). Adding CT for patients in the 70-gene high risk
group could prevent 33 events per 1000 patient years, resulting in a NNT of 30 (95% CI 19
benefit to 64 benefit).
In multivariate Cox regression analysis adjusted for age, tumor size, number of positive
lymph nodes, grade, ER and PR status, and HER2-expression, the results were similar to the
univariate results, indicating significant benefit in survival for adding CT in the high risk
group (P = 0.02). Details of the multivariate analysis for BCSS are shown separately for the
70-gene high risk and low risk patient groups in Table 2.
Table 2. Multivariate analysis of treatment effects for several prognostic factors. BCSS for the 70-
gene high risk patients is shown above and for the 70-gene low risk patients below.
MammaPrint HR (95% CI) P -value
High risk
Age at diagnosis (by year) 0.96 (0.91–1.02) 0.17
Tumor size (by cm) 1.05 (1.01–1.09) 0.02
No. of positive nodes (0-3) 1.39 (0.95–2.03) 0.09
Grade 1.03 (0.48–2.19) 0.94
ER-positive status 0.48 (0.18–1.34) 0.16
PR-positive status 0.31 (0.09–1.03) 0.06
HER2-positive status 0.72 (0.25–2.10) 0.55
Adjuvant therapy: ET versus ET + CT 0.21 (0.06–0.80) 0.02
Low risk
Age at diagnosis (by year) 1.00 (0.88–1.15) 0.95
Tumor size (by cm) 0.98 (0.89–1.10) 0.77
No. of positive nodes (0-3) 1.09 (0.37–3.16) 0.88
Grade 0.57 (0.12–2.82) 0.49ER-positive status ∞ (0–∞) 0.99
PR-positive status 0.09 (0.01–0.90) 0.04
HER2-positive status ∞ (0–∞) 0.99
Adjuvant therapy: ET versus ET + CT ∞ (0–∞) 0.98
Abbreviations: BCSS, breast cancer-specific survival; HR, hazard ratio; 95% CI, 95% confidence interval;
cm, centimeter; no, number; ER, estrogen receptor; PR, progesterone receptor; ET, endocrine therapy; CT,
chemotherapy.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 114/248
Predictive value of the 70-gene signature
125
7
Discussion
This is the first study assessing the prediction of adjuvant CT benefit using the 70-gene
MammaPrint™ signature in a pooled analysis of lymph node negative and positive
patients. When grouped by chemo-ET or ET alone, patients in the 70-gene low risk group
derive no significant survival benefit from CT added to ET. Of note, very few events were
observed in this 70-gene low risk patient group, irrespective of type of adjuvant treatment,
confirming their overall good outcome. Indeed, for these patients, a low gene expression
result may indicate a sufficiently low risk of recurrence and cancer-related death at 5 years
to obviate any benefit of adjuvant CT. In contrast, a significant and clinically meaningful
benefit of combined chemo-ET was shown for the 70-gene high risk group. These observed
differences in benefit for the 70-gene low and high risk group were not significant for the
interaction test, comparing the differential in the extent of the benefit between 70-gene
low and high risk patients. Ioannidis et al. have previously indicated that an interaction is not
necessarily required for a predictive score to be useful in therapeutic decisions, especially
when absolute risk in the low risk group is so low that CT would not be recommended. 20
The results from a pooled analysis of individual patient data not only confirm the 70-gene
signature as a validated, independent prognostic tool, but also suggest the assay to be a
predictive tool for the expected benefit of adjuvant CT in patients with early breast cancer
and a high risk 70-gene profile.
One of the strengths of this study is its design using a pooled analysis of centrally reviewed
and updated individual patient data, representing a commonly accepted method of ameta-analysis.21 While this study was not done using retrospective analysis of phase III
clinical trial data, the patients studied represent an unselected early breast cancer cohort,
which can be seen in Table 1. Moreover, the included consecutive series were obtained
from prospectively collected frozen banked tumor material at several leading European
cancer centers. All patients with a cancer diagnosis were accessioned into the tumor banks
consecutively as they presented to the respective institutions. Clinical and pathological
data shown in Table 1 were centrally reviewed and blinded to the microarray analysis. One
of the clear limitations of this study next to limited patient numbers and differences in CT
regimens is its retrospective design. However, it will be several years before survival datafrom ongoing randomized controlled trials such as the MINDACT or TAILORx study22,23 will
be available.
The use of multigene assays such as the 70-gene profile and the 21-gene RS has increased
in recent years and these assays have impacted treatment decisions. In multiple validation
studies it has been demonstrated that the 70-gene signature adds independent prognostic
information to routine clinico-pathologic risk assessment.13,14,17 In a study of 427 breast
cancer patients from 16 community-based Dutch hospitals,16 discordances in risk
stratification between the 70-gene signature and treatment guidelines were noted in up to
41% of patients. This led to an adjustment of the adjuvant treatment regimen in two-third
of the study cohort.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 115/248
Chapter 7
126
Two studies have evaluated the predictive utility of the 21-gene RS with respect to CT
benefit. The advantage of this assay is its validation on tumor tissue from phase III trials
with uniform CT regimens, although only a subset was available for analysis. Within the
NSABP B20 study, the degree of benefit from adjuvant CT ranged from little in the low and
intermediate RS to 20% absolute benefit in the highest RS group.12 Of note, the control arm
of this study had been used for development of the 21-gene RS which may have resulted
in overinterpretation of the data.7,20 Ioannidis mentioned in his commentary that the poor
performance of the RS in the CT arm of NSABP B20 caused the significant treatment-RS
interaction effect. The second predictive study was done on samples from the Southwest
Oncology Group study S8814 (INT0100) in node positive patients and presented at the
2007 San Antonio Breast Cancer Symposium.24 No benefit in disease-free survival for the
patients with a low RS for added CAF CT concurrent with tamoxifen was shown, whereas
the benefit was significant in the highest RS group.
In the neoadjuvant setting a number of studies using several drugs demonstrated the
predictive value of several gene signatures for CT response. These signatures comprise
known signatures such as the genomic grade index as well as several new classifiers.25-37
Additional data to support the predictive potential for the 70-gene assay comes from the
neoadjuvant study of Straver et al..38 In this study, only patients who had high risk profiles
were likely to achieve a pathologic complete response (pCR) to CMF or anthracycline-
containing CT regimens. In fact, no patient with a low risk profile achieved a pCR and only
two patients (9%) of this group achieved a partial response to therapy compared to 37%
overall response (P = 0.008) in the high risk group including a 20% pCR rate (P = 0.015). Theresults of all these studies support the theory that gene expression profiles can separate
CT-responsive from poorly or non-responsive tumors.
Clinical implications
In about two-third of all hormone receptor-positive cases, clinical and genomic risk
assessment using the 70-gene signature will be concordant. If both methods indicate a
high risk of recurrence, the use of combined chemo-ET seems clinically indicated. If both
methods indicate a low risk of recurrence, then ET alone should be adequate treatment.For the one-third of patients with discordant risk assessment, our findings suggest
consideration of the following approach. If the 70-gene profile indicates a low risk in a
clinically stratified high risk patient, ET alone may be indicated in highly endocrine-
responsive patients, as defined by the St. Gallen consensus panel, as these patients are at
very low risk to recur and will likely gain little or no benefit from additional CT. Conversely,
70-gene high risk and clinically assessed low risk patients will likely benefit from combined
chemo-endocrine treatment. If these patients are highly endocrine-responsive, then
endocrine treatment alone might be the prudent option, however, withholding adjuvant
therapy might not be a prudent option for this group of patients. Furthermore, other

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 116/248
Predictive value of the 70-gene signature
127
7
factors such as age and co-morbidities may influence shared decision-making for adjuvant
systemic therapy. However, generally definitive recommendations cannot be drawn from
retrospective studies and only the ongoing, well designed prospective trials will provide
definitive answers to this important question.
Conclusions
In this study, a statistically significant and clinically meaningful benefit for the addition of
adjuvant CT to endocrine treatment in 70-gene high risk patients in the adjuvant setting
has been shown. There appears to be no evidence for a similar benefit for the 70-gene
low risk patients and these patients are at such a low risk of recurrence and cancer-related
death, that addition of CT may not be justified. ET alone seems to be the optimal treatment
for this group of patients. It seems reasonable to use multigene assays whenever indicated
in hormone receptor-positive patients for improved decision-making regarding the role of
adding adjuvant CT to hormonal treatment.
Acknowledgments
This work was supported by the Austrian Society of Surgery and Agendia BV. Both provided
unrestricted educational grants for the work of M. Knauer. We are indebted to Femke de
Snoo, MD PhD for critically reading the manuscript and providing helpful comments and
to Marleen Kok for providing part of the data used for our analyses.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 117/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 118/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 119/248
Chapter 7
130
36. Potti A, Dressman HK, Bild A, et al. Genomic signatures to guide the use of chemotherapeutics. Nat Med
2006; 12: 1294-1300.
37. Thuerigen O, Schneeweiss A, Toedt G, et al. Gene expression signature predicting pathologic complete
response with gemcitabine, epirubicin, and docetaxel in primary breast cancer. J Clin Oncol 2006; 24: 1839-
1845.
38. Straver ME, Glas AM, Hannemann J, et al. The 70-gene signature as a response predictor for neoadjuvant
chemotherapy in breast cancer. Breast Cancer Res Treat 2010; 119: 551-558.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 120/248
Chapter 8
Calibration and discriminatory accuracy
of prognosis calculation for breast cancer
with the online Adjuvant! program: a
hospital-based retrospective cohort study
Stella Mook*
Marjanka K. Schmidt*
Emiel J.Th. Rutgers
Anthonie O. van de Velde
Otto Visser
Sterre M. Rutgers
Nicola Armstrong
Laura J. Van ’t VeerPeter M. Ravdin
* Contributed equally
Lancet Oncol 2009; 10: 1070-1076.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 121/248
Chapter 8
134
Summary
Background
Adjuvant! is a web-based program that calculates individualized 10-year survival
probabilities and predicted benefit of adjuvant systemic therapy. The Adjuvant! model
has not been validated in any large European series. The aim of our study was to validate
Adjuvant! in Dutch patients, investigating both its calibration and discriminatory accuracy.
Methods
Patients who were at least partly treated at the Netherlands Cancer Institute for breast
cancer between 1987 and 1998 were included if they met the following criteria: tumor size
T1 (≤2 cm), T2 (2–5 cm), or T3 (>5 cm), invasive breast carcinoma, with information about
involvement of axillary lymph nodes available, no distant metastases, primary surgery,
axillary staging, and radiotherapy according to national guidelines. Clinicopathological
characteristics and adjuvant treatment data were retrieved from hospital records and
medical registries and were entered into the Adjuvant! (version 8.0) batch processor with
blinding to outcome. Endpoints were overall survival and the proportion of patients that
did not die from breast cancer (breast cancer-specific survival [BCSS]).
Findings
5380 patients were included with median follow-up of 11.7 years (range 0.03-21.8). the
10-year observed overall survival (69.0%) and BCSS (78.6%) and Adjuvant! predicted
overall survival (69.1%) and BCSS (77.8%) were not statistically different ( p = 0.87 and p =
0.18, respectively). Moreover, differences between predicted and observed outcomes were
within 2% for most relevant clinicopathological subgroups. In patients younger than 40
years, Adjuvant! overestimated overall survival by 4.2% ( p = 0.04) and BCSS by 4.7% ( p =
0.01). The concordance index, which indicates discriminatory accuracy at the individual
level, was 0.71 for BCSS in the entire cohort.
Interpretation
Adjuvant! accurately predicted 10-year outcomes in this large-scale Dutch validation study
and is of use for adjuvant treatment decision making, although the results may be less
reliable in some subgroups.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 122/248
Dutch validation of Adjuvant!
135
8
Introduction
Treatment recommendations for early-stage breast cancer are based on prognosis (i.e., the
estimated risk of relapse and death after primary surgery and radiotherapy) and expected
benefit of adjuvant therapy. Treatment guidelines qualitatively incorporate prognosis
and treatment efficacy without quantitative estimates.1-3 Nevertheless, methods that give
quantitative estimates of prognosis exist, such as the Nottingham Prognostic Index and
Adjuvant!.4-6 These quantitative methods include several assumptions, the most crucial
being that the populations for which the models were developed are representative of
others.
Adjuvant! is a computer program that is freely accessible on the internet (www.
adjuvantonline.com). The program provides estimated 10-year survival probabilities and
risk of relapse on the basis of a model incorporating patient’s age, co-morbidity, tumor size,
tumor grade, estrogen-receptor status, and number of involved lymphnodes.6 the program
calculates the expected efficacy of adjuvant therapy (chemotherapy, hormonal therapy, or
both) for different classes of regimens.7-9 The program gives the estimated prognosis and
expected treatment benefit in a comprehensive format and can help to inform patients
and to involve them in decision making about therapeutic options.10-12
Adjuvant! was largely developed with information from the Surveillance, Epidemiology
and End Results (SEER) registry. The SEER registry has data for about 10% of patients with
breast cancer in the USA.6 Olivotto and colleagues13 validated Adjuvant! (version 5.0) in a
population-based series of 4083 early-stage patients with breast cancer registered in theBritish Columbia Breast Cancer Outcomes Unit database. They showed that the Adjuvant!
model was well calibrated - i.e., it accurately predicted the number of breast cancer-related
deaths observed in the whole study cohort and subsets of their population (predicted
and observed outcomes were within 2%). However, because European populations might
differ from those in the USA and Canada, whether outcome predictions of the Adjuvant!
model are applicable in Europe is unknown: differences in incidence of obesity, duration
and type of adjuvant and salvage treatment, ethnic background, and intrinsic tumor
characteristics might affect prognosis.14-19 Furthermore, although Olivotto and colleagues13
showed the goodness of fit of the Adjuvant! model, no information about its discriminatoryaccuracy was given. Because Adjuvant! is used in Europe and the USA to support treatment
decisions in clinical practice and randomized trials,20-22 we aimed to test the validity of
Adjuvant! in a large cohort of Dutch patients with breast cancer, determining its ability to
predict outcomes in groups of patients (calibration) and to distinguish individuals who will
experience different outcomes (discriminatory accuracy).23,24

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 123/248
Chapter 8
136
Methods
Patients
All women who were at least partly treated for breast cancer at the Netherlands Cancer
Institute at the Antoni van Leeuwenhoek Hospital (NKI-AVL) from 1987 to 1998 were
identified in the hospital’s Medical Registry. Patients were included if they had tumor
size T1 (≤2 cm), T2 (2–5 cm), or T3 (>5 cm), unilateral tumors, invasive breast carcinoma,
information about involvement of axillary lymph nodes available, no distant metastases,
primary surgery, axillary staging, and radiotherapy according to national guidelines.
Patients with previous malignant disease and those who received neoadjuvant therapy
were excluded, as were those with unknown tumor size, unknown nodal status, unknown
adjuvant systemic therapy, no definitive axillary surgery (axillary-lymph-node dissection
with fewer than six nodes examined; Figure 1). Information about adjuvant systemic
treatment was derived from the medical registry. Adjuvant treatment was given according
to national guidelines, taking into account patients’ wishes and preferences.17
The study is reported according to the STROBE statement.25 No ethical review was required
according to Dutch legislation.
Procedures
Histology, tumor size, tumor grade, and number of positive lymph nodes were retrievedfrom three sources and entered in the database according to the following hierarchy of
preference for data source: first, personal logbook from pathologists at NKI-AVL containing
pathology revisions of breast cancer diagnosed between 1994–96; second, the PALGA
system (Dutch network and National Database for Pathology); third, medical registry of
the NKI-AVL. Information about estrogen-receptor status was retrieved from three sources
and entered into a database according to the following hierarchy: first, estrogen-receptor
ligand-binding assays (breast cancers diagnosed 1987–95); second, Pathologist logbook
(breast cancers diagnosed 1995–96), and third the PALGA system (Dutch network and
National Database for Pathology; Supplements).Outcome data (date of first local, regional and distant recurrence, second malignancies,
contralateral breast cancer, and date of last follow-up or death) were obtained from the
medical registry. These data were completed by linking patient records to the Dutch
municipal registry, which contains the date of death or emigration if applicable, for all Dutch
citizens. For patients not in this national registry as having died or emigrated, the date of
last follow-up was recorded as Feb 1, 2007 (i.e., 2 months before the date of linkage). Cause
of death was retrieved from the medical registry if available and from individual patients’
files when no cause of death was entered in the registry (n=1090 breast cancer-specific
death; n=188 other causes). If neither the medical registry nor patients’ files contained

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 124/248
Dutch validation of Adjuvant!
137
8
cause of death, we used the presence of distant metastases as a surrogate: patients
without known cause of death (n=875) were assigned to breast cancer-specific mortality
if they were diagnosed with distant metastases during follow-up (n=191 breast cancer-
specific death; n=684 other causes). Patients with registered breast cancer-specific death
and patients who were assigned to breast cancer-specific death based on the presence of
distant metastases were pooled for analyses.
10-year predicted overall survival and breast cancer-specific survival (BCSS) were calculated
for each patient individually. Data on age, co-morbidity, tumor size, tumor grade, number
of positive axillary lymph-nodes, estrogen-receptor status, and adjuvant systemic
treatment were entered in the Adjuvant! (version 8.0) batch processor, with blinding to
patient outcomes. The model’s estimation of prognosis is based on 10-year observed
overall survival of women diagnosed with breast cancer between 1988 and 1992 in the
USA and recorded in the SEER database.6 The estimations of treatment efficacy are mainly
based on the proportional risk reductions derived from the Early Breast Cancer Trialists’
Collaborative Group 1998 meta-analyses and recently updated with the meta-analyses
data from 2005.7-9 Because we could not retrieve reliable data for co-morbidity, we used
the default assumption of minor health problems. For patients with no data on estrogen-
receptor status, the status was entered in the model as unknown.
Statistical analyses
Overall survival and BCSS were derived from Kaplan-Meier survival analyses of the entiregroup and various subsets.26 For the same datasets, the average predicted overall survival
and BCSS were calculated from individual predicted outcomes by Adjuvant!. To assess the
calibration of the model (goodness of fit), observed and average predicted outcomes were
compared by use of a one-sample t-test for proportions, assuming the Adjuvant! predicted
value to be the population value (under the assumption that the model is true) and thus
fixed. In addition, we plotted averages of observed versus predicted outcomes, grouped by
deciles of predicted outcomes.23 The slope of the fitted line was compared with the slope
of the line indicating a perfect relationship (y=x).
To assess discriminatory accuracy of Adjuvant! (its ability to discern patients havinggood outcomes from those having poor outcomes), we calculated an index of predictive
discrimination, the concordance index (c-index).23 The c-index was corrected for overfitting
by bootstrapping with 200 resamples each. A c-index of 1 means that the model perfectly
ranks patients according to survival (i.e., patients having a better outcome also having a
better predicted outcome), 0.5 means the model does no better than chance. the predictive
accuracy and proportion of explained variation, as defined by Schemper and colleagues,24
was also calculated. SEs were estimated by bootstrapping with 200 resamples each. Known
prognostic factors (i.e., age, tumor size, tumor grade, number of positive lymph-nodes,
histology, estrogen-receptor status, and adjuvant systemic therapy) were used in the Cox

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 125/248
Chapter 8
138
multivariate model. Furthermore, on the basis of backward multivariate Cox regression
analyses, year of diagnosis was added to construct the best predictive model for BCSS and
overall survival in our dataset.27 Analyses were done with SPSS version 15.0 and R statistical
software (www.r-project.org).
Role of the funding source
The funding sources had no role in study design; collection, analysis, or interpretation of
data; writing of the paper; or in decisions relating to publication. SM, MKS, and LVV had full
access to all data. SM, MKS, LVV, and PMR took final responsibility for the decision to submit
the paper for publication.
Results
Our database included 5380 patients, 2604 of whom (48%) received no adjuvant systemic
therapy. The algorithm in Adjuvant! attributes different efficacy estimates depending
on type of chemotherapy and hormonal treatment. Among 1961 patients treated with
endocrine therapy, 1908 (97%) received tamoxifen (2–5 years); therapy was not specified
for 13 (0.7%). 892 (82%) of 1084 patients treated with adjuvant chemotherapy received
cyclophosphamide, methotrexate, and fluorouracil, 122 (11%) received fluorouracil,
epirubicin, and cyclophosphamide, 42 (4%) received high-dose chemotherapy, and 11(1%) received cyclophosphamide and doxorubicin. For the remaining 16 patients (2%),
type of chemotherapy was unspecified. 2276 (42%) of 5380 patients had complete data for
all factors used in the Adjuvant! model to predict outcome. Grade was unknown for 1379
patients (26%), and estrogen-receptor status unknown for 2253 (42%).
During a median follow-up of 11.7 years (range 0.03–21.8), 2153 (40%) of 5380 patients
died; 3032 (94%) of 3227 patients alive at last follow-up had 10 years or more follow-up
(Figure 1). Table 1 shows the distribution of demographic, pathological, and primary treatment
data for our study cohort. For all patients, the 10-year observed overall survival (69 .0%)
and BCSS (78.6%) rates as compared with the 10-year overall survival (69.1%) and BCSS(77.8%) rates predicted by Adjuvant! were within 1% and not significantly different ( p >0.05;
Table 1). In general, Adjuvant! predicted overall survival accurately in the various subsets
of patients (i.e., differences between predicted and observed outcomes were within 2%),
whereas Adjuvant! underestimated BCSS in some subsets (Table 1). Subsets of patients for
whom there was a discrepancy between predicted outcomes by Adjuvant! and actual
observed outcomes included patients under 40 years, for whom both predicted overall
survival and BCSS were overly optimistic (4.2% and 4.7%, respectively; p = 0.04 and p = 0.01).
For patients older than 69 years the program also overestimated overall survival by 3 .4%
( p = 0.05), but BCSS was accurately predicted in this group (predicted–observed –1.7%).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 126/248
Dutch validation of Adjuvant!
139
8
In subgroups of nodal status, overall survival was accurately predicted by Adjuvant!;
however, the program underestimated BCSS by 3.1% ( p = 0.002) in patients with one to
three positive lymph-nodes.
Although Adjuvant! predicted overall survival accurately for subsets of tumor size, a
discrepancy between predicted and observed BCSS was noted (–5.8% to 2.4%; Table 1). In
particular, predicted BCSS was optimistic for patients with tumors with diameter 11–20
mm, although it was pessimistic in patients with tumors 21–50 mm in diameter. In patients
with estrogen-receptor-negative tumors Adjuvant! underestimated BCSS by 4.1% ( p = 0.02).
This underestimation of outcome by Adjuvant!, although non-significant, was also seen for
overall survival (–3.2%, p = 0.07).
Figure 1. Study profile
5761 patients in tumor registry
5380 patients included in analysis
381 excluded:
− 168 no information on tumor size
− 34 no information on lymph-node status
− 116 N0, fewer than six lymph nodes examined
− 62 N+, fewer than six lymph nodes examined
− 1 no information about adjuvant systemic therapy
3227 alive 2153 dead
1281 breast cancer-specific death 872 other cause death

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 127/248
Chapter 8
140
T a b
l e 1 . B a s e l i n e c h a r a c t e r i s t i c s a n d A d j u v a n t ! p r e d i c t e d v e r s u s o b s e r v e d o v e r a l l s u r v i v a l a n d b r e a s t c
a n c e r - s p e c i fi c s u r v i v a l .
P a t i e n t s
O v e r a l l s u r v i v a l
B r e a s t c a n c e r -
s p e c i fi c s u r v i v a l
N o .
%
A d j u v a n t !
P r e d i c t e d
O b s e r v e d
( S E )
P r
e d i c t e d - O b s e r v e d
( 9 5 % C
I )
P
v a l u e
A d j u v a n t !
P r e
d i c t e d
O b s e r v e d
( S E )
P r e d i c t e d - O b s e r v e d
9 5 % C
I
P
v a l u e
A l l p a t i e n t s
5 3 8 0
1 0 0
6 9 . 1
6 9 ( 0 . 6 )
0 . 1 ( - 1 . 0 8 t o 1 . 2 8 )
0 . 8 7
7 7 . 8
7 8 . 6 ( 0 . 6 )
- 0 . 8 ( - 1 . 9 8 t o 0 . 3 8 )
0 . 1 8
Y e a r o f d i a g n o s i s
1 9 8 7 - 1 9 8 9
1 1 6 9
2 1 . 7
6 7 . 6
6 7 . 7 ( 1 . 4 )
- 0 . 1 ( - 2 . 8 5 t o 2 . 6 5 )
0 . 9 4
7 6 . 4
7 7 . 0 ( 1 . 3 )
- 0 . 6 ( - 3 . 1 5 t
o 1 . 9 5 )
0 . 6 4
1 9 9 0 - 1 9 9 3
2 0 1 7
3 7 . 5
6 9 . 2
6 7 . 8 ( 1 . 0 )
1 . 4 ( - 0 . 5 6 t o 3 . 3 6 )
0 . 1 6
7 8 . 1
7 7 . 7 ( 1 . 0 )
0 . 4 ( - 1 . 5 6 t
o 2 . 3 6 )
0 . 6 9
1 9 9 4 - 1 9 9 7
2 1 9 4
4 0 . 8
6 9 . 8
7 0 . 8 ( 1 . 0 )
- 1 . 0 ( - 2 . 9 6 t o 0 . 9 6 )
0 . 3 2
7 8 . 4
8 0 . 3 ( 0 . 9 )
- 1 . 9 ( - 3 . 6 7 t o - 0 . 1 4 )
0 . 0 4
T y p e o f s u r g e r y
B r e a s t - c o n s e r v i n g s u r g e r y
2 8 8 5
5 3 . 6
7 6 . 5
7 6 ( 0 . 8 )
0 . 5 ( - 1 . 0 7 t o 2 . 0 7 )
0 . 5 3
8 3 . 8
8 2 . 8 ( 0 . 7 )
1 . 0 ( - 0 . 3 7 t
o 2 . 7 3 )
0 . 1 5
M a s t e c t o m y
1 9 7 8
3 6 . 8
5 9 . 1
6 0 ( 1 . 1 )
- 0 . 9 ( - 3 . 0 6 t o 1 . 2 6 )
0 . 4 1
6 9 . 7
7 2 . 6 ( 1 . 0 )
- 2 . 9 ( - 4 . 8 6 t o - 0 . 9 4 )
0 . 0 0 4
U n k n o w n
5 1 7
9 . 6
6 6 . 1
6 4 . 3 ( 2 . 1 )
1 . 8 ( - 2 . 3 3 t o 5 . 7 3 )
0 . 3 9
7 5 . 7
7 7 . 7 ( 1 . 9 )
- 2 . 0 ( - 5 . 7 3 t
o 1 . 7 3 )
0 . 2 9
A g
e ( y e a r s )
< 4 0
5 7 2
1 0 . 6
7 2 . 4
6 8 . 2 ( 2 . 0 )
4 . 2 ( 0 . 2 7 t o 8 . 1 3 )
0 . 0 4
7 3 . 5
6 8 . 8 ( 1 . 9 )
4 . 7 ( 0 . 9 7 t
o 8 . 4 3 )
0 . 0 1
4 0 - 4 9
1 4 4 8
2 6 . 9
7 6 . 6
7 8 . 6 ( 1 . 1 )
- 2 . 0 ( - 4 . 1 6 t o 0 . 1 6 )
0 . 0 7
7 8 . 8
8 1 . 2 ( 1 . 0 )
- 2 . 4 ( - 4 . 3 6 t o - 0 . 4 4 )
0 . 0 2
5 0 - 5 9
1 3 6 9
2 5 . 4
7 2 . 0
7 3 . 6 ( 1 . 2 )
- 1 . 6 ( - 3 . 9 5 t o 0 . 7 5 )
0 . 1 8
7 6 . 8
7 7 . 7 ( 1 . 1 )
- 0 . 9 ( - 3 . 0 6 t
o 1 . 2 6 )
0 . 4 1
6 0 - 6 9
1 1 7 4
2 1 . 8
6 8 . 9
6 8 . 3 ( 1 . 4 )
0 . 6 ( - 2 . 1 5 t o 3 . 3 5 )
0 . 6 7
8 0 . 1
8 0 . 9 ( 1 . 2 )
- 0 . 8 ( - 3 . 1 5 t
o 1 . 5 5 )
0 . 5 1
≥ 7 0
8 1 7
1 5 . 2
4 9 . 1
4 5 . 7 ( 1 . 7 )
3 . 4 ( 0 . 0 6 t o 6 . 7 4 )
0 . 0 5
7 7 . 8
7 9 . 5 ( 1 . 6 )
- 1 . 7 ( - 4 . 8 4 t
o 1 . 4 4 )
0 . 2 9
H i s t o l o g y
M a i n l y D C I S
5 5
1 . 0
8 3 . 8
8 7 . 2 ( 4 . 5 )
- 3 . 4 ( - 1 2 . 4 2 t o 5 . 6 2 )
0 . 4 5
9 0 . 2
9 6 . 2 ( 2 . 6 )
- 6 . 0 ( - 1 1 . 2 1 t o - 0 . 7 9 )
0 . 0 3
I D C
4 0 0 1
7 4 . 4
6 8 . 7
6 8 . 3 ( 0 . 7 )
0 . 4 ( - 0 . 9 7 t o 1 . 7 7 )
0 . 5 7
7 7 . 2
7 7 . 6 ( 0 . 7 )
- 0 . 4 ( - 1 . 7 7 t
o 0 . 9 7 )
0 . 5 7
I L C
6 1 4
1 1 . 4
6 5 . 3
6 6 . 2 ( 1 . 9 )
- 0 . 9 ( - 4 . 6 3 t o 2 . 8 3 )
0 . 6 4
7 5 . 6
7 7 . 8 ( 1 . 7 )
- 2 . 2 ( - 5 . 5 4 t
o 1 . 1 4 )
0 . 2 0
I D / L C
3 1 8
5 . 9
7 0 . 4
7 0 . 1 ( 2 . 6 )
0 . 3 ( - 4 . 8 2 t o 5 . 4 2 )
0 . 9 1
7 8 . 5
7 8 . 5 ( 2 . 4 )
0 . 0 ( - 4 . 7 2 t
o 4 . 7 2 )
1 . 0 0
T u b u l a r
1 1 4
2 . 1
8 8 . 8
9 5 . 6 ( 1 . 9 )
- 6 . 8 ( - 1 0 . 5 6 t o - 3 . 0 4 )
0 . 0 0 0 5
9 5 . 2
1 0 0 ( 0 . 0 )
- 4 . 8 ( - 4 . 8 0 t o - 4 . 7 9 ) < 0 . 0 0 0 1
M u c i n o u s
7 6
1 . 4
7 4 . 0
6 5 . 6 ( 5 . 5 )
8 . 4 ( - 2 . 5 6 t o 1 9 . 3 6 )
0 . 1 3
8 7 . 6
8 8 . 1 ( 4 . 0 )
- 0 . 5 ( - 8 . 4 7 t
o 7 . 4 7 )
0 . 9 0
M e d u l a r
6 8
1 . 3
7 4 . 5
8 0 . 9 ( 4 . 8 )
- 6 . 4 ( - 1 5 . 9 8 t o 3 . 1 8 )
0 . 1 9
7 9 . 4
8 6 . 4 ( 4 . 2 )
- 7 . 0 ( - 1 5 . 3 8 t
o 1 . 3 8 )
0 . 1 0
O t h e r s
1 3 4
2 . 5
6 7 . 5
6 4 . 1 ( 4 . 2 )
3 . 4 ( - 4 . 9 1 t o 1 1 . 7 1 )
0 . 4 2
7 8 . 8
7 6 . 7 ( 3 . 8 )
2 . 1 ( - 5 . 4 2 t
o 9 . 6 2 )
0 . 5 8

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 128/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 129/248
Chapter 8
142
P a t i e n t s
O v e r a l l s u r v i v a l
B r e a s t c a n c e r -
s p e c i fi c s u r v i v a l
N o .
%
A d j u v a n t !
P r e d i c t e d
O b s e r v e d
( S E )
P r
e d i c t e d - O b s e r v e d
( 9 5 % C
I )
P
v a l u e
A d j u v a n t !
P r e
d i c t e d
O b s e r v e d
( S E )
P r e d i c t e d - O b s e r v e d
9 5 % C
I
P
v a l u e
S y s t e m i c t r e a t m e n t
N o n e
2 6 0 4
4 8 . 4
7 6 . 8
7 5 . 8 ( 0 . 8 )
1 . 0 ( - 0 . 5 7 t o 2 . 5 7 )
0 . 2 1
8 5 . 3
8 4 . 6 ( 0 . 7 )
0 . 7 ( - 0 . 6 7 t o 2 . 0 7 )
0 . 3 2
C h e m o t h e r a p y o n l y
8 1 5
1 5 . 1
6 7 . 4
6 9 . 3 ( 1 . 6 )
- 1 . 9 ( - 5 . 0 4 t o 1 . 2 4 )
0 . 2 4
6 9 . 4
7 1 . 7 ( 1 . 6 )
- 2 . 3 ( - 5 . 4 4 t
o 0 . 8 4 )
0 . 1 5
H o r m o n a l t h e r a p y o n l y
1 6 9 2
3 1 . 4
5 8 . 8
5 8 . 4 ( 1 . 2 )
0 . 4 ( - 1 . 9 5 t o 2 . 7 5 )
0 . 7 4
7 2 . 1
7 3 . 7 ( 1 . 1 )
- 1 . 6 ( - 3 . 7 6 t
o 0 . 5 6 )
0 . 1 5
C h e m o a n d h o r m o n a l
t h e r a p y
2 6 9
5 . 0
6 4 . 5
6 9 . 1 ( 2 . 8 )
- 4 . 6 ( - 1 0 . 1 1 t o 0 . 9 1 )
0 . 1 0
6 7 . 0
7 1 . 4 ( 2 . 8 )
- 4 . 4 ( - 9 . 9 1 t
o 1 . 1 1 )
0 . 1 2
C o
m p l e t e n e s s o f d a t a
M i s s i n g e s t r o g e n - r e c e p t o r
s t a t u s a n d / o r g r a d e
3 1 0 4
5 7 . 7
6 9 . 0
6 8 . 7 ( 0 . 8 )
0 . 3 ( - 1 . 2 7 t o 1 . 8 7 )
0 . 7 1
7 7 . 8
7 8 . 9 ( 0 . 8 )
- 1 . 1 ( - 2 . 6 7 t
o 0 . 4 7 )
0 . 1 7
C o m p l e t e
2 2 7 6
4 2 . 3
6 9 . 2
6 9 . 4 ( 1 . 0 )
- 0 . 2 ( - 2 . 1 6 t o 1 . 7 6 )
0 . 8 4
7 7 . 8
7 8 . 2 ( 0 . 9 )
- 0 . 4 ( - 2 . 1 7 t
o 1 . 3 7 )
0 . 6 6
P - v a
l u e s c a l c u l a t e d w i t h o n e s a m p l e t - t e
s t .
T a b
l e 1 . C o n t i n u e d .

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 130/248
Dutch validation of Adjuvant!
143
8
Figure 2 shows the observed outcome versus the average predicted outcome for the cohort,
grouped by deciles of predicted overall survival or BCSS probabilities. The slope of the
line representing a perfect fit of predicted with observed outcomes (y=x) and the slope
of the actual line fitted to our data for overall survival was not significantly different. This
indicates that the calibration of Adjuvant! is similarly good in patients with poor overall
survival and patients with excellent overall survival. However, for BCSS, the model tended
to underestimate and to overestimate BCSS in the extremes of the distribution of poor and
good survival, respectively (slope was significantly different p < 0.0001).
To assess discriminatory accuracy of the model (i.e., its ability to separate patients who will
die from breast cancer from those who will not), we calculated Harrell’s c-index (0 .71 for
BCSS), as well as the predictive accuracy and explained variation (0 .73 and 13% for BCSS,
respectively). Hence, the predictive accuracy for BCSS increased from 0.69 for a model
without predictors to 0.73 for the Adjuvant! model (Table 2). In various clinical subgroups
(Table 1), the c-index varied from 0.65 to 0.75 (data not shown). The c-index for a multivariate
Cox regression model best fitted to the outcome of the 5380 patients with a backward
approach (model included age, tumor size, tumor grade, number of positive lymph
nodes, estrogen-receptor status, histology, type of adjuvant systemic therapy and year of
diagnosis) was similar to the Adjuvant! model (i.e., 0.72 and 0.71, respectively for BCSS).
Table 2. Discriminatory accuracy of Adjuvant! and a multivariate Cox model fitted to the
outcome.
Overall survival Breast cancer-specific survival
Adjuvant! Cox model* Adjuvant! Cox model*
C index 0.70 0.69 0.71 0.72
Predictive accuracy model without
predictors [1-D0]0.64 0.64 0.69 0.69
Predictive accuracy [1-Dx] (SE) 0.69 (0.008) 0.69 (0.007) 0.73 (0.02) 0.74 (0.02)
Explained variation [(Dx-D0)/D0] (SE) 15% (1%) 15% (1%) 13% (1%) 16% (2%)
For overall survival the model included age, tumor size, tumor grade, number of positive lymph-nodes,histology, adjuvant systemic therapy and year of diagnosis. For breast cancer-specific survival the model
included age, tumor size, tumor grade, number of positive lymph-nodes, histology, estrogen-receptor
status, adjuvant systemic therapy, and year of diagnosis.
C-index = Harrell’s concordance index. Dx = predictive accuracy of model with predictors. D0 = predictive
accuracy of model without predictors.
*Best-fitted multivariate Cox model.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 131/248
Chapter 8
144
Figure 2. Mean predicted versus observed outcomes by deciles of predicted outcome.
Error bars are SE.
Discussion
Overall projections of overall survival and BCSS with Adjuvant! were within 1% of observed
results and estimates within most subgroups seemed reasonably accurate (within 2% or
not significantly different from observed estimates). The conservative Dutch guidelines for
adjuvant systemic therapy used in the era of the study cohort results in a large proportion
of patients (2604 [48%] of 5380) who received no adjuvant systemic therapy. For this group
of patients, we could assess the prognostic value of Adjuvant! (i.e., the prediction of diseaseoutcome in the absence of adjuvant systemic therapy). Although most patients with early
breast cancer now receive some form of adjuvant systemic treatment, the confirmation
of the prognostic value is important for the decision whether or not to treat. Moreover,
when the program predicts prognosis accurately, the potential benefit of different types of
adjuvant treatment is also predicted more accurately, because the latter depends on the a
priori risk of recurrence. Adjuvant! is commonly used to decide whether patients who will
be treated with endocrine therapy are candidates for additional chemotherapy. Because
a small proportion of patients received chemotherapy with or without endocrine therapy
(815 [15%] and 269 [5%] of 5380, respectively) the prediction of chemotherapy benefit in
0
10
20
30
40
50
60
70
80
90
100
0 10 20 30 40 50 60 70 80 90 100
O b s e r v e d o u t c o m e
Predicted outcome
Overall survival (OS)
Breast cancer-specific survival (BCSS)
R2=0.996
Observed OS= 0.96 + 0.98*Predicted OS
R2=0.992
Observed BCSS= 12.23 + 0.85*Predicted BCSS

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 132/248
Dutch validation of Adjuvant!
145
8
addition to endocrine therapy is less robust. However, the decision to add chemotherapy
to the endocrine treatment regimen depends also on the predicted outcome of a patient
when treated with hormonal therapy only. Adding chemotherapy to endocrine therapy will
be more beneficial for patients who will have an a priori poorer predicted disease outcome.
Our results show that Adjuvant! predicted both overall survival and BCSS accurately in
patients treated with endocrine therapy (1692 [31%] of 5380).
One of the limitations of our study is that in the era of this study standard adjuvant
chemotherapy consisted of cyclophosphamide, methotrexate, and fluorouracil for six
cycles and standard adjuvant endocrine therapy consisted of tamoxifen for which we
evaluated Adjuvant!. Therefore, future studies are required to validate Adjuvant! predictions
of currently used therapies, such as taxane-based chemotherapy and aromatase inhibitors.
The largest discrepancy between subgroups between our study and the Canadian validation
study13 was in patients younger than 35 years (10% for BCSS). As a consequence of this
disagreement and after further review of the SEER registry data, Adjuvant! was modified to
give more pessimistic estimates for estrogen-receptor-positive patients under 35 years of
age. Even after this adjustment (the major difference between Adjuvant! 5.0and Adjuvant!
8.0), the predicted outcomes still seem too optimistic, albeit less so than in the original
validation study (by 5% for BCSS). When results were stratified for estrogen-receptor status
in patients younger than 35 years and age 35–40 years, the overestimation was exclusively
seen in patients with estrogen-receptor-positive tumors in both age groups (Supplements).
This suggests that the correction factor of 1.5 for patients under 35 years is insufficient and
that an additional correction for patients between 35–40 years with estrogen-receptor-positive tumors might be justified.
Both studies showed that the outcomes of ductal and lobular cancers were accurately
predicted, but for other histological subtypes, the predicted outcomes by Adjuvant! are too
pessimistic. At present, histology is not incorporated in Adjuvant!; however, the program
warns the user that some histological subtypes might warrant an adjustment (e.g., medullary
cancers where high grade does not confer high risk).28 Other discrepancies between
observed outcomes and outcomes predicted by Adjuvant! seem modest or inconsistent
between our study and the original validation study. For example, underestimation of
BCSS was seen in one subgroup of tumor size. Olivotto and colleagues13
noted no suchunderestimation, although the distributions of tumor size were similar. This suggests
that the discrepancy in predicted and observed BCSS is not caused by a suboptimum
incorporation of size in the Adjuvant! model.
A second subgroup in which the underestimation of BCSS was significant is patients with
one to three positive lymph nodes. Although we do not have information about the extent of
lymph-node involvement (i.e., isolated tumor cells, micrometastases, or macrometastases),
until the late 1990s lymph nodes that contained only isolated tumor cells were assessed
as positive lymph-nodes in the Netherlands. Consequently, the group of patients with one
to three positive lymph nodes in our database probably includes some patients with only

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 133/248
Chapter 8
146
isolated cells who have a better disease outcome than patients with macrometastases in
one to three lymph-nodes (Supplements).29,30 As for younger patients, the predicted overall
survival by Adjuvant! was too optimistic for patients older than 70 years, which is possibly
caused by the lack of data on co-morbidity status. Co-morbidity was entered as the default
assumption of minor health problems, which is likely to be an underestimation in older
patients and therefore to result in overestimation of overall survival in these patients. The
accurate prediction of BCSS in patients older than 70 years supports this hypothesis.
The proportion of missing data is one of the limitations of our retrospective cohort for
the validation of Adjuvant!; we lacked data on estrogen-receptor status, tumor grade, or
both for 3104 (58%) of 5380 patients. Missing information about tumor grade or estrogen-
receptor status will now be less common. However, patients with incomplete data
had similar disease outcome as patients with complete data, indicating that including
patients with missing data did not induce a selection bias (Table 1). Information on HER2
status was not available in this cohort and will be incorporated in an upcoming version of
Adjuvant!. The program predicted disease outcome accurately for patients with unknown
estrogen-receptor status. By contrast, the model underestimated BCSS in patients with
estrogen-receptor-negative tumors. Detailed analysis of this subgroup revealed that the
underestimation was exclusively seen in patients treated with hormonal therapy (n=250;
Supplements). This particular group had better outcome than predicted, suggesting that these
tumors could have been erroneously scored or coded in the registry as estrogen-receptor-
negative.
Patients who were partly treated at NKI-AVL were mainly referred from regional hospitals toour institute for radiotherapy. All diagnostic information was made available and reviewed
by the NKI-AVL. Adjuvant! predicted overall survival and BCSS accurately in these patients
and those treated at NKI-AVL ( Supplements). As a consequence, the population includes a
much wider representation of patients, and selection bias of our cohort is likely to be less
pronounced than in a single-institute cohort.
This large-scale validation study of Adjuvant! in a hospital-based population of Dutch
patients with breast cancer showed that the calculated predictions by Adjuvant! agreed
with the observed outcomes and that the predictions are applicable to a Dutch population,
and presumably to a European population, corroborating that populations of patientswith European ancestry in different continents have similar disease. Potential differences
between US and European patients with breast cancer could have resulted in deviations
of outcome in both directions and therefore would level out in an overall comparison of
predicted and observed outcomes. The good performance of the model in American and
European settings implies that the prognostic features and disease course are broadly
similar in both settings.
The model’s success in these settings does not ensure success in other uses, because,
for example, time, changes in exogenous exposures (hormone replacement therapy),
diagnostic techniques (types and intensity of screening), and surgical staging could affect

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 134/248
Dutch validation of Adjuvant!
147
8
the prognosis of patients with otherwise similar tumors. Furthermore, although we used a
large validation set, somewhat larger than the validation in British Columbia Breast Cancer
patients published by Olivotto and colleagues (n=4083), some subgroups were small and
findings in those groups should be considered with at least some caution.
To validate the Adjuvant! model in our study population we investigated both the
calibration (goodness of fit) and the discriminatory accuracy of the model. Although the
latter is rarely tested, it is of paramount importance to justify the use of prognostic models
for clinical outcome prediction.23,24 Results of the discriminatory accuracy of the Adjuvant!
model showed that in addition to good calibration, the model was capable of separating
individuals with a poor outcome from those with a good outcome with moderate power
(c-index 0.71). Remarkably, the discriminatory accuracy of a multivariate Cox model fitted
to our dataset was similar to that of Adjuvant!, indicating that the prognostic information
of the variables used in Adjuvant! was incorporated in the model in the best way possible.
Furthermore, the maximum explained variation by clinicopathological variables is about
15%, irrespective of whether they are incorporated in Adjuvant! or a model fitted to
our dataset. that the unexplained variation remains relatively large is supported by the
observation that patients with identical clinicopathological variables can have strikingly
different outcomes and proves that the information captured by these criteria can only
explain part of the differences in outcome. incorporation of biological markers, such as
molecular profiles and germline variants, in the model will likely increase the explained
variation and therefore result in a more rigorous prediction of outcome at the individual
patient level in the near future.
Contributors
SM, MKS, ER, LVV, and PMR designed the study. SM, MKS, AOV, OV, SMR, and PMR collected
data. SM, MKS, and NA analyzed data. SM, MKS, ER, NA, LVV, and PMR interpreted data. SM,
MKS, ER, LVV, and PMR wrote the paper.
Funding
Dutch National Genomics Initiative-Cancer Genomics Center, Dutch Cancer Society-KWF
grant NKI 2007-3839.
Conflicts of interest
PMR owns and is paid in part by Adjuvant Inc, which owns the rights to Adjuvant! online.
The other authors have no conflicts of interest to declare.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 135/248
Chapter 8
148
Acknowledgments
We thank Hans Peterse (deceased), Otilia Dalesio, and the Medical Registry staff for
providing baseline data, Hans Bonfrer and Tiny Korse for providing the estrogen-receptor
ligand binding assay data, Matti Rookus, Flora van Leeuwen, and Marieke Vollebergh for
helpful discussions. This study was financially supported by the Dutch National Genomics
Initiative-Cancer Genomics Center (SM and SMR) and the Dutch Cancer Society-KWF grant
NKI 2007-3839 (MKS).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 136/248
Dutch validation of Adjuvant!
149
8
References
1. NCCN Clinical Practice Guidelines in Oncology. Breast Cancer V.1.2009. www.nccn.org. (Last accessed
June 2, 2009).
2. Eifel P, Axelson JA, Costa J, et al. National Institutes of Health consensus development conference
statement: Adjuvant therapy for breast cancer, November 1-3, 2000. J Natl Cancer Inst 2001; 93: 979-989.
3. Goldhirsch A, Glick JH, Gelber RD, Coates AS, Senn HJ. Meeting Highlights: International consensus
panel on the treatment of primary breast cancer. J Clin Oncol 2001; 19: 3817-3827.
4. Haybittle JL, Blamey RW, Elston CW, et al. A prognostic index in primary breast cancer. Br J Cancer 1982;
45: 361-366.
5. Galea MH, Blamey RW, Elston CE, Ellis IO. The Nottingham Prognostic Index in primary breast cancer.
Breast Cancer Res Treat 1992; 22: 207-219.
6. Ravdin PM, Siminoff LA, Davis GJ, et al. Computer program to assist in making decisions about adjuvant
therapy for women with early breast cancer. J Clin Oncol 2001; 19: 980-991.
7. Early Breast Cancer Trialists’ Collaborative Group. Polychemotherapy for early breast cancer: an
overview of the randomised trials. Lancet 1998; 352: 930-942.
8. Early Breast Cancer Trialists’ Collaborative Group. Tamoxifen for early breast cancer: an overview of the
randomised trials. Lancet 1998; 351: 1451-1467.
9. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for
early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet
2005; 365: 1687-1717.
10. Siminoff LA, Gordon NH, Silverman P, Budd T, Ravdin PM. A decision aid to assist in adjuvant therapy
choices for breast cancer. Psychooncology 2006; 15: 1001-1013.
11. Zikmund-Fisher BJ, Fagerlin A, Ubel PA. Improving understanding of adjuvant therapy options by using
simpler risk graphics. Cancer 2008; 113: 3382-3390.
12. Belkora J, Rugo HS, Moore DH, Hutton D, Esserman L. Risk communication with patients with breast
cancer: cautionary notes about printing Adjuvant! estimates. Lancet Oncol 2008; 9: 602-603.
13. Olivotto IA, Bajdik CD, Ravdin PM, et al. Population-based validation of the prognostic model
ADJUVANT! for early breast cancer. J Clin Oncol 2005; 23: 2716-2725.
14. Coleman MP, Quaresma M, Berrino F, et al. Cancer survival in five continents: a worldwide population-
based study (CONCORD). Lancet Oncol 2008; 9: 730-756.15. Sant M, Allemani C, Berrino F, et al. Breast carcinoma survival in Europe and the United States. Cancer
2004; 100: 715-722.
16. Chlebowski RT, Aiello E, McTiernan A. Weight loss in breast cancer patient management. J Clin Oncol 2002;
20: 1128-1143.
17. CBO Richtlijn Mammacarcinoom 2008. http://www.cbo.nl/product/richtlijnen/folder20021023121843/
rl_mamma_08. pdf (Last accessed, June 2, 2009).
18. Harlan LC, Clegg LX, Abrams J, Stevens JL, Ballard-Barbash R. Community-based use of chemotherapy
and hormonal therapy for early-stage breast cancer: 1987-2000. J Clin Oncol 2006; 24: 872-877.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 137/248
Chapter 8
150
19. Chlebowski RT, Chen Z, Anderson GL, et al. Ethnicity and breast cancer: factors influencing differences
in incidence and outcome. J Natl Cancer Inst 2005; 97: 439-448.
20. Love N. Management of breast cancer in the adjuvant and metastatic settings: Patterns of care in
medical oncology. http://www.paternsofcare.com/2005/3/adjuvant.htm (Last accessed June 2, 2009).
21. Bogaerts J, Cardoso F, Buyse M, et al. Gene signature evaluation as a prognostic tool: challenges in the
design of the MINDACT trial. Nat Clin Pract Oncol 2006; 3: 540-551.
22. Cardoso F, Van ‘t Veer L, Rutgers E, et al. Clinical application of the 70-gene profile: the MINDACT trial.
J Clin Oncol 2008; 26: 729-735.
23. Harrell FE, Jr., Lee KL, Mark DB. Multivariable prognostic models: issues in developing models,
evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 1996; 15: 361-387.
24. Schemper M and Henderson R. Predictive accuracy and explained variation in Cox regression. Biometrics
2000; 56: 249-255.
25. Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in
Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370:
1453-1457.
26. Kaplan EL and Meier P. Nonparametric estimation from incomplete observation. J Am Stat Assoc 1958; 53:
457-481.
27. Cox DR. Regression models and lifetables. J R Statist Soc B 1972; 34: 187-220.
28. Pedersen L, Holck S, Schiodt T, Zedeler K, Mouridsen HT. Medullary carcinoma of the breast, prognostic
importance of characteristic histopathological features evaluated in a multivariate Cox analysis. Eur J
Cancer 1994; 30A: 1792-1797.
29. Cote RJ, Fpeterson H, Chaiwun B, et al. Role of immunohistochemical detection of lymph-node
metastases in management of breast cancer. Lancet 1999; 354: 896-900.
30. Reed J, Rosman M, Verbanac K, et al. Prognostic implications of isolated tumor cells and micrometastases
in sentinel nodes of patients with invasive breast cancer: 10-year analysis of patients enrolled in the
prospective East Carolina University/Anne Arundel Medical Center Sentinel Node Multicenter Study.
J Am Coll Surg 2009; 208: 333-340.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 138/248
Dutch validation of Adjuvant!
151
8
Supplements Chapter 8
Supplementary Table 1. Different sources of pathology data.
Dept. Clin.
Chem.
Pathologist
logbook*PALGA Med. Reg. Unknown Total
N (%) N (%) N (%) N (%) N (%) N
Histology 482 (9.0) 4692 (87.2) 206 (3.8) 0 5380
Tumor size 429 (8.0) 4339 (80.6) 612 (11.4) 0 5380
Grade 397 (7.5) 3252 (60.4) 352 (6.5) 1379 (25.6) 5380
Number of positive lymph-nodes 486 (9.0) 4478 (83.2) 416 (7.8) 0 5380
Estrogen-receptor status 643 (11.9) 270 (5.0) 2214 (41.2) 0 2253 (41.9) 5380
Dept. Clin. Chemistry, Department of Clinical Chemistry; PALGA, Dutch network and National Database for
Pathology; Med. Reg., Medical Registry of Netherlands Cancer Institute-Antoni van Leeuwenhoek hospital
(NKI-AVL).
* Personal logbook of NKI-AVL pathologist J.L. Peterse.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 139/248
Chapter 8
152
S u p p l e m e n t a r y T a b l e 2 . A d j u v a n t ! p r e d i c t e d v e r s u s o b s e r v e d O S
a n d B C S S s t r a t i fi e d b y a g e a n d e
s t r o g e n - r e c e p t o r s t a t u s .
O v e r a l l s u r v i v a l
B r e a s t c a n c e r - s p e c i fi
c s u r v i v a l
N o .
A d j u v a n t !
p r e d i c t e d
O b s e r v e d
( S
E )
P r e d i c t e d -
O b s e r v e d
P - v a l u e
A d
j u v a n t !
p r e d i c t e d
O b s e r v e d
( S E )
P r e d i c t e d -
O b s e r v e d
P - v a l u e
A g e ≤ 3 5 y r s
2 7 2
6 9 . 5
6 7 . 4 ( 2 . 9 )
2 . 1
0 . 4 7
7 0 . 4
6 7 . 8
2 . 6
0 . 3 5
E s t r o g e n - r e c e p t o r s t a t u s
P o s i t i v e
9 6
7 3 . 8
6 4 . 5 ( 4 . 9 )
9 . 3
0 . 0 6
7 4 . 8
6 4 . 5 ( 4 . 9 )
1 0 . 3
0 . 0 4
N e g a t i v e
5 8
6 6 . 0
6 9 . 0 ( 6 . 1 )
- 3 . 0
0 . 6 2
6 6 . 8
6 9 . 0 ( 6 . 1 )
- 2 . 2
0 . 7 2
U n k n o w n
1 1 8
6 7 . 8
6 9 . 1 ( 4 . 3 )
- 1 . 3
0 . 7 6
6 8 . 7
6 9 . 9 ( 4 . 3 )
- 1 . 2
0 . 7 8
A g e 3 5 - 4 0 y r s
3 0 0
7 5 . 0
6 8 . 9 ( 2 . 7 )
6 . 1
0 . 0 2
7 6 . 3
6 9 . 8 ( 2 . 7 )
6 . 5
0 . 0 2
E s t r o g e n - r e c e p t o r s t a t u s
P o s i t i v e
1 1 9
7 8 . 9
6 8 . 9 ( 4 . 2 )
1 0 . 0
0 . 0 2
8 0 . 2
6 9 . 6 ( 4 . 2 )
1 0 . 6
0 . 0 1
N e g a t i v e
5 8
6 8 . 4
7 0 . 7 ( 6 . 0 )
- 2 . 3
0 . 7 0
6 9 . 5
7 0 . 7 ( 6 . 0 )
- 1 . 2
0 . 8 4
U n k n o w n
1 2 3
7 4 . 4
6 8 . 1 ( 4 . 2 )
6 . 3
0 . 1 4
7 5 . 7
6 9 . 5 ( 4 . 2 )
6 . 2
0 . 1 4
O S , O v e r a l l s u r v i v a l ; B C S S , B r e a s t c a n
c e r - s p e c i fi c s u r v i v a l ; S E , S t a n d a r d e r
r o r .
P - v a l u e s b a s e d o n o n e s a m p l e t - t e s t .

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 140/248
Dutch validation of Adjuvant!
153
8
Supplementary Table 3. Adjuvant! predicted versus observed BCSS stratified by number of
positive lymph-nodes.
Patients Breast cancer-specific survival
No. %Adjuvant!
predicted
Observed
(SE)
Predicted -
Observed P -value
Number of positive lymph-nodes
0 2704 50.3 88.5 87.0 (0.7) 1.5 0.03
1 876 16.3 75.8 81.8 (1.3) -6.0 <0.0001
2 538 10.0 74.7 76.0 (1.9) -1.3 0.49
3 306 5.7 73.6 71.9 (2.7) 1.7 0.53
4 213 4.0 60.6 65.8 (3.4) -5.2 0.13
5 168 3.1 57.9 66.0 (3.8) -8.1 0.03
6 111 2.1 57.4 60.7 (4.9) -3.3 0.50
7 86 1.6 56.9 55.0 (5.5) 1.9 0.73
8 70 1.3 54.5 53.9 (6.2) 0.6 0.92
9 59 1.1 55.3 45.7 (6.8) 9.6 0.16
>9 249 4.6 37.5 37.7 (3.2) -0.2 0.95
BCSS, Breast cancer-specific survival; SE, Standard error.
P-values based on one sample t-test.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 141/248
Chapter 8
154
Supplementary Table 4. Adjuvant! predicted versus observed BCSS stratified by treatment and
estrogen-receptor status.
Patients Breast cancer-specific survival
No. %Adjuvant!
predicted
Observed
(SE)
Predicted -
Observed P -value
Untreated patients 2604
Estrogen-receptor status
Positive 1143 43.9 87.0 85.0 (1.1) 2.0 0.07
Negative 331 12.7 76.8 77.7 (2.3) -0.9 0.70
Unknown 1130 43.4 86.2 86.2 (1.1) 0.0 1.00
Chemotherapy only 815
Estrogen-receptor status
Positive 349 42.8 72.0 74.0 (2.4) -2.0 0.41
Negative 129 15.8 62.9 64.0 (4.3) -1.1 0.80
Unknown 337 41.3 69.2 72.3 (2.5) -3.1 0.22
Hormonal therapy only 1692
Estrogen-receptor status
Positive 787 46.5 77.8 77.4 (1.6) 0.4 0.80
Negative 192 11.3 55.5 64.9 (3.6) -9.4 0.01
Unknown 713 42.1 70.3 72.1 (1.8) -1.8 0.32
Chemo- & hormonal therapy 269
Estrogen-receptor status
Positive 138 8.2 74.1 73.6 (3.8) 0.5 0.90
Negative 58 3.4 50.7 62.0 (6.4) -11.3 0.08
Unknown 73 4.3 66.3 75.0 (5.1) -8.7 0.09
BCSS, Breast cancer-specific survival; SE, Standard error.
P-values based on one sample t-test.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 142/248
Dutch validation of Adjuvant!
155
8
Supplementary table 5. Adjuvant! predicted versus observed outcomes stratified by location
(within NKI-AVL or elsewhere) of primary surgery.
Patients
No. %Adjuvant!
predictedObserved (SE)
Predicted -
Observed P -value
Overall survival
Location of primary treatment 5380
Primary surgery NKI-AVL 1659 30.8 71.1 72.6 (1.1) -1.5 0.17
Primary surgery elsewhere 3721 69.2 68.2 67.4 (0.8) 0.8 0.32
Breast cancer-specific survival
Location of primary treatment 5380
Primary surgery NKI-AVL 1659 30.8 80.4 80.4 (1.0) 0.0 1.00
Primary surgery elsewhere 3721 69.2 77.1 77.8 (0.7) -0.7 0.32
NKI-AVL, Netherlands Cancer Institute – Antoni van Leeuwenhoek Hospital; SE, Standard error.
P-values based on one sample t-test.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 143/248
Chapter 9
Independent prognostic value of screen
detection in invasive breast cancer
Stella Mook
Laura J. Van ’t Veer
Emiel J.Th. Rutgers
Peter M. Ravdin
Anthonie O. van de Velde
Flora E. van Leeuwen
Otto Visser
Marjanka K. Schmidt
Accepted for publication in JNCI

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 144/248
Chapter 9
158
Abstract
Background
Mammographic screening has led to a proportional shift toward earlier-stage breast
cancers at presentation. We assessed whether the method of detection provides prognostic
information above and beyond standard prognostic factors and investigated the accuracy
of predicted overall and breast cancer–specific survival by the computer tool Adjuvant!
among patients with screen-detected, interval, and nonscreening-related carcinomas.
Methods
We studied 2592 patients with invasive breast cancer who were treated at the Netherlands
Cancer Institute from January 1, 1990, through December 31, 2000. Overall and breast
cancer–specific survival probabilities among patients with mammographically screen-
detected (n = 958), interval (n = 417), and nonscreening-related (n = 1217) breast
carcinomas were compared. Analyses were adjusted for clinicopathologic characteristics
and adjuvant systemic therapy. Because of gradual implementation of population-based
screening in the Netherlands, analyses were stratified a priori according to two periods of
diagnosis. All statistical tests were two-sided.
Results
Screen detection was associated with reduced mortality (adjusted hazard ratio for all-cause
mortality = 0.74, 95% confidence interval = 0.63 to 0.87, p < 0.001, and adjusted hazard
ratio for breast cancer–specific mortality = 0.62, 95% confidence interval = 0.50 to 0.78, p <
0.001, respectively) compared with nonscreening-related detection. The absolute adjusted
reduction in breast cancer–specific mortality was 7% at 10 years. The prognostic value
of the method of detection was independent of the period of diagnosis and was similar
across tumor size and lymph node status categories, indicating its prognostic value beyond
stage migration. Adjuvant! underestimated breast cancer–specific survival in patients withscreen-detected (-3.2%) and interval carcinomas (-5.4%).
Conclusions
Screen detection was found to be independently associated with better prognosis for
overall and breast cancer– specific survival and to provide prognostic information beyond
stage migration among patients with invasive breast cancer. We propose that the method
of detection should be taken into account when estimating individual prognosis.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 145/248
Prognostic value of screen detection
159
9
Introduction
Breast cancer mortality has decreased during the last several decades because of both the
introduction of mammographic screening and the improvement and more extensive use
of adjuvant systemic therapy.1-7 Several studies have shown that breast cancer screening
leads to a reduction of breast cancer mortality for the entire population.8-11 However, it is
still unclear how much the method of detection affects the prognosis of individual patients
and whether the method of detection should be used as a prognostic factor to improve
individualized treatment.
Breast cancers detected by screening mammography are often at an earlier stage of
development than those detected after the patient has displayed symptoms of disease.12-17
This stage shift at diagnosis is a reflection of screening-related lead-time bias (i.e., the time
between detection of the tumor by mammography and the moment the tumor would have
been detected in the absence of screening).18-20 Lead-time bias automatically lengthens
survival duration, thereby causing at least part of the observed improved outcome of
patients with screen-detected tumors. Another phenomenon that contributes to the
improved outcome of patients with a screen-detected tumor is length bias.19 Carcinomas
detected by screening are not a random sample of cancers in the population but, instead,
may contain a disproportionately large proportion of slow -growing tumors that tend to be
associated with better survival, even in the absence of screening. If the method of detection
has prognostic value that is independent of known prognostic factors (such as tumor size
and lymph node status), it could potentially improve the prediction of outcome and theselection of patients for adjuvant systemic therapy and should therefore be incorporated
in decision -making tools and guidelines.
Therefore, another important question is whether prognostic tools (such as the web-
based program Adjuvant!) that are based on an unknown mixture of screen-detected
and nonscreening-related carcinomas predict outcome of patients with screen-detected
breast cancer accurately. To our knowledge, the study by Wishart et al.21 was the only study
that has evaluated whether one of the currently available prediction models (i.e., the
Nottingham Prognostic Index) is adequate for screen-detected breast cancers. In addition,
to our knowledge, none of the earlier studies by others8-11
that examined the prognosticvalue of the method of detection on prognosis evaluated both the most important and
least biased outcomes: overall and breast cancer–specific survival.22 Therefore, we assessed
whether the method of detection (i.e., screen-detected carcinomas, interval carcinomas, or
nonscreening-related carcinomas) provided independent prognostic information for the
individual patient in a comprehensive way. In addition, we investigated whether outcomes
predicted by the web-based computer tool Adjuvant! were accurate, independent of the
method of detection.23-25

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 146/248
Chapter 9
160
Patients and Methods
Patient Selection
Women who were treated for invasive breast cancer at the Netherlands Cancer Institute–
Antoni van Leeuwenhoek Hospital (NKI-AVL) from January 1, 1990, through December
31, 2000, and aged 50–69 years were selected from a database that we constructed for
a previous study.23 The following selection criteria were used: 1) a diagnosis of invasive
unilateral breast carcinoma; 2) a known tumor size of T1 (≤ 2 cm), T2 (2–5 cm), or T3 (> 5 cm);
3) a known lymph node status of negative (pN0) or positive (pN1 = 1–3, pN2 = 4–9, or pN3
>9 positive lymph nodes); 4) no distant metastases; 5) primary surgery; 6) complete axillary
lymph node staging; and 7) administration of radiation therapy according to national
guidelines. Patients with previous malignancies and patients who received neoadjuvant
therapy were not included. A total of 2861 patients fulfilled the selection criteria and were
initially included in the analysis. No ethical review was required according to the Dutch
legislation.23
Breast Cancer Screening in the Netherlands
The Dutch screening program started April 1, 1990, in a number of zip code regions, and
all women aged 50–69 years in those regions were invited to participate in the screening
program. Zip code regions were selected on the basis of availability of screening units,and regions were added as soon as a supplementary screening unit became available until
full coverage was achieved in 1997.26-27 Women were invited for biennial mam mography
through a personal letter that included a scheduled appointment for mammography that
could be changed on request. Nonattendants received a reminder after 2–3 months.27
Screening mammograms were performed in independent and (mostly) mobile screening
units (3–8 units per region). No screening mammographies were performed outside the
national screening program. Information about screening mammography or diagnostic
mammography was recorded in separate systems in the screening facility or in the hospital.
Screening was extended to women aged 70–75 years in 1998. The national participationrate of the fully implemented Dutch screening program is between 70% and 80%.26-27
Method of Detection
Information about the method of detection was retrieved from the database of the
Comprehensive Cancer Center Amsterdam and was available for 2592 of 2861 patients.
The Comprehensive Cancer Center Amsterdam is a regional cancer registry that receives
this information from the Dutch national screening facil ities. Patients with an unknown
method of detection (n = 269) were excluded (Figure 1). Breast cancer–specific survival in this

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 147/248
Prognostic value of screen detection
161
9
group was similar to that in the group of patients with a known method of detection (n =
2592) (data not shown).
Figure 1. Flow diagram for patient selection and median follow-up by method of detection.
NKI–AVL = Netherlands Cancer Institute–Antoni van Leeuwenhoek Hospital.
We classified three types of breast carcinomas on the basis of method of detection: 1)
screen-detected carcinomas, defined as carcinomas that were mammographically detected
in the first or subsequent screening rounds (n = 958); 2) interval carcinomas, defined as
symptomatic carcinomas that were diagnosed within 24 months of a negative screening
(n = 417); and 3) nonscreening-related carcinomas, defined as symptomatic carcinomas in
patients who were not participating in the screening program (n = 1217). Among the 958
patients with a screen-detected carcinoma, 510 (53%) were detected in the first screening
round (i.e., prevalent carcinomas) and 443 (46%) in a subsequent screening round (i.e.,
incident carcinomas); this information was missing for five patients. Overall survival and
breast cancer–specific survival among the 510 patients with breast carcinomas that were
Selection NKI-AVL Medical Registry
Patients included in analyses
N = 2861
n = 2592
Median follow-up 11.0 y (range 0.2-19.1 y)
Nonscreening-related
carcinomas
n = 1217
Screen-detected carcinomas
n = 958
Interval carcinomas
n = 417
Alive
n = 689
Deceased
n = 528
Alive
n = 709
Deceased
n = 249
Deceased
n = 123
Alive
n = 294
Excluded
No information about method of detection (n=269)
Median follow-up (range)
14.1 y (0.8-19.1 y)
Median follow-up (range)
11.9 y (8.1-18.7 y)
Median follow-up (range)
11.2 y (3.8-17.5 y)

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 148/248
Chapter 9
162
detected in the first screening round was similar to those in patients with breast carci-
nomas that were detected in second or subsequent screening rounds ( Supplementary Figure
1 and Supplementary Table 1), so we pooled data from patients with screen-detected prevalent
carcinomas and from patients with screen-detected incident carcinomas. Ninety-six
patients had symptomatic carcinomas detected more than 24 months after a negative
screening (interval range = 25–83 months). Disease outcomes for these 96 patients were
similar to that for patients with nonscreening-related carcinomas, and so we pooled data
from the 96 patients with symptomatic carcinomas detected more than 24 months after
a negative screening and that from the 1121 patients with nonscreening-related cancers.
Because of the stepwise implementation of the screening, the group of patients who were
diagnosed with nonscreening-related breast carcinomas could presumably represent
different groups of patients in each period of diagnosis. That is, there could have been a
larger self-selected group of nonparticipants in the nonscreening group in the later years
of diagnoses (1997–2000) compared with the early years of diagnoses (1990–1996), during
which the nonparticipants were mostly noninvited persons. Therefore, we stratified our
results into two periods of diagnosis: 1990–1996 and 1997–2000.
Pathology Data
Data on histology, tumor size, tumor grade, number of positive lymph nodes, estrogen-
receptor status (Table 1), and HER2 status were retrieved from the NKI-AVL’s Department of
Clinical Chemistry, personal logbook of NKI-AVL pathologist, Dutch Network and NationalDatabase for Pathology, and the Medical Registry of the NKI-AVL, as previously described.23
Tumors were classified into categories of stage according to the International Union Against
Cancer TNM classification and were classified by the differentiation grade according to
methods previously described by Bloom and Richardson.28
Adjuvant Treatment
Information about adjuvant systemic therapy was obtained for each patient in this study
from the NKI-AVL Medical Registry. In general, the use of adjuvant systemic therapy inthe Netherlands increased, especially during the past decade.7 Since the introduction of
a consensus guideline for adjuvant systemic therapy by the Dutch Breast Cancer Platform
(NABON) in 2000, adjuvant systemic therapy was recommended for patients with lymph
node–positive breast cancer and for a selection of patients with lymph node–negative
breast cancer, according to tumor size and grade.29 Before the introduction of this
guideline, adjuvant systemic therapy was mainly recommended for lymph node–positive
disease, tamoxifen was recommended for postmenopausal patients, and chemotherapy
was recommended for premenopausal patients. In our study cohort of 2592 patients, 1150
(44.4%) did not receive adjuvant systemic therapy, 164 (6.3%) received chemotherapy,
1105 (42.6%) received hormonal therapy, and 173 (6.7%) received both chemotherapy and

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 149/248
Prognostic value of screen detection
163
9
hormonal therapy. Trends in the usage of adjuvant systemic therapy in our study cohort are
depicted in Supplementary Figure 2.
Outcome data
Outcome data were obtained from the NKI-AVL Medical Registry (date of first local, regional,
or distant recurrence; second malignancies; and/or contralateral breast cancer and date of
last follow-up or death). These outcome data were further completed by linking patient
records to the Dutch municipal registry, which contains the date of death or emigration
for all Dutch citizens. For patients who were not registered as having died or emigrated,
the date of last follow-up was recorded as February 1, 2009 ( i.e., 2 months before the date
of linkage). Cause of death was partially retrieved from the Medical Registry and partially
from individual patient files, with 418 breast cancer–specific deaths and 94 deaths from
other causes being identified. Patients without a known cause of death (n = 388) were
considered to have died of breast cancer if they were diagnosed with distant metastases
during follow-up (n = 77 breast cancer–specific deaths; n = 311 other causes).
Predicted Outcomes by Adjuvant!
To evaluate the influence of the method of detection on algorithms for outcome prediction,
we compared 10-year observed overall survival and breast cancer–specific survival with
those that had been predicted by Adjuvant! (Batch processor version 8.0; Adjuvant!Incorporation, San Antonio, TX). Adjuvant! is a web-based computer tool that calculates
individual outcomes by entering the patient’s age, co-morbidity, tumor size, tumor grade,
number of positive axillary lymph nodes, estrogen receptor status, and adjuvant systemic
therapy. For this study, predicted outcomes were calculated by entering clinicopathologic
data for each individual patient in the Adjuvant!, version 8.0 batch processor, including
HER2 status. The Adjuvant! processor was run by one of the authors (P. M. Ravdin), while
blinded to patient outcomes. The model’s estimation of prognosis is calculated based on
10-year observed overall survival of women diagnosed with breast cancer between January
1, 1988, and December 31, 1992, in the United States and recorded in the Surveillance,Epidemiology, and End Results database.25 The estimations of treatment efficacy by this
tool are mainly calculated from the proportional risk reductions derived from the Early
Breast Cancer Trialists’ Collaborative Group 1998 meta-analyses, which was recently
updated with the meta-analyses data from 2005.30-31 Because we could not retrieve reliable
data about co-morbidity, we used the default assumption of ‘minor health problems.’ In our
study, 1447 patients had complete data for all factors that were used to predict outcome
by the Adjuvant! model. Grade was unknown for 394 tumors, and estrogen receptor status
was unknown for 931 tumors; for these tumors, grade and estrogen receptor status were
entered in the model as ‘unknown.’ Given that Adjuvant! calculates predicted outcomes at
10 years, we evaluated its accuracy in a subgroup of patients who could have had at least
10 years of follow-up (i.e., the 2329 patients who were diagnosed before the year 2000).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 150/248
Chapter 9
164
T a b
l e 1 . A s s o c i a t i o n b e t w e e n c l i n i c
o p a t h o l o g i c a l c h a r a c t e r i s t i c s o f p a t i e n t s w i t h b r e a s t c a n c e r a n d m
e t h o d o f d e t e c t i o n * †
N o n s c r e e n i n g - r e l a t e d c a r c i n o m a
S c r e e n - d e t e c t e d c a r c i n o m a
P
I n t e r v a l c a r c i n o m a
P
C h
a r a c t e r i s t i c
N o .
( % )
N o .
( % )
N o .
( % )
Y e a r o f d i a g n o s i s
< 0 . 0 0 1
< 0 . 0 0 1
1 9 9 0 – 1 9 9 6
9 3 2 ( 7 6 . 6 )
5 1 4 ( 5 3 . 7 )
1 6 8 ( 4 0 . 3 )
1 9 9 7 – 2 0 0 0
2 8 5 ( 2 3 . 4 )
4 4 4 ( 4 6 . 3 )
2 4 9 ( 5 9 . 7 )
A g
e , y
< 0 . 0 0 1
0 . 0 2
5 0 – 5 9
7 1 5 ( 5 8 . 8 )
4 9 2 ( 5 1 . 4 )
2 7 2 ( 6 5 . 2 )
6 0 – 7 0
5 0 2 ( 4 1 . 2 )
4 6 6 ( 4 8 . 6 )
1 4 5 ( 3 4 . 8 )
H i s t o l o g y †
0 . 0 3
0 . 1 6
I D C
9 2 8 ( 7 6 . 3 )
7 0 8 ( 7 3 . 9 )
3 0 2 ( 7 2 . 4 )
I L C
1 4 4 ( 1 1 . 8 )
1 0 0 ( 1 0 . 4 )
6 4 ( 1 5 . 3 )
I D / L C
5 4 ( 4 . 4 )
7 2 ( 7 . 5 )
2 5 ( 6 . 0 )
O t h e r s
9 1 ( 7 . 5 )
7 8 ( 8 . 1 )
2 6 ( 6 . 2 )
T u
m o r s i z e ‡
< 0 . 0 0 1
0 . 1 8
p T 1
6 0 9 ( 5 0 . 0 )
7 2 7 ( 7 5 . 9 )
2 2 4 ( 5 3 . 7 )
p T 2
5 6 1 ( 4 6 . 1 )
2 2 4 ( 2 3 . 4 )
1 7 2 ( 4 1 . 2 )
p T 3
4 7 ( 3 . 9 )
7 ( 0 . 7 )
2 1 ( 5 . 0 )
N o
d a l s t a t u s §
< 0 . 0 0 1
0 . 0 5
p N 0
5 6 7 ( 4 6 . 6 )
6 3 5 ( 6 6 . 3 )
1 8 9 ( 4 5 . 3 )
p N 1
4 1 9 ( 3 4 . 4 )
2 1 8 ( 2 2 . 8 )
1 3 6 ( 3 2 . 6 )
p N 2
1 6 9 ( 1 3 . 9 )
7 5 ( 7 . 8 )
5 5 ( 1 3 . 2 )
p N 3
6 2 ( 5 . 1 )
3 0 ( 3 . 1 )
3 7 ( 8 . 9 )
S t a g e
< 0 . 0 0 1
0 . 3 6
I
3 7 9 ( 3 1 . 1 )
5 4 3 ( 5 6 . 7 )
1 3 4 ( 3 2 . 1 )
I I
5 8 5 ( 4 8 . 1 )
3 0 8 ( 3 2 . 2 )
1 8 5 ( 4 4 . 4 )
I I I
2 5 3 ( 2 0 . 8 )
1 0 7 ( 1 1 . 2 )
9 8 ( 2 3 . 5 )

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 151/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 152/248
Chapter 9
166
Statistical Analyses
Primary endpoints were overall survival, as measured from the time of diagnosis to death
from any cause, or breast cancer–specific survival, as measured from the time of diagnosis
to breast cancer–specific death. Patients who were still alive or who had died of other causes
were censored on the date of the last follow-up or death. Kaplan–Meier survival analyses,
log-rank tests, and univariate Cox proportional hazard ratios (HRs) were calculated to esti-
mate differences in survival (mortality HRs) among patients with screen-detected, interval,
or nonscreening-related breast carcinomas. To adjust for lead-time and length bias,
multivariable Cox proportional hazard models were used to calculate the independent
prognostic value of the method of detection after adjustment for age, tumor size, axillary
lymph node status, tumor grade, estrogen receptor status, and adjuvant systemic therapy.
In addition, to minimize lead-time bias, we evaluated disease outcome for screen-detected
and nonscreening-related tumors, stratified for lymph node status and for tumor size. The
proportional hazard assumption for the Cox model was evaluated by visual examination of
the log minus log curves. Data are presented as hazard ratios with 95% confidence intervals
(CIs). For the estimation of the absolute difference in survival, directly adjusted Cox survival
curves were generated.
To assess the value of Adjuvant!, we calculated the observed overall survival and breast
cancer–specific survival from Kaplan–Meier survival analyses for each subgroup by the
method of detection and stratified by period of diagnosis. For the same datasets, the
average predicted overall survival and breast cancer–specific survival percentages werecalculated from individual predicted outcomes by Adjuvant!. Observed and average
predicted outcomes were compared with a one-sample t test by assuming that the pre-
dicted outcomes were constant. All P values are two-sided, and a P value of less than .05
was considered statistically significant. Analyses were performed with SPSS, version 15.0
(SPSS, Inc, Chicago, IL) and STATA, version 11.1 (StataCorp, College Station, TX). The study
was reported according to the STROBE statement.32
Results
Baseline Characteristics and Stage Distribution
Analyses included 2592 patients (Figure 1), of whom 1614 were diagnosed with breast cancer
between January 1, 1990, and December 31, 1996, and 978 patients were diagnosed
between January 1, 1997, and December 31, 2000. As a consequence of the stepwise
implementation of breast cancer screening in the Netherlands, breast carcinomas of most
patients who were diagnosed before 1997 were detected outside the screening program.
This group of patients diagnosed between January 1, 1990, and December 31, 1996,

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 153/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 154/248
Chapter 9
168
Overall and Breast Cancer–Specific Survival by Method of Detection
Patients with screen-detected carcinomas had statistically significantly better overall
survival and breast cancer–specific survival than patients with nonscreening-related
carcinomas (for all-cause mortality, univariate HR = 0.60, 95% CI = 0.51 to 0.69, p < 0.001;
for breast cancer–specific mortality, univariate HR = 0.43, 95% CI = 0.34 to 0.53, p < 0.001)
(Figure 3, A and B). Similar patterns were observed for all-cause mortality and for breast cancer–
specific mortality in patients diagnosed between 1990 and 1996, and between 1997 and
2000 (Figure 3, C–F ).
In a multivariable model that was adjusted for age at diagnosis, tumor size, tumor grade,
lymph node status, estrogen receptor status, and adjuvant systemic therapy (Table 2), screen
detection was still independently associated with increased survival for patients diagnosed
with breast cancer between 1990 and 1996 (for all-cause mortality, adjusted HR = 0.77, 95%
CI = 0.64 to 0.92, p = 0.005; for breast cancer–specific mortality, adjusted HR = 0.66, 95%
CI = 0.50 to 0.86, p = 0.002). The favorable outcome of screen-detected carcinomas was of
similar magnitude in patients diagnosed more recently (for all-cause mortality, adjusted
HR = 0.73, 95% CI = 0.52 to 1.02, p = 0.07; for breast cancer–specific mortality, adjusted HR
= 0.63, 95% CI = 0.40 to 1.01, p = 0.05) but with less statistical significance. Overall, screen
detection was associated with reduced mortality (adjusted HR for all-cause mortality =
0.74, 95% CI = 0.63 to 0.87, p < 0.001; adjusted HR for breast cancer–specific mortality =
0.62, 95% CI = 0.50 to 0.78, p < 0.001) compared with nonscreening-related detection. The
absolute reduction in breast cancer–specific mortality at 10 years of follow-up betweenthe screen-detected and nonscreening-related carcinomas was 7% (adjusted survival rates
were 86% versus 79%, respectively; unadjusted differences were 13% with survival rates of
89% for screen-detected carcinomas and 76% for nonscreening-related carcinomas).
0.0
0.2
0.4
0.6
0.8
1.0
O v e r a l l s u r v i v a l p r
o b a b i l i t y
0 5 10 15
Time (years)
958
417 27356 217
883 602 152
Interval
Screen-detectedNumbersat
risk 1217 3111004 707 Nonscreening-related
Screen-detected versus nonscreening-related: HR = 0.60, 95% CI = 0.51 to 0.69
Interval versus nonscreening-related: HR = 0.79, 95% CI = 0.65 to 0.96
Log-rank p < 0.001
A

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 155/248
Prognostic value of screen detection
169
9
0.0
0.2
0.4
0.6
0.8
1.0
B r e a s t c a n c e r - s p e c i fi c
s u r v i v a l p r o
b a b i l i t y
0 5 10 15
Time (years)
958
417 27356 217
883 602 152
Interval
Screen-detectedNumbers
at
risk 1217 3111004 707 Nonscreening-related
Screen-detectedversus nonscreening-related: HR = 0.43, 95% CI = 0.34 to 0.53
Interval versus nonscreening-related: HR = 0.76, 95% CI = 0.59 to 0.98
Log-rank p < 0.001
0.0
0.2
0.4
0.6
0.8
1.0
O v e r a l l s u r v i v a l p r o b a b i l i t y
0 5 10 15
Time (years)
514
168 25142 122
472 416 152
Interval
Screen-detectedNumbers
at
risk 932 311760 608 Nonscreening-related
Screen-detectedversus nonscreening-related: HR = 0.63, 95% CI = 0.53 to 0.75
Interval versus nonscreening-related: HR = 0.72, 95% CI = 0.55 to 0.95
Log-rank p < 0.001
B
C

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 156/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 157/248
Prognostic value of screen detection
171
9
Figure 3. Kaplan–Meier curves for overall survival and breast cancer-specific survival by method
of detection. Log-rank p-values and univariate hazard ratios (HRs) for all-cause mortality and
breast cancer-specific mortality with corresponding 95% confidence intervals (CIs) at 5, 10, and
15 years are shown (error bars).
A) Overall survival for all patients (n = 2592).B) Breast cancer-specific survival for all patients (n = 2592).
C) Overall survival for patients diagnosed in 1990–1996 (n = 1614).
D) Breast cancer-specific survival for patients diagnosed in 1990–1996 (n = 1614).
E) Overall survival for patients diagnosed in 1997–2000 (n = 978).
F) Breast cancer-specific survival for patients diagnosed in 1997–2000 (n = 978). Interval
carcinomas were diagnosed 24 months or less after a negative screening. Non-screening-related
carcinomas were symptomatic cancer in patients who had not been screened or were screened
more than 24 months before detection of breast cancer. Numbers of patients at risk are shown
below each graph.
Furthermore, diagnosis of an interval carcinoma between 1990 and 1996 was independently
associated with better survival (for all-cause mortality, adjusted HR = 0.71, 95% CI = 0.54
to 0.96, p = 0.02; for breast cancer–specific mortality, adjusted HR = 0.70, 95% CI = 0.49 to
1.01, p = 0.05) compared with nonscreening-related detection. Conversely, diagnosis of an
interval carcinoma between 1997 and 2000 was not associated with survival (for all-cause
mortality, adjusted HR = 0.89, 95% CI = 0.63 to 1.24, p = 0.48; for breast cancer–specific
mortality, adjusted HR = 0.91, 95% CI = 0.59 to 1.40, p = 0.66) (Table 2).
0.0
0.2
0.4
0.6
0.8
1.0
B r e a s t c a n c e r - s p e c i fi c
s u r v i v a l p r
o b a b i l i t y
0 5 10
Time (years)
444
249 95209
411 186
Interval
Screen-detectedNumbers
at
risk 285 99244 Nonscreening-related
Screen-detectedversus nonscreening-related: HR = 0.47, 95% CI = 0.30 to 0.74
Interval versus nonscreening-related: HR = 1.11, 95% CI = 0.73 to 1.70
Log-rank p = 0.72
F

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 158/248
Chapter 9
172
We also found that the interaction term between the method of detection and lymph
node status was statistically significant in multivariable models for all-cause mortality ( p
= 0.045) and breast cancer–specific mortality ( p = 0.009). However, in the model including
the interaction term, screen detection was still associated with all-cause and breast
cancer–specific mortality, with similar HRs for screen-detected cancers (all-cause mortality,
adjusted HR = 0.70, 95% CI = 0.56 to 0.87, p = 0.001; breast cancer–specific mortality,
adjusted HR = 0.51, 95% CI = 0.36 to 0.72, p < 0.001) and somewhat lower HRs for interval
cancers (all-cause mortality, adjusted HR = 0.48, 95% CI = 0.33 to 0.71, p < 0.001; and breast
cancer–specific mortality, adjusted HR = 0.27, 95% CI = 0.14 to 0.51, p < 0.001).
Table 2. Multivariable Cox proportional hazard analyses for all-cause mortality and breast cancer-
specific mortality for all patients, patients who were diagnosed in the period of implementation
of screening (1990-1996), and patients who were diagnosed in the period when screening
reached full coverage (1997–2000)*.
All-cause mortalityBreast cancer-specific
mortality
Characteristics P HR (95% CI) P HR (95% CI)
Year of diagnosis 1990–2000
Method of detection
Screen-detected versus nonscreening-related <0.001 0.74 (0.63 to 0.87) <0.001 0.62 (0.50 to 0.78)
Interval carcinoma versus nonscreening-related 0.009 0.76 (0.62 to 0.93) 0.02 0.73 (0.56 to 0.94)
Age (per year) <0.001 1.05 (1.04 to 1.06) 0.15 1.01 (1.00 to 1.03)
pT†
pT2 (versus pT1) <0.001 1.51 (1.30 to 1.75) <0.001 1.75 (1.43 to 2.14)
pT3 (versus pT1) <0.001 1.80 (1.30 to 2.50) 0.02 1.65 (1.09 to 2.49)
pN‡
pN1 (versus pN0) <0.001 1.44 (1.16 to 1.77) 0.003 1.56 (1.17 to 2.07)
pN2 (versus pN0) <0.001 2.32 (1.82 to 2.97) <0.001 3.01 (2.18 to 4.15)
pN3 (versus pN0) <0.001 4.40 (3.25 to 5.94) <0.001 6.30 (4.36 to 9.10)
GradeII (versus I) 0.01 1.34 (1.06 to 1.69) <0.001 2.31 (1.51 to 3.55)
III (versus I) <0.001 2.31 (1.79 to 2.96) <0.001 4.59 (2.95 to 7.13)
Grade unknown (versus I) <0.001 1.54 (1.19 to 1.99) <0.001 3.03 (1.93 to 4.76)
ER status
ER negative (versus ER positive) 0.04 1.24 (1.01 to 1.53) 0.06 1.29 (0.99 to 1.68)
ER unknown (versus ER positive) 0.15 1.11 (0.96 to 1.29) 0.23 1.13 (0.92 to 1.39)
Chemotherapy (yes versus no) 0.14 0.83 (0.65 to 1.06) 0.02 0.71 (0.53 to 0.95)
Hormonal therapy (yes versus no) 0.02 0.78 (0.65 to 0.95) 0.10 0.80 (0.62 to 1.04)

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 159/248
Prognostic value of screen detection
173
9
Table 2. Continued
All-cause mortalityBreast cancer-specific
mortality
Characteristics P HR (95% CI) P HR (95% CI)
Year of diagnosis: 1990–1996
Method of detection
Screen-detected versus nonscreening-related <0.005 0.77 (0.64 to 0.92) 0.002 0.66 (0.50 to 0.86)
Interval carcinoma versus nonscreening-related 0.02 0.71 (0.54 to 0.96) 0.05 0.70 (0.49 to 1.01)
Age (per year) <0.001 1.04 (1.03 to 1.06) 1.0 1.00 (0.98 to 1.02)
pT†
pT2 (versus pT1) <0.001 1.54 (1.30 to 1.82) <0.001 1.86 (1.47 to 2.35)
pT3 (versus pT1) 0.003 1.79 (1.22 to 2.62) 0.04 1.64 (1.01 to 2.67)pN‡
pN1 (versus pN0) 0.04 1.31 (1.02 to 1.69) 0.08 1.37 (0.97 to 1.95)
pN2 (versus pN0) <0.001 2.23 (1.67 to 2.98) <0.001 3.00 (2.06 to 4.37)
pN3 (versus pN0) <0.001 4.13 (2.86 to 5.95) <0.001 6.13 (3.93 to 9.55)
Grade
II (versus I) 0.07 1.28 (0.99 to 1.66) 0.004 2.00 (1.25 to 3.18)
III (versus I) <0.001 2.15 (1.62 to 2.85) <0.001 3.91 (2.43 to 6.30)
Grade unknown (versus I) 0.02 1.40 (1.06 to 1.84) <0.001 2.49 (1.54 to 4.02)
ER status
ER negative (versus ER positive) 0.41 1.12 (0.86 to 1.47) 0.93 1.02 (0.73 to 1.42)
ER unknown (versus ER positive) 0.47 1.06 (0.90 to 1.25) 0.67 0.95 (0.76 to 1.19)
Chemotherapy (yes versus no) 0.11 0.75 (0.53 to 1.07) 0.03 0.64 (0.43 to 0.97)
Hormonal therapy (yes versus no) 0.17 0.85 (0.67 to 1.07) 0.16 0.80 (0.58 to 1.10)
Continued►

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 160/248
Chapter 9
174
Table 2. Continued
All-cause mortalityBreast cancer-specific
mortality
Characteristics P HR (95% CI) P HR (95% CI)
Year of diagnosis: 1997–2000
Method of detection
Screen-detected versus nonscreening-related 0.07 0.73 (0.52 to 1.02) 0.05 0.63 (0.40 to 1.01)
Interval carcinoma versus nonscreening-related 0.48 0.89 (0.63 to 1.24) 0.66 0.91 (0.59 to 1.40)
Age (per year) <0.001 1.06 (1.04 to 1.09) 0.005 1.05 (1.02 to 1.09)
pT†
pT2 (versus pT1) 0.05 1.36 (1.00 to 1.85) 0.22 1.29 (0.86 to 1.93)
pT3 (versus pT1) 0.10 1.71 (0.91 to 3.20) 0.43 1.39 (0.61 to 3.16)pN‡
pN1 (versus pN0) 0.006 1.71 (1.16 to 2.51) 0.02 1.89 (1.12 to 3.18)
pN2 (versus pN0) 0.001 2.27 (1.39 to 3.71) 0.01 2.29 (1.20 to 4.37)
pN3 (versus pN0) <0.001 4.71 (2.75 to 8.07) <0.001 6.04 (3.07 to 11.87)
Grade
II (versus I) 0.06 1.64 (0.97 to 2.75) 0.02 4.24 (1.31 to 13.78)
III (versus I) <0.001 2.86 (1.62 to 5.07) 0.001 7.24 (2.15 to 24.40)
Grade unknown (versus I) 0.02 2.33 (1.12 to 4.83) 0.08 3.68 (0.86 to 15.87)
ER status
ER negative (versus ER positive) 0.14 1.34 (0.91 to 1.98) 0.003 2.09 (1.28 to 3.42)
ER unknown (versus ER positive) 0.73 0.91 (0.52 to 1.58) 0.83 0.91 (0.39 to 2.12)
Chemotherapy (yes versus no) 0.99 1.00 (0.67 to 1.49) 0.46 1.21 (0.73 to 2.00)
Hormonal therapy (yes versus no) 0.10 0.73 (0.51 to 1.06) 0.38 1.25 (0.76 to 2.04)
* All analyses were done with the use of the Cox proportional hazard model. All statistical tests were two-
sided.
CI = confidence interval; ER = estrogen receptor; HR = hazard ratio.† pT = pT1 ≤2 cm; pT2 = 2–5 cm; pT3 >5 cm. ‡ pN = pN0 = lymph node-negative; pN1 = 1–3 positive lymph
nodes; pN2 = 4–9 positive lymph nodes; pN3 >9 positive lymph nodes.
In 1998, screening in the Netherlands was extended to woman aged 70–75 years. Including
those patients in this analysis resulted in 180 additional breast cancer patients, including
74 (41%) screen-detected breast cancers, 14 (8%) interval breast cancers, and 92 (51%)
nonscreening-related breast cancers. When we included this age group in the survival
analysis, the difference in outcomes between screen-detected and nonscreening-related

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 161/248
Prognostic value of screen detection
175
9
carcinomas was even larger for breast cancer–specific mortality (unadjusted HR = 0.35,
95% CI = 0.23 to 0.52, p < 0.001 and adjusted HR = 0.49, 95% CI = 0.32 to 0.75, p < 0.001)
( Supplementary Table 2).
Screen-detected breast carcinomas were smaller (mean size 17 versus 24 mm; p < 0.001)
and more often (66.3% versus 46.6%) had a lymph node–negative status compared with
nonscreening-related carcinomas, reflecting the well-known stage shift caused by
screening (Table 1). In addition to the multivariable analyses, we compared breast cancer–
specific survival between patients with screen-detected carcinomas and patients with
nonscreening-related carcinomas as stratified by tumor size and by lymph node status.
Because the differences in breast cancer–specific survival between screen-detected and
nonscreening-related carcinomas were similar in both periods of diagnosis (1990–1996
and 1997–2000), we pooled patients with such carcinomas to increase sample sizes for
subgroup analyses by tumor size and lymph node status. Patients with screen-detected
cancers had better breast cancer–specific survival than patients with nonscreening-related
tumors within each stratum of tumor size, with the most pronounced difference in tumors
of 10 mm or less in diameter (for breast cancer–specific mortality, unadjusted HR = 0.28, 95%
CI = 0.11 to 0.71, p = 0.007; adjusted HR = 0.35, 95% CI = 0.13 to 0.96, p = 0.04) ( Supplementary
Table 3 and Supplementary Figure 3, A–D). In analyses stratified by lymph node status, better breast
cancer–specific survival was associated with screen-detected tumors in both patients with
lymph node–negative and patients with lymph node–positive breast cancer (in lymph
node–negative patients, unadjusted HR for breast cancer–specific mortality = 0.40, 95% CI
= 0.28 to 0.56, p < 0.001; in lymph node–positive patients, unad justed HR = 0.59, 95% CI =0.45 to 0.79, p < 0.001). After adjustment for other prognostic factors (including age, tumor
size, grade, estrogen receptor status and adjuvant systemic therapy), screen detection was
strongly and statistically significantly associated with improved breast cancer–specific
survival among patients with lymph node–negative disease, but this association was
weaker and non-statistically significant among patients with lymph node–positive disease
(in lymph node–negative patients, adjusted HR for breast cancer–specific mortality =
0.51, 95% CI = 0.36 to 0.73, p < 0.001; in lymph node–positive patients, adjusted HR = 0.79,
95% CI = 0.59 to 1.06, p = 0.12) ( Supplementary Table 4 and Supplementary Figure 3, E–F ). The observed
survival difference of patients with lymph node–positive screen-detected carcinomas wasto a larger extent associated with stage shift and period of diagnosis; that is, lymph node–
positive patients with screen-detected breast cancer were statistically significantly more
likely to be diagnosed in 1997–2000 and to have smaller and better differ entiated tumors
than lymph node–positive patients whose breast cancer was not detected by screening ( p
< 0.001) (data not shown). Screen detection was also independently associated with breast
cancer–specific survival among systemically untreated patients (adjusted HR = 0.48, 95%
CI = 0.32 to 0.71, p < 0.001).

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 162/248
Chapter 9
176
T a b
l e 3 . A d j u v a n t ! p r e d i c t e d a n d o b
s e r v e d 1 0 - y e a r o v e r a l l s u r v i v a l a
n d b r e a s t c a n c e r - s p e c i fi c s u r v i v a
l f o r a l l p a t i e n t s d i a g n o s e d b e f o r e 2 0 0 0 , f o r
p a t
i e n t s d i a g n o s e d i n t h e p e r i o d o f i m p l e m e n t a t i o n o f s c r e e n i n g ( 1 9
9 0 – 1 9 9 6 ) , a n d f o r p a t i e n t s d i a g n
o s e d i n t h e p e r i o d w h e n s c r e e n i n g r e a c h e d
f u l l
c o v e r a g e ( 1 9 9 7 – 1 9 9 9 ) * .
1 0 - y e a r o v e r a l l s u r v i v a l
1 0 - y e a r b r e a s t c a n c e r - s p e c
i fi c s u r v i v a l
P e
r i o d o f d i a g n o s i s a n d
m e t h o d o f d e t e c t i o n
N o .
P a t i e n
t s ( % )
A d j u v a n t !
p r e d i c t e d ,
%
O b s e r
v e d ,
% (
9 5 %
C I )
P r e d i c t e d –
o b s e r v e d
P
A d
j u v a n t !
p r e d i
c t e d ,
%
O b s e r v e d ,
% (
9 5 % C
I ) P r e d i c t e
d –
o b s e r v e d
P
M e t h o d o f d e t e c t i o n , y e a r o f d i a g n o
s i s : 1 9 9 0 – 1 9 9 9
N
o n s c r e e n i n g r e l a t e d
1 1 4 9
( 6 4 . 9 )
6 9 . 2
6 6 . 6 ( 6 3 . 9 t o 6 9 . 3 )
2 . 6
0 . 0 6
7 6 . 5 7 5 . 7 ( 7 3 . 2 t o 7 8 . 2 )
0 . 8
0 . 5 4
S
c r e e n - d e t e c t e d
8 3 0
( 4 6 . 9 )
7 7 . 6
8 2 . 0 ( 7 9 . 5 t o 8 4 . 5 )
- 4 . 4
< 0 . 0 0 1
8 6 . 1 8 9 . 3 ( 8 7 . 1 t o 9 1 . 5 )
- 3 . 2
0 . 0 0 4
I
n t e r v a l c a r c i n o m a
3 5 0
( 1 9 . 8 )
6 8 . 7
7 2 . 4 ( 6 7 . 7 t o 7 7 . 1 )
- 3 . 7
0 . 1 2
7 5 . 5 8 0 . 9 ( 7 6 . 6 t o 8 5 . 2 )
- 5 . 4
0 . 0 2
M e t h o d o f d e t e c t i o n , y e a r o f d i a g n o
s i s : 1 9 9 0 – 1 9 9 6 ( i m p l e m e n t a t i o n o
f s c r e e n i n g )
N
o n s c r e e n i n g r e l a t e d
9 3 2
( 5 7 . 7 )
6 8 . 6
6 5 . 3 ( 6 2 . 2 t o 6 8 . 4 )
3 . 3
0 . 0 4
7 6 . 2 7 4 . 3 ( 7 1 . 4 t o 7 7 . 2 )
1 . 9
0 . 2 1
S
c r e e n - d e t e c t e d
5 1 4
( 3 1 . 8 )
7 6 . 7
8 0 . 9 ( 7 7 . 6 t o 8 4 . 2 )
- 4 . 2
0 . 0 1
8 5 . 5 8 7 . 7 ( 8 4 . 8 t o 9 0 . 6 )
- 2 . 2
0 . 1 4
I
n t e r v a l c a r c i n o m a
1 6 8
( 1 0 . 4 )
6 8 . 9
7 3 . 2 ( 6 6 . 5 t o 7 9 . 9 )
- 4 . 3
0 . 2 1
7 5 . 9 8 0 . 9 ( 7 4 . 8 t o 8 7 . 0 )
- 5 . 0
0 . 1 1
M e t h o d o f d e t e c t i o n , y e a r o f d i a g n o
s i s : 1 9 9 7 – 1 9 9 9 ( f u l l c o v e r a g e o f s c r e e n i n g )
N
o n s c r e e n i n g r e l a t e d
2 1 7
( 2 2 . 2 )
7 1 . 9
7 2 . 3 ( 6 6 . 2 t o 7 8 . 4 )
- 0 . 4
0 . 9 0
7 8 . 2 8 1 . 7 ( 7 6 . 2 t o 8 7 . 2 )
- 3 . 5
0 . 2 1
S
c r e e n - d e t e c t e d
3 1 6
( 3 2 . 3 )
7 9 . 2
8 3 . 8 ( 7 9 . 7 t o 8 7 . 9 )
- 4 . 6
0 . 0 3
8 7 . 0 9 2 . 1 ( 8 9 . 0 t o 9 5 . 2 )
- 5 . 1
0 . 0 0 2
I
n t e r v a l c a r c i n o m a
1 8 2
( 1 8 . 6 )
6 8 . 6
7 1 . 7 ( 6 5 . 0 t o 7 8 . 4 )
- 3 . 1
0 . 3 6
7 5 . 3 8 0 . 8 ( 7 4 . 9 t o 8 6 . 7 )
- 5 . 5
0 . 0 0 7
* A n a l y s e s w e r e d o n e w i t h t h e u s e o f o n
e s a m p l e t t e s t s . A l l s t a t i s t i c a l t e s t s w
e r e t w o - s i d e d . C I = c o n fi d e n c e i n t e r v a l .

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 163/248
Prognostic value of screen detection
177
9
Adjuvant! Predictions
To evaluate the influence of the method of detection on an algorithm for outcome
prediction, we compared 10-year observed overall survival and breast cancer–specific
survival with 10-year overall survival and breast cancer–specific survival that had
been predicted by Adjuvant!. Adjuvant! predicted the outcome among patients with
nonscreening-related carcinomas accurately, that is, the predicted survival of patients with
a nonscreening-related carcinoma was within 2% of the observed survival and/or non-
statistically significantly different in all but one group: Adjuvant! overestimated overall
survival in patients with a nonscreening-related carcinoma diagnosed between 1990 and
1996 with 3.3% ( p= 0.04). However, Adjuvant! predictions underestimated overall survival
and breast cancer–specific survival among patients with screen-detected and interval
carcinomas. Prediction of breast cancer–specific survival was underestimated by Adjuvant!
for patients with screen-detected and interval carcinomas by -3.2% and -5.4%, respectively.
Among patients with screen-detected carcinomas, in particular, Adjuvant! underestimated
survival for all periods of diagnosis (Table 3). In addition, Adjuvant! underestimated breast
cancer–specific survival in patients younger than 50 years whose breast cancer was
diagnosed more recently (1997–2000) with -3.0%, reflecting the observed 22% reduction
in breast cancer–specific survival, whereas Adjuvant! predictions for patients younger than
50 years diagnosed between 1990 and 1996 were accurate ( Supplementary Table 5 ).23
Discussion
We found that screen detection was independently associated with better breast cancer–
specific survival, as shown in multivariable analyses and analyses stratified for tumor size
and lymph node status, and provided prognostic information beyond stage migration
for patients with invasive breast cancer. These results are in agreement with previous
studies.9,11,21 Therefore, the method of detection should be taken into account when
selecting patients for adjuvant systemic therapy and withholding chemotherapy for women
with screen-detected carcinoma could be considered. We also analyzed the accuracy ofpredicted disease outcome by the computer tool Adjuvant! as stratified by the method of
detection.25 When we compared outcomes from this study with outcomes predicted by
Adjuvant! for the same patients, we found that predicted breast cancer–specific survival
by Adjuvant! was underestimated for all three groups, with the most pronounced and
statistically significant differences in patients with screen-detected and interval breast
carcinomas.
The true independent prognostic value of the method of detection for individual breast
cancer patients may remain a matter of dispute. This dispute may not be settled unless
a precise method for assessing tumor advancement is developed. Nonetheless, we

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 164/248
Chapter 9
178
have obtained consistent evidence in this study that the method of detection was an
independent prognostic factor beyond stage shift for disease outcome in patients with
invasive breast carcinomas, with increased survival being associated with screen-detected
carcinomas.
However, the question remains whether models and guidelines for adjuvant systemic
therapy that were developed in an (partially) unscreened population are applicable to
patients with screen-detected carcinomas and whether the use of these models and guide-
lines may lead to overtreatment in these patients. Our data indicate that current models for
determining prognosis in breast cancer patients may be improved by including the method
of detection. In our study, the general underestimation of survival outcome by Adjuvant!
for patients diagnosed with breast cancer in 1997 through 1999 may be attributed in part
to improved salvage therapy and adjuvant systemic therapy.33-35 We observed a reduction
in breast cancer–specific mortality for patients younger than 50 years who were recently
diagnosed, which supports this hypothesis. However, the underestimations of overall
and breast cancer–specific survival by Adjuvant! were most pronounced in patients with
screen-detected carcinomas, indicating that although improved therapy will influence the
model’s prediction, the method of detection should be taken into account when selecting
patients for adjuvant systemic therapy.
It is well established and confirmed by our study that screened populations have a larger
proportion of smaller, lymph node–negative, lower grade, and estrogen receptor–positive
tumors than nonscreened populations. Stratification by tumor size reduces the magnitude
of lead-time bias that is caused by stage shift, although it may not completely eliminatelead-time bias because shift within a stage can still occur (e.g., more T1ab tumors with a
diameter of ≤ 1 cm in the pT1 category of ≤ 2 cm tumors). We found that, even within
strata of less than 10-mm tumors and of 10- to 20 mm tumors, screen-detected carcinomas
were associated with better breast cancer–specific survival than non-screened carcinomas.
Stratification by lymph node status showed that, despite the prognostic value of screen
detection being similar among patients with lymph node–negative and lymph node–
positive disease, screen detection was independently associated with breast cancer–
specific survival especially for patients with no lymph node metastases at diagnosis and
that the observed survival difference of patients with lymph node–positive screen-detectedcarcinomas was to a larger extent associated with stage shift and period of diagnosis.
When studying the effect of screening on mortality at the population level, both lead-time
(stage shift) and length bias (less-aggressive tumors) can cause a spurious improvement of
survival in the screened population. When investigating the independent prognostic value
of the method of detection on the prediction of outcome for an individual patient, screen-
detected carcinomas appear to have a more favorable tumor biology (e.g., to be at a low
grade at diagnosis) and are subject to potential overdiagnosis.36 A different natural history
of screen-detected carcinomas has also been postulated by others.37,38 Moreover, we found
that, even after adjustment for known prognostic factors and within strata of tumor size,

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 165/248
Prognostic value of screen detection
179
9
method of detection had independent prognostic value. This result could indicate that
we were not able to completely correct for length bias with the prognostic factors that
were available; however, we argue that it is exactly this remaining unexplained difference
in tumor biology beyond stage shift (length bias) that is important in the prediction of
outcome for the individual patient.
Although the prognostic value of screen detection was similar among patients diagnosed
in 1990–1996 and those diagnosed in 1997–2000, there were several reasons to stratify our
data analyses according to period of diagnosis. First, because the stepwise implementation
of screening in the Netherlands, patients diagnosed with nonscreening-related breast
carcinomas in 1990–1996 were predominantly women who had not been invited for
screening in a certain geographic region, whereas patients diagnosed with nonscreening-
related breast carcinomas after 1996 were more likely to have been a specific subset of
patients who decided not to participate in the breast cancer screening program for various
reasons. Patients diagnosed from 1990 to 1996 were expected to be a random selection
of patients that, consequently, can be viewed as a unique control group of nonscreening-
related cancers. Patients diagnosed after 1996 are subject to selection biases, such as
worse accessibility to adequate treatment facilities or lower socioeconomic status, which
will influence both participation rate and outcome. In addition, as shown by Kalager et
al.,10 organized screening programs also result in a survival benefit for patients outside
the screening program that can be attributed to increased awareness and optimization
of breast cancer care. This effect may dilute the prognostic value of screen detection,
especially in more recent years (1997–2000) when the coverage of screening was complete. The possibility that both screening and improved adjuvant systemic therapy contributed to
the reduction in breast cancer mortality from 1990 to 2010 with similar magnitude further
emphasizes the necessity for comparisons during the same period between patients with
screen-detected carcinomas and those with nonscreening-related carcinomas.39
The observed intermediate survival among patients with interval breast cancers was
consistent with previous studies.40-42 Interval breast carcinomas are a heterogeneous
group of tumors consisting of true interval carcinomas (i.e., rapidly growing tumors), occult
carcinomas, and tumors that were missed on previous screening mammography (i.e., slowly
growing tumors).43
The latter group of tumors could be related to breast density and thusassociated with younger age at diagnosis, which we did observe. Although general baseline
tumor characteristics did not differ much between interval cancers and nonscreening-
related cancers, patients with interval carcinomas received adjuvant systemic therapy
more often. However, we found that, in the adjuvant-untreated group specifically, survival
was similar between patients with interval carcinomas and patients with a screen-detected
carcinoma (data not shown). In addition, increased patient awareness as a result of the
screening program and self-selection could have resulted in a better outcome for interval
carcinomas.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 166/248
Chapter 9
180
One of the strengths of our study was that information about whether a tumor was
detected in the first screening round ( i.e., was a prevalent carcinoma) or in a subsequent
screening round (i.e., was an incident carcinoma) was available. Another strength was
that both overall survival and breast cancer–specific survival could be evaluated and that
outcome data were collected in a manner that was blinded to the method of detection,
thereby eliminating potential problems of differential bias in ascertainment and coding
of cause of death (i.e., the sticky-diagnosis and slippery-linkage biases, respectively).44 In
addition, patients in this study cohort had a substantial follow-up.
As a consequence of the conservative adjuvant systemic therapy guidelines that were
used during the time patients in this study cohort were treated for breast cancer, a large
proportion of patients received no chemo and/or hormonal therapy ( Supplementary Figure
2). Although most patients with early-stage breast cancer currently receive some form
of adjuvant systemic therapy, the estimated prognosis (i.e., disease outcome without
adjuvant systemic therapy) is important for the decision whether or not to treat patients
with adjuvant systemic therapy. We found that method of detection has independent
prognostic value, with screen detection associated with better survival. Thus, withholding
chemotherapy for women with screen-detected carcinoma could be considered; however,
these results require validation in an independent series of patients.
There have been several randomized clinical screening trials8,9,11 that have investigated the
association between screening and outcome. These studies have identified a reduction of
25%–35% in breast cancer mortality that is associated with screen detection, which was
sustained, though attenuated, after adjustment for prognostic factors. Notwithstandingthe outcome of the randomized clinical trials, these results are not simply applicable to the
general and diverse population that is participating in breast cancer screening. Shen et al.11
studied patients who were included in trials that were conducted in 1963–1966 and 1980–
1985, thus representing different birth cohorts from those of women who are currently at
risk of breast cancer. In addition, they missed important clinicopathologic information (e.g.,
exact tumor size and tumor grade). Although Joensuu et al.9 had detailed information and
could adjust distant disease-free survival for tumor size, number of positive lymph nodes,
tumor grade, and hormone receptor status, there were only 443 patients with a screen-
detected carcinoma. Wishart et al.21
have shown that screen-detected carcinomas wereassociated with better overall survival than symptomatic breast cancer. The prognostic
value of screen detection remained statistically significant after correction for stage shift
defined by the Nottingham Prognostic Index, but no data on breast cancer–specific
survival were included. Although Wishart et al.21 analyzed 5604 patients, the control group
(i.e., symptomatic breast cancer patients) consisted of a mixture of patients with potentially
very different survival rates, that is, true interval carcinomas, patients with interval car-
cinomas diagnosed more than 3 years after a negative mammographic screening, and
patients who did not participate in the screening program.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 167/248
Prognostic value of screen detection
181
9
This study had several limitations. Information was not available for tumor markers, such
as HER2 (for the majority of patients) or Ki67. However, it is not likely that the remaining
difference in outcome between screen-detected and nonscreening-related tumors can
be explained merely by these factors.45 In general, patients were treated according to
guidelines available at that time; however, other factors (e.g., co-morbidity or HER2 status)
could have influenced choice of treatment. Residual con founding by indication was shown
by the increased risk of death after chemotherapy or hormonal treatment in carcinomas
diagnosed in 1997–2000 (Table 2), although hazard ratios of treatment were non-statistically
significant. Several studies46-48 have shown that gene expression profiles can account for
a substantial part of the unexplained variance in prognosis. Therefore, the independent
prognostic value of method of detection after adjustment for gene expression in a tumor
remains to be determined.
In summary, we have shown that screen detection was consistently associated with disease
outcome and provided prognostic information beyond stage migration among patients
with invasive breast cancer. As a consequence, we propose that method of detection should
be used in combination with traditional markers of tumor burden and aggressiveness
to estimate prognosis for each patient, and to guide their decision to receive adjuvant
systemic therapy.
Funding
This work was supported by The Dutch Cancer Society (grant number NKI 2009-4363)(MKS) and the Dutch National Genomics Initiative-Cancer Genomics Center (grant number
NKI CGC 2008-2012) (LvtV).
Notes
We acknowledge the contribution of the Medical Registry and the Clinical Chemistry
Department of the NKI-AVL (Amsterdam, The Netherlands), all treating oncologists of the
patients concerned, and all radiologists who collected and interpreted the mammographic
screening data provided by the Comprehensive Cancer Center Amsterdam. Dr. Ravdin wasinvolved in the design of and has an interest in Adjuvant!. The funding sources had no role
in study design, collection, analysis, or interpretation of data, writing of the paper, or in
decisions relating to publication.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 168/248
Chapter 9
182
Reference List
1. Berry DA and Ravdin PM. Breast cancer trends: a marriage between clinical trial evidence and
epidemiology. J Natl Cancer Inst 2007; 99: 1139-1141.
2. Chu KC, Tarone RE, Kessler LG, et al. Recent trends in U.S. breast cancer incidence, survival, and mortality
rates. J Natl Cancer Inst 1996; 88: 1571-1579.
3. Garne JP, Aspegren K, Balldin G, Ranstam J. Increasing incidence of and declining mortality from breast
carcinoma. Trends in Malmo, Sweden, 1961-1992. Cancer 1997; 79: 69-74.
4. Jatoi I and Miller AB. Why is breast-cancer mortality declining? Lancet Oncol 2003; 4: 251-254.
5. Otten JD, Broeders MJ, Fracheboud J, et al. Impressive time-related influence of the Dutch screening
programme on breast cancer incidence and mortality, 1975-2006. Int J Cancer 2008; 123: 1929-1934.
6. Smigal C, Jemal A, Ward E, et al. Trends in breast cancer by race and ethnicity: update 2006. CA Cancer J Clin
2006; 56: 168-183.
7. Vervoort MM, Draisma G, Fracheboud J, van de Poll-Franse LV, de Koning HJ. Trends in the usage of
adjuvant systemic therapy for breast cancer in the Netherlands and its effect on mortality. Br J Cancer
2004; 91: 242-247.
8. De Koning HJ. Mammographic screening: evidence from randomised controlled trials. Ann Oncol 2003;
14: 1185-1189.
9. Joensuu H, Lehtimaki T, Holli K, et al. Risk for distant recurrence of breast cancer detected by
mammography screening or other methods. JAMA 2004; 292: 1064-1073.
10. Kalager M, Haldorsen T, Bretthauer M, et al. Improved breast cancer survival following introduction of
an organized mammography screening program among both screened and unscreened women: a
population-based cohort study. Breast Cancer Res 2009; 11: R44.
11. Shen Y, Yang Y, Inoue LY, et al. Role of detection method in predicting breast cancer survival: analysis of
randomized screening trials. J Natl Cancer Inst 2005; 97: 1195-1203.
12. Chu KC, Smart CR, Tarone RE. Analysis of breast cancer mortality and stage distribution by age for the
Health Insurance Plan clinical trial. J Natl Cancer Inst 1988; 80: 1125-1132.
13. Connor RJ, Chu KC, Smart CR. Stage-shift cancer screening model. J Clin Epidemiol 1989; 42: 1083-1095.
14. Ernst MF, Roukema JA, Coebergh JW, et al. Breast cancers found by screening: earlier detection, lower
malignant potential or both? Breast Cancer Res Treat 2002; 76: 19-25.
15. Feinstein AR, Sosin DM, Wells CK. The Will Rogers phenomenon. Stage migration and new diagnostictechniques as a source of misleading statistics for survival in cancer. N Engl J Med 1985; 312: 1604-1608.
16. Fracheboud J, Otto SJ, van Dijck JA, et al. Decreased rates of advanced breast cancer due to
mammography screening in The Netherlands. Br J Cancer 2004; 91: 861-867.
17. Weaver DL, Rosenberg RD, Barlow WE, et al. Pathologic findings from the Breast Cancer Surveillance
Consortium: population-based outcomes in women undergoing biopsy after screening mammography.
Cancer 2006; 106: 732-742.
18. Hutchison GB and Shapiro S. Lead time gained by diagnostic screening for breast cancer. J Natl Cancer Inst
1968; 41: 665-681.
19. Kramer BS, Gohagan JK, Prorok PC. Cancer screening: theory and practice. New York (NY): Marcel
Dekker; 1999.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 169/248
Prognostic value of screen detection
183
9
20. Shapiro S, Goldberg JD, Hutchison GB. Lead time in breast cancer detection and implications for
periodicity of screening. Am J Epidemiol 1974; 100: 357-366.
21. Wishart GC, Greenberg DC, Britton PD, et al. Screen-detected vs symptomatic breast cancer: is
improved survival due to stage migration alone? Br J Cancer 2008; 98: 1741-1744.
22. Krzyzanowska MK and Tannock IF. Should screen-detected breast cancers be managed differently?
J Natl Cancer Inst 2005; 97: 1170-1171.
23. Mook S, Schmidt MK, Rutgers EJ, et al. Calibration and discriminatory accuracy of prognosis calculation
for breast cancer with the online Adjuvant! program: a hospital-based retrospective cohort study. Lancet
Oncol 2009; 10: 1070-1076.
24. Olivotto IA, Bajdik CD, Ravdin PM, et al. Population-based validation of the prognostic model
ADJUVANT! for early breast cancer. J Clin Oncol 2005; 23: 2716-2725.
25. Ravdin PM, Siminoff LA, Davis GJ, et al. Computer program to assist in making decisions about adjuvant
therapy for women with early breast cancer. J Clin Oncol 2001; 19: 980-991.
26. De Koning HJ, Fracheboud J, Boer R, et al. Nation-wide breast cancer screening in The Netherlands:
support for breast-cancer mortality reduction. National Evaluation Team for Breast Cancer Screening
(NETB). Int J Cancer 1995; 60: 777-780.
27. Fracheboud J, De Koning HJ, Beemsterboer PM, et al. Nation-wide breast cancer screening in The
Netherlands: results of initial and subsequent screening 1990-1995. National Evaluation Team for
Breast Cancer Screening. Int J Cancer 1998; 75: 694-698.
28. Bloom HJ and Richardson WW. Histological grading and prognosis in breast cancer; a study of 1409
cases of which 359 have been followed for 15 years. Br J Cancer 1957; 11: 359-377.
29. Bontenbal M, Nortier JW, Beex LV, et al. [Adjuvant systemic therapy for patients with resectable breast
cancer: guideline from the Dutch National Breast Cancer Platform and the Dutch Society for Medical
Oncology]. Ned Tijdschr Geneeskd 2000; 144: 984-989.
30. Early Breast Cancer Trialists’ Collaborative Group. Polychemotherapy for early breast cancer: an
overview of the randomised trials. Lancet 1998; 352: 930-942.
31. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for
early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet
2005; 365: 1687-1717.
32. Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in
Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370:1453-1457.
33. Coleman MP, Quaresma M, Berrino F, et al. Cancer survival in five continents: a worldwide population-
based study (CONCORD). Lancet Oncol 2008; 9: 730-756.
34. Harlan LC, Clegg LX, Abrams J, Stevens JL, Ballard-Barbash R. Community-based use of chemotherapy
and hormonal therapy for early-stage breast cancer: 1987-2000. J Clin Oncol 2006; 24: 872-877.
35. Sant M, Allemani C, Berrino F, et al. Breast carcinoma survival in Europe and the United States. Cancer
2004; 100: 715-722.
36. Jorgensen KJ and Gotzsche PC. Overdiagnosis in publicly organised mammography screening
programmes: systematic review of incidence trends. BMJ 2009; 339: b2587.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 170/248
Chapter 9
184
37. Esserman L, Shieh Y, Thompson I. Rethinking screening for breast cancer and prostate cancer. JAMA
2009; 302: 1685-1692.
38. Zahl PH, Maehlen J, Welch HG. The natural history of invasive breast cancers detected by screening
mammography. Arch Intern Med 2008; 168: 2311-2316.
39. Berry DA, Cronin KA, Plevritis SK, et al. Effect of screening and adjuvant therapy on mortality from
breast cancer. N Engl J Med 2005; 353: 1784-1792.
40. Cowan WK, Angus B, Gray JC, Lunt LG, al Tamimi SR. A study of interval breast cancer within the NHS
breast screening programme. J Clin Pathol 2000; 53: 140-146.
41. Koivunen D, Zhang X, Blackwell C, Adelstein E, Humphrey L. Interval breast cancers are not biologically
distinct--just more difficult to diagnose. Am J Surg 1994; 168: 538-542.
42. Schroen AA, Wobbes T, van der Sluis RF. Interval carcinomas of the breast: a group with intermediate
outcome. J Surg Oncol 1996; 63: 141-144.
43. Porter PL, El Bastawissi AY, Mandelson MT, et al. Breast tumor characteristics as predictors of
mammographic detection: comparison of interval- and screen-detected cancers. J Natl Cancer Inst 1999;
91: 2020-2028.
44. Black WC, Haggstrom DA, Welch HG. All-cause mortality in randomized trials of cancer screening. J Natl
Cancer Inst 2002; 94: 167-173.
45. Harris L, Fritsche H, Mennel R, et al. American Society of Clinical Oncology 2007 update of
recommendations for the use of tumor markers in breast cancer. J Clin Oncol 2007; 25: 5287-5312.
46. Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-
negative breast cancer. N Engl J Med 2004; 351: 2817-2826.
47. Van ‘t Veer LJ, Dai H, Van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast
cancer. Nature 2002; 415: 530-536.
48. Wang Y, Klijn JG, Zhang Y, et al. Gene-expression profiles to predict distant metastasis of lymph-node-
negative primary breast cancer. Lancet 2005; 365: 671-679.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 171/248
Prognostic value of screen detection
185
9
Supplements Chapter 9
Supplementary Figure 1. Breast cancer-specific mortality in 953 women diagnosed with a
screen-detected carcinoma between 1990 and 2000. Kaplan–Meier curves for breast cancer-specific survival and the univariate hazard ratio (HR) with its 95% confidence interval (CI) for
prevalent versus incident carcinomas are shown.
Kaplan-Meier survival analysis, log-rank test, and univariate Cox proportional hazard ratio (HRs)
were calculated to estimate differences in survival among patients with prevalent carcinoma ( i.e.,
detected in the first screening round) and patients with incident carcinomas ( i.e., detected in a
second or subsequent screening round).
0.0
0.2
0.4
0.6
0.8
1.0
B r e a s t c a
n c e r - s p e c i fi c
s u r v i v a l p r o b a b i l i t y
0 5 10 15
Time (years)
510
443 15406 213
472 387 137
Incident carcinoma
Prevalent carcinomaNumbers at
risk
Prevalent versus incident carcinoma: HR = 1.02, 95% CI = 0.69 to 1.49
Log-rank p = 0.928

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 172/248
Chapter 9
186
Supplementary Table 1. Multivariable Cox proportional hazard regression analyses for breast
cancer-specific mortality in patients with breast cancer detected in the first screening round
(i.e., prevalent carcinoma) (n = 510) and patients with breast cancer detected in a second or
subsequent screening round (i.e., incident carcinoma) (n = 443)*.
Breast cancer-specific mortality
Characteristics P HR (95% CI)
Incident versus prevalent carcinoma 0.85 0.95 (0.58 to 1.56)
Period of diagnosis (1990–1996 versus 1997–2000) 0.01 0.87 (0.79 to 0.97)
Age (per year) 0.15 1.03 (0.99 to 1.06)
pT†
pT2 (versus pT1) 0.04 1.58 (1.02 to 2.46)
pT3 (versus pT1) 0.04 3.87 (1.04 to 14.32)
pN‡
pN1 (versus pN0) 0.09 1.71 (0.92 to 3.18)
pN2 (versus pN0) 0.002 2.83 (1.45 to 5.55)
pN3 (versus pN0) <0.001 6.21 (2.85 to 13.56)
Grade
II (versus I) 0.002 3.13 (1.51 to 6.49)
III (versus I) <0.001 5.90 (2.65 to 13.16)
Unknown (versus I) 0.41 1.47 (0.59 to 3.70)
ER status
ER negative (versus ER positive) 0.16 1.51 (0.85 to 2.69)
ER unknown (versus ER positive) 0.10 0.65 (0.40 to 1.08)
Chemotherapy (yes versus no) 0.81 0.92 (0.47 to 1.82)
Hormonal therapy (yes versus no) 0.58 0.86 (0.50 to 1.49)
* All statistics were calculated with the use of the Cox proportional hazard model. All statistical tests were
two-sided.
CI = confidence interval; ER = estrogen receptor; HR = hazard ratio.† pT = pT1 ≤ 2 cm; pT2 = 2–5 cm; pT3 > 5 cm. ‡ pN = pN0 = lymph node-negative; pN1 = 1–3 positive lymph
nodes; pN2 = 4–9 positive lymph nodes; pN3 > 9 positive lymph nodes.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 173/248
Prognostic value of screen detection
187
9
Supplementary Figure 2. Trends in the treatment of patients with adjuvant systemic therapy
in our study cohort of 2592 breast cancer patients aged 50 to 69 years, diagnosed between 1990
and 2000, stratified by nodal status.
CT = chemotherapy; HT = hormonal therapy.
100%
40%
60%
80%
0%
20%
100%
40%
60%
80%
0%
20%
P e r c e n t a g e r e c e i v i n g a d j u v a n t s y s t e m i c t r e a t m e n t
19901995
19941993
19921991
19961997
19981999
2000 1990 19951994199319921991 1996 1997 1998 1999 2000
Lymph node-negative Lymph node-positive
None
NoneCT
CTHT
HT
CT & HT
CT & HT
Year of diagnosis Year of diagnosis
A B

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 174/248
Chapter 9
188
Supplementary Table 2. Multivariable Cox proportional hazard regression analyses for breast
cancer-specific mortality in patients diagnosed between 1997 and 2001, including 180 patients
who were aged 70–75 years*.
Breast cancer-specific mortality
Characteristics P HR (95% CI)
Method of detection
Screen-detected versus nonscreening-related <0.001 0.49 (0.32 to 0.75)
Interval versus nonscreening-related 0.41 0.85 (0.57 to 1.26)
Age (per year) 0.006 1.04 (1.01 to 1.07)
pT†
pT2 (versus pT1) 0.01 1.62 (1.11 to 2.37)
pT3 (versus pT1) 0.05 2.02 (1.01 to4.04)
pN‡
pN1 (versus pN0) 0.005 1.99 (1.24 to 3.20)
pN2 (versus pN0) 0.009 2.16 (1.21 to 3.86)
pN3 (versus pN0) <0.001 5.90 (3.19 to 10.92)
Grade
II (versus I) 0.02 3.56 (1.28 to 9.93)
III (versus I) 0.002 5.61 (1.93 to 16.32)
Unknown (versus I) 0.20 2.28 (0.64 to 8.07)
ER status
ER negative (versus ER positive) 0.002 2.00 (1.28 to 3.11)
ER unknown (versus ER positive) 0.80 1.11 (0.51 to 2.42)
Chemotherapy (yes versus no) 0.66 1.11 (0.69 to 1.80)
Hormonal therapy (yes versus no) 0.42 1.20 (0.77 to 1.87)
* All statistics were calculated with the use of the Cox proportional hazard model. All statistical tests were
two-sided.
CI = confidence interval; ER = estrogen receptor; HR = hazard ratio.† pT = pT1 ≤ 2 cm; pT2 = 2–5 cm; pT3 > 5 cm. ‡ pN = pN0 = lymph node-negative; pN1 = 1–3 positive lymph
nodes; pN2 = 4–9 positive lymph nodes; pN3 > 9 positive lymph nodes.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 175/248
Prognostic value of screen detection
189
9
S u p p l e m e n t a r y T a b l e 3 . M u l t i v a r i a
b l e C o x p r o p o r t i o n a l h a z a r d r e g r e s s i o n a n a l y s e s f o r b r e a s t c a n c e r - s p e c i fi c m o r t a l i t y s t r a t i fi e d b y t u m o r s i z e * .
T u m o r s i z e o f ≤ 1 0 m m
T u m o r s i z e o f 1 1 – 2 0 m m
T u m o r
s i z e o f 2 1 – 3 0 m m
T u m o r s i z e
3 1 – 5 0 m m
C h
a r a c t e r i s t i c s
P
H R ( 9 5 % C
I )
P
H R ( 9 5 % C
I )
P
H R ( 9 5 % C
I )
P
H R ( 9 5 % C
I )
M e t h o d o f d e t e c t i o n : S c r e e n - d e t e c t e d
v e r s u s n o n s c r e e n i n g - r e l a t e d
0 . 0 4
0 . 3 5 ( 0 . 1 3 t o 0 . 9 6 )
0 . 1 0
0 . 7 4 ( 0 . 5 2 t o 1 . 0 5 )
0 . 0 0 2
0 . 5 3 ( 0 . 3 6 t o 0 . 7 9 )
0 . 0 8
0 . 5 7 ( 0 . 3 1 t o 1 . 0 7 )
A g
e ( p e r y e a r )
0 . 9 2
1 . 0 0 ( 0 . 9 3 t o 1 . 0 9 )
0 . 8 8
1 . 0 0 ( 0 . 9 7 t o 1 . 0 4 )
0 . 7 9
1 . 0 0 ( 0 . 9 8 t o 1 . 0 3 )
0 . 1 4
1 . 0 3 ( 0 . 9 9 t o 1 . 0 8 )
p N
† p N 1 ( v e r s u s p N 0 )
0 . 6 8
1 . 4 9 ( 0 . 2 3 t o 9 . 6 7 )
0 . 9 7
1 . 0 1 ( 0 . 5 8 t o 1 . 7 7 )
0 . 0 6
1 . 5 7 ( 0 . 9 8 t o 2 . 5 1 )
0 . 8 7
0 . 9 4 ( 0 . 4 2 t o 2 . 0 6 )
p N 2 ( v e r s u s p N 0 )
0 . 2 1
4 . 4 3 ( 0 . 4 3 t o 4 6 . 1 6 )
0 . 0 0 7
2 . 3 9 ( 1 . 2 7 t o 4 . 4 8 ) < 0 . 0 0 1
3 . 0 1 ( 1 . 7 7 t o 5 . 1 4 )
0 . 1 3
1 . 9 2 ( 0 . 8 3 t o 4 . 4 8 )
p N 3 ( v e r s u s p N 0 )
0 . 0 2
3 7 . 9 2 ( 1 . 7 5 t o 8 2 2 . 8 5 )
0 . 1 0
2 . 6 4 ( 0 . 8 4 t o 8 . 3 4 ) < 0 . 0 0 1
8 . 6 5 ( 4 . 6 0 t o 1 6 . 2 5 )
0 . 0 0 1
4 . 3 8 ( 1 . 8 5 t o 1 0 . 3 8 )
G r
a d e
I I ( v e r s u s I )
0 . 5 1
1 . 5 1 ( 0 . 4 5 t o 5 . 0 9 )
0 . 0 0 9
2 . 3 3 ( 1 . 2 4 t o 4 . 3 9 )
0 . 2 0
1 . 7 5 ( 0 . 7 5 t o 4 . 0 7 )
0 . 6 9
1 . 5 2 ( 0 . 2 0 t o 1 1 . 6 8 )
I I I ( v e r s u s I )
0 . 6 9
1 . 5 4 ( 0 . 1 9 t o 1 2 . 2 6 ) <
0 . 0 0 1
5 . 9 1 ( 3 . 0 2 t o 1 1 . 5 7 )
0 . 0 1
3 . 1 3 ( 1 . 3 2 t o 7 . 4 1 )
0 . 3 7
2 . 5 3 ( 0 . 3 3 t o 1 9 . 1 4 )
U n k n o w n ( v e r s u s I )
0 . 3 8
1 . 8 4 ( 0 . 4 8 t o 7 . 1 1 )
0 . 0 0 2
2 . 9 7 ( 1 . 4 7 t o 6 . 0 1 )
0 . 0 5
2 . 4 4 ( 1 . 0 1 t o 5 . 8 9 )
0 . 4 1
2 . 3 5 ( 0 . 3 1 t o 1 8 . 0 3 )
E R
s t a t u s
E R n e g a t i v e ( v e r s u s E R p o s i t i v e )
0 . 6 6
1 . 4 6 ( 0 . 2 7 t o 7 . 8 0 )
0 . 4 8
1 . 2 1 ( 0 . 7 2 t o 2 . 0 4 )
0 . 3 8
1 . 2 5 ( 0 . 7 6 t o 2 . 0 6 )
0 . 2 5
1 . 4 9 ( 0 . 7 5 t o 2 . 9 5 )
E R u n k n o w n ( v e r s u s E R p o s i t i v e )
0 . 4 9
0 . 6 8 ( 0 . 2 3 t o 2 . 0 5 )
0 . 1 3
1 . 3 5 ( 0 . 9 2 t o 1 . 9 7 )
0 . 8 1
1 . 0 4 ( 0 . 7 3 t o 1 . 4 9 )
0 . 2 1
1 . 4 1 ( 0 . 8 3 t o 2 . 4 1 )
C h
e m o t h e r a p y ( y e s v e r s u s n o )
0 . 6 7
1 . 5 3 ( 0 . 2 2 t o 1 0 . 8 4 )
0 . 8 1
0 . 9 2 ( 0 . 4 8 t o 1 . 7 7 )
0 . 0 3
0 . 5 5 ( 0 . 3 2 t o 0 . 9 4 )
0 . 1 6
0 . 5 6 ( 0 . 2 6 t o 1 . 2 5 )
H o
r m o n a l t h e r a p y ( y e s v e r s u s n o )
0 . 6 4
0 . 6 7 ( 0 . 1 3 t o 3 . 4 9 )
0 . 9 3
0 . 9 8 ( 0 . 5 9 t o 1 )
0 . 3 4
0 . 8 0 ( 0 . 5 1 t o 1 . 2 6 )
0 . 0 7
0 . 5 5 ( 0 . 2 9 t o 1 . 0 5 )
* A l l s t a t i s t i c s w e r e c a l c u l a t e d u s i n g t h e
C o x p r o p o r t i o n a l h a z a r d m o d e l a n d
w e r e t w o - s i d e d .
C I =
c o n fi d e n c e i n t e r v a l ; E R = e s t r o g e n r
e c e p t o r ; H R = h a z a r d r a t i o .
† p N : p N 0 = l y m p h n o d e - n e g a t i v e ; p N 1
= 1 – 3 p o s i t i v e l y m p h n o d e s ; p N 2 = 4
– 9 p o s i t i v e l y m p h n o d e s ; p N 3 > 9 p o
s i t i v e l y m p h n o d e s .

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 176/248
Chapter 9
190
0.0
0.2
0.4
0.6
0.8
1.0
B r e a s t c a n c e r - s p e c i fi c
s u r v i v a l p r o b a b
i l i t y
0 5 10 15
Time (years)
238
116 36109 72
225 163 46
Nonscreening-related
Screen-detectedNumbers at
risk
Screen-detectedversus nonscreening-related: HR = 0.28, 95% CI = 0.11 to 0.71
Log-rank p = 0.004
0.0
0.2
0.4
0.6
0.8
1.0
B r e a s t c a n c e r - s p e c i fi c
s u r v i v a l p
r o b a b i l i t y
0 5 10 15
Time (years)
476
484 139432 320
450 305 74
Nonscreening-related
Screen-detectedNumbers at
risk
Screen-detectedversus nonscreening-related: HR = 0.63, 95% CI = 0.45 to 0.90
Log-rank p = 0.009
A
B

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 177/248
Prognostic value of screen detection
191
9
0.0
0.2
0.4
0.6
0.8
1.0
B r e a s t c a n c e r - s p e c i fi c
s u r v i v a l p r o b a b
i l i t y
0 5 10 15
Time (years)
164
384 89290 204
144 90 19
Nonscreening-related
Screen-detectedNumbers at
risk
Screen-detectedversus nonscreening-related: HR = 0.60, 95% CI = 0.41 to 0.87
Log-rank p = 0.007
0.0
0.2
0.4
0.6
0.8
1.0
B r e a s t c a n c e r - s p e c i fi c
s u r v i v a l
p r o b a b i l i t y
0 5 10 15
Time (years)
55
172 35128 82
41 31 10
Nonscreening-related
Screen-detectedNumbers at
risk
Screen-detectedversus nonscreening-related: HR = 0.58, 95% CI = 0.32 to 1.05
Log-rank p = 0.07
C
D

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 178/248
Chapter 9
192
Supplementary Figure 3. Breast cancer-specific survival by method of detection. Kaplan–Meier
curves for breast cancer-specific survival and univariate hazard ratios (HRs) for breast cancer-
specific mortality.
A) Patients with tumors of 10 mm or less.
B) Patients with tumors of 11–20 mm.
C) Patients with tumors of 21–30 mm.
D) Patients with tumors of 31–50 mm.
0.0
0.2
0.4
0.6
0.8
1.0
B r e a s t c a n c e r - s p e c i fi c
s u r v i v a l p r o b a
b i l i t y
0 5 10 15
Time (years)
635
567 164503 362
608 430 118
Nonscreening-related
Screen-detectedNumbers at
risk
Screen-detectedversus nonscreening-related: HR = 0.40, 95% CI = 0.28 to 0.56
Log-rank p < 0.001
0.0
0.2
0.4
0.6
0.8
1.0
B r e a s t c a n c e r - s p e c i fi c
s u r v i v a l p r o b a b i l i t y
0 5 10 15
Time (years)
323
650 147501 345
275 172 34
Nonscreening-related
Screen-detectedNumbers atrisk
Screen-detectedversus nonscreening-related: HR = 0.59, 95% CI = 0.45 to 0.79
Log-rank p = 0.001
E
E

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 179/248
Prognostic value of screen detection
193
9
E) Patients with lymph node-negative breast cancer.
F) Patients with lymph node-positive breast cancer.
NRS = Non-screening-related carcinomas, symptomatic cancer in patients who had not been
screened or were screened more than 24 months before detection of breast cancer. SD = Screen-
detected carcinomas.
The number of patients at risk is shown below each graph. For 32 patients, no exact tumor size
was available (only pT stage), and so they were excluded from the analyses shown in Figure
3, A–D. Kaplan-Meier survival analyses, log-rank tests, and univariate Cox proportional hazard
ratios (HRs) were calculated to estimate differences in survival among patients with screen-
detected carcinoma and patients with non-screening-related carcinoma.
Supplementary Table 4. Multivariable Cox proportional hazard regression analyses for breast
cancer-specific mortality stratified by lymph node status*.
Lymph node-negative Lymph node-positive
Characteristics P HR (95% CI) P HR (95% CI)
Method of detection: screen-detected
versus non-screening-related<0.001 0.51 (0.36 to 0.73) 0.12 0.79 (0.59 to 1.06)
Age (per year) 0.26 1.02 (0.99 to 1.05) 0.77 1.00 (0.98 to 1.03)
pT†
pT2 (versus pT1) <0.001 1.87 (1.32 to 2.65) <0.001 2.00 (1.51 to 2.67)
pT3 (versus pT1) 0.08 3.62 (0.88 to 14.95) 0.009 2.05 (1.20 to 3.49)
Grade
Grade II (versus grade I) 0.002 2.45 (1.38 to 4.35) 0.05 1.98 (0.99 to 3.94)
Grade III (versus grade I) <0.001 4.08 (2.11 to 7.87) <0.001 4.62 (2.31 to 9.25)
Grade unknown (versus grade I) <0.001 3.35 (1.82 to 6.16) 0.001 3.19 (1.57 to 6.49)
ER status
ER negative (versus ER positive) 0.26 1.36 (0.80 to 2.32) 0.18 1.29 (0.89 to 1.88)
ER unknown (versus ER positive) 0.30 0.82 (0.57 to 1.19) 0.02 1.38 (1.05 to 1.81)
Chemotherapy (yes versus no) 0.90 1.06 (0.45 to 2.46) 0.15 0.75 (0.50 to 1.11)
Hormonal therapy (yes versus no) 0.20 0.76 (0.49 to 1.16) 0.70 0.92 (0.62 to 1.38)
* All statistics were calculated using the Cox proportional hazard model and were two-sided.
CI = confidence interval; ER = estrogen receptor; HR = hazard ratio.
† pT: pT1 ≤ 2 cm; pT2 = 2–5 cm; pT3 > 5 cm.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 180/248
Chapter 9
194
Supplementary Table 5. Adjuvant! 10-year observed and predicted breast cancer-specific
survival for patients younger than 50 years by period of diagnosis*.
10-year breast cancer-specific survival
Period of diagnosisNo. patients
(%)
Adjuvant!
predicted, %
Observed,
% (95% CI)
Predicted –
observed P
1990–1996 1381 (70.0) 77.3 77.5 (75.3 to 79.7) 0.2 0.86
1997–2000 592 (30.0) 79.3 82.3 (79.2 to 85.4) -3.0 0.06
* All statistics were calculated by one sample t tests and were two-sided.
CI = confidence interval.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 181/248
Chapter 10
General discussion
and future prospects

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 182/248
Chapter 10
198

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 183/248
Discussion & future prospects
199
10
Over the last decades, breast cancer management has changed dramatically. Primary local
treatment has evolved from the extensive Halsted mastectomy to less invasive breast
conservative surgery followed by radiotherapy, which is currently the standard treatment
for approximately 2/3 of the breast cancer patients.1 In addition, staging of the axilla by
the sentinel node procedure is now widely practiced and the standard of care for patients
with clinically negative nodal status.2,3 Patients with a negative sentinel node can be spared
complete axillary lymph node dissection and its associated side-effects.4,5 The final analysis
of the AMAROS trial show will show whether in case of sentinel lymph node involvement
axillary lymph node dissection can be abandoned and radiotherapy of the axilla provides a
safe and equivalent alternative with less morbidity. In the meantime, even more provocative
results of the ASCO Z0011 trial by Giuliano and colleagues were published.6 Patients with
invasive breast carcinomas ≤ 5 cm treated with breast conserving therapy and adjuvant
systemic therapy (in 96% of the patients) who had 1-3 positive sentinel nodes were
randomized between axillary lymph node dissection and no further axillary treatment.
Remarkably, no difference in local and regional recurrence was observed, suggesting that
for a selected group of patients with macrometastases in the sentinel lymph node further
axillary treatment can be safely omitted.
All the above mentioned changes in breast cancer management touch upon the ultimate
goal to optimize and tailor treatment by reducing side-effects without jeopardizing
survival and were guided by a conceptual change in the theory on breast cancer
etiology and progression.7 Traditionally, breast cancer management was based on the
Halsted theory. Halsted stated that breast cancer is a localized disease, spreading in anorderly and consecutive manner from local tissue, to regional lymph nodes and then to
distant sites.8 This theory justified the use of extensive loco-regional surgery (i.e. radical
mastectomy) to remove all local and regional disease, thereby improving survival. In 1968,
Fisher introduced an alternative hypothesis, which has led to a number of changes in
breast cancer management.9,10 Fisher postulated that breast cancer is primarily a systemic
disease, with the presence of circulating cancer cells already at an early stage, thus requires
treatment of the entire patient (systemic treatment). As a consequence, according to the
Fisher theory, local recurrence should be considered an indicator of metastatic disease, and
the development of distant metastases is a result of both tumor and patient characteristicsand the interaction between them. This hypothesis and the knowledge of the incurable
nature of metastatic breast cancer with the emanating fear of undertreatment have caused
a substantial increase in the use of adjuvant systemic therapy.11,12,13

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 184/248
Chapter 10
200
Selection of patients for adjuvant systemic therapy; current practice
Currently, guidelines recommend adjuvant systemic therapy (AST) for all patients with
lymph node positive disease and for over 80% of breast cancer patients with lymph node
negative disease. 13,14 These guidelines base their recommendations for the use of AST
on clinicopathological prognostic characteristics, such as age, tumor size, tumor grade,
lymph node status and estrogen receptor status. 14-17 These clinicopathological factors are
used to identify subgroups of patients with a poor prognosis who are expected to benefit
more from adjuvant systemic therapy. However, many patients in these subgroups are
overtreated since they do not have micrometastases at diagnosis and thus are likely to
remain free from distant metastases.18 This overtreatment is particularly poignant in lymph
node negative breast cancer where over 80% is treated with AST, whereas approximately
70% of the patients are free of distant metastases at 10 years and likely to be cured with
locoregional treatment alone.18 Conversely, patient selection based on clinicopathological
criteria can also cause undertreatment. According to some current guidelines, AST is often
not recommended for patients with small tumors of less than 1 cm; however, a proportion of
these small tumors may have spread before detection and should consequently be treated
with AST. It is clear that patients who suffer from an apparently similar tumor with regard
to pathological characteristics can have remarkably different disease outcomes. Therefore,
patient selection for adjuvant systemic therapy by traditional prognostic factors has its
limitations and will lead to both over- and undertreatment. Breast cancer treatment with
as little as possible side effects and optimal survival requires a patient-tailored approachbased on appropriate patient selection. This shift from a ‘one size fits all’ approach to a more
personalized approach uncovers the need for better prognostic markers or tools in breast
cancer and is the rational for this thesis.
Multigene prognosis signatures
The introduction of high-throughput microarray technology facilitated the development of
gene-expression profiles or signatures that can measure the expression of multiple genesin a single test.19-21 The 70-gene prognosis signature (MammaPrint™) is one of the new
prognostic markers that can accurately discriminate between breast cancer patients at low
and high risk of developing distant metastases, based on the expression level of 70 selected
genes.22 Validation studies confirmed that the signature can accurately predict disease
outcome in premenopausal, lymph node negative breast cancer patients.23,24 In addition,
the prognostic value of the signature was independent of known clinicopathological
prognostic factors.23-27 These studies, as well as studies described in this thesis have led to
the inclusion of the 70-gene signature in current guidelines.14,15 Soon after the development
of the 70-gene signature, the Recurrence Score (OncotypeDX™) was developed and

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 185/248
Discussion & future prospects
201
10
validated.28-31 This test classifies tumors based on the expression of 16 genes into a low
Recurrence Score (RS), an intermediate RS or a high RS. The RS has been validated in several
patient series and has been incorporated into the St. Gallen recommendations and NCCN
guidelines.15,32 The recently conducted Trial Assigning IndividuaLized Options for Treatment
(Rx) (TAILORx), will address whether patients who are assigned to the intermediate RS have
benefit from adjuvant chemotherapy in addition to endocrine therapy. Patient inclusion for
the TAILORx was finished end 2010.33
Prognostic value of the 70-gene signature in breast cancer subgroups
For the studies presented in this thesis independent retrospective patient series were
selected to assess the prognostic value of the 70-gene signature in postmenopausal breast
cancer patients and in patients with 1-3 positive lymph nodes. For the validation of the
signature in small tumors patients were selected from a pooled database of previously
published studies and studies described in chapter 4 and 5 of this thesis.23-25,34,35
The majority of breast cancer patients are postmenopausal women.36 Although former
treatment guidelines recommended adjuvant endocrine therapy only, there is a strong
increase in the use of chemotherapy for postmenopausal patients.37-39 This more extensive
use of adjuvant treatment is intuitively in contrast to the more favorable tumor characteristics
and good disease outcome observed in many postmenopausal patients.37-39 Besides, the
overview data show that the benefit of chemotherapy diminishes as age increases.18 Inaddition, the benefit of chemotherapy in postmenopausal patients seems to occur mainly
in the first five years.18 In chapter 4 we show that even though the 70-gene signature was
developed in premenopausal patients, it has independent prognostic value and utility
in postmenopausal women. The signature identified poor prognosis patients who are at
high risk of developing distant metastases early in the disease course and are therefore
likely to benefit more from chemotherapy. Postmenopausal patients who were classified
as low risk were likely to remain free of early disease recurrence; however, a proportion of
those low risk patients did develop late metastases. This low risk subgroup consisted of
estrogen receptor positive tumors and only 1 patient received endocrine therapy. Sincethe beneficial effect of chemotherapy in postmenopausal patients is limited to the first five
years, patients classified as low risk who are at risk of late breast cancer related events are
more likely to benefit from endocrine therapy.
Historically, lymph node status is considered to be the most powerful prognostic factor
in breast cancer, with the presence and number of involved nodes being associated with
poor disease outcome.40-42 As a consequence, patients with lymph node positive disease
are currently offered chemotherapy, regardless of other clinicopathological characteristics.
However, a subset of patients (approximately 25-30%) will remain free of distant metastases
for at least 10 years without AST and are presumably cured by locoregional treatment

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 186/248
Chapter 10
202
alone.18,43 So far, no prognostic factor that can identify this subset of good prognosis lymph
node positive patients has been identified. New prognostic markers or signatures will only
have medical utility when they can identify a clinically relevant subset of patients with
potential treatment consequences. For example, the identification of a subset of patients
who have a low risk of recurrence will only be relevant when the risk is sufficiently small
to justify withholding chemotherapy. In chapter 5 we have demonstrated that the 70-
gene signature was able to identify a subset of patients with 1-3 positive lymph nodes
who are at sufficiently low risk to consider withholding chemotherapy. The appreciation
of the existence of low risk lymph node positive patients who might not benefit from
chemotherapy was also confirmed for the Recurrence Score by Albain and colleagues. 28
Based on these results the currently conducted randomized MINDACT trial has extended
its eligibility criteria to patients with up to 3 positive nodes. Results of this prospective
trial might end the long existing and persistent idea that all patients with lymph node
involvement will be confronted with metastatic disease and should receive adjuvant
chemotherapy.
In addition to lymph node status, tumor size is a traditional prognostic factor that is taken
into account when selecting patients for adjuvant systemic therapy. 40-42 Current guidelines
are inconsistent in the systemic treatment recommendations for patients with small breast
tumors.14,15,17,32 In the study described in chapter 6 we show that the 70-gene signature can
select patients with pT1c tumors (pT1c: 11-20cm) who are at low risk of distant recurrence
and therefore could be safely spared chemotherapy. Moreover, the 70-gene signature
could identify patients with small breast tumors (pT1ab ≤10mm) who do have a substantialrisk of developing distant metastases despite the small tumor size. The above mentioned
results support the Fisher hypothesis that metastatic capacity is an early inheritance, and
that lymph node involvement is an indicator and not instigator of distant disease.9,44 In
addition, our studies suggest that the metastatic capacity depends (at least partially) on
the genetic makeup of a tumor and thus can be identified by the measurement of tumor
gene expression.
Retrospective validation
Retrospective studies are of indispensable value to identify potential biomarkers that
deserve further evaluation; however, there are some drawbacks that one needs to be aware
of.
In retrospective series that were not part of a randomized trial, patients have received
treatment according to the guidelines present at that time. Therefore, clinicopathological
markers will have influenced treatment decision, which will complicate extrapolation of
the results. However, recommendations for the use of adjuvant systemic therapy in the
Netherlands have been conservative for a long time, as described in the introduction of

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 187/248
Discussion & future prospects
203
10
this thesis.14,45,46 As a result, retrospective series of Dutch breast cancer patients who were
diagnosed before 2000 will consist of a relatively large proportion of untreated patients.
For instance, the first validation study of the 70-gene signature included a true consecutive
series of lymph node negative patients of whom only 10% received AST.24 In addition, the
postmenopausal patient series described in chapter 4 was a true consecutive series and
no patients were excluded because of chemotherapy treatment. One might argue that the
prognostic value of a marker cannot be assessed in a (partially) treated population. However,
selecting patients who did not receive adjuvant systemic therapy will introduce selection
bias. Markers that can define the residual risk of recurrence when a patient will be treated
with endocrine therapy alone are of utmost importance in determining the potential value
and necessity of additional chemotherapy. Including patients who have only received
adjuvant endocrine therapy seems to be a reasonable compromise. The evaluation of the
70-gene signature in postmenopausal patients (chapter 4) was performed in a consecutive
series of patients who did not receive AST or were only treated with endocrine therapy.
The Recurrence Score (OncotypeDX™) provides an estimate of the additive effect of adjuvant
chemotherapy in combination with 5 years of endocrine treatment with Tamoxifen.28-31
However, for patients who are assigned to the intermediate RS, the additional benefit of
chemotherapy remains uncertain while having a considerable risk of recurrence and result
of the TAILORx needs to be awaited.33
To avoid selection bias as mentioned above, we included patients with lymph node positive
disease regardless of adjuvant systemic therapy for the validation study described in
chapter 5. As a consequence, 56% of the patients received adjuvant chemotherapy. Thesepatients had more often estrogen receptor negative and poorly differentiated tumors, which
in general are believed to have more benefit from chemotherapy.18 In addition, patients
treated with chemotherapy were more often classified as poor prognosis by the 70-gene
signature. In the study presented in chapter 7, we analyzed 541 patients who had received
adjuvant systemic therapy and who were classified by the 70-gene signature. Patients with
a 70-gene poor prognosis signature treated with chemotherapy followed by endocrine
therapy had a significantly better distant disease-free survival compared with poor
prognosis patients who were treated with endocrine therapy alone. Conversely, patients
with a low risk 70-gene signature who were treated with chemotherapy and endocrinetherapy had similar disease outcomes as low risk patients treated with endocrine therapy
alone. This study provides evidence that patients with a high risk 70-gene signature are
more likely to benefit from adjuvant chemotherapy, whereas a low risk 70-gene signature
indicates limited benefit from adjuvant chemotherapy, in addition to a low recurrence
risk to begin with. Additionally, in a recently published study the predictive value of the
70-gene signature was assessed in patients treated with neoadjuvant chemotherapy.47
Although patients included in this study were considered as clinically high risk patients
(95% of the tumors were > 2 cm and 72% had lymph node positive disease), the 70-gene
signature identified 14% good prognosis tumors. Among patients with a good prognosis

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 188/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 189/248
Discussion & future prospects
205
10
bank for future research, including proteomics, temporarily preservation of tissue in
preservation fluid might not be suitable and fresh frozen tissue is probably a more reliable
source for future research. Therefore we conducted a pilot study preceding the MINDACT
trial, in which we have tested and optimized the comprehensive logistics to obtain good-
quality fresh frozen tumor tissue (chapter 3). The feasibility of performing gene expression
profiling in daily practice is further reflected by the fast accrual of the MINDACT trial.50

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 190/248
Chapter 10
206
Clinicopathological risk assessment and individualized prognostication
The prognostic tool Adjuvant!
In the MINDACT trial, the clinicopathological risk will be assessed by Adjuvant! to provide an
internationally used and standardized method for predicting outcome. Adjuvant! predicts
10 year disease outcome with and without the use of adjuvant systemic therapy based
on age, co-morbidity, tumor size, tumor grade, estrogen receptor status and lymph node
status.16 The model was developed in an American breast cancer population and previously
validated in Canadian breast cancer patients.16,51 In chapter 8 a Dutch validation study of
the model is described. The results show that in general Adjuvant! can be used for Dutch
breast cancer patients; however, predictions in patients under 40 years should be carefully
judged. In this validation study we assessed both the accuracy of the model to predict
disease outcome in subgroups of breast cancer patients (i.e. the goodness of fit or calibration)
and the model’s ability to distinguish individuals who will experience different outcomes
(discriminatory accuracy). In the era of personalized treatment, the discriminatory accuracy
of a prognostic tool or marker is of paramount importance.52-54 A model can predict disease
outcome very accurately in the whole group or in clinically relevant subgroups, without
identifying the correct patients who are at high risk of recurrence. For instance, when 30%
of the patients will suffer from recurrence and the model indeed predicts a recurrence
of 30% in this group, its calibration is excellent. However, the model could still identify
the wrong patients as poor prognosis as is depicted in figure 1, hence resulting in a poordiscriminatory accuracy and limited value for the individual patient. In addition to the
good calibration of the Adjuvant! tool in Dutch patients (differences between predicted
and observed outcomes were within 2% for most clinically relevant subgroups), the model
showed moderate discriminatory accuracy. This observation was expected since we know
that patients with identical clinicopathological characteristics can have different outcomes.
Consequently, the prognostic information that is captured by these characteristics can
only explain part of the differences in outcome. Considering the results described in this
thesis, the 70-gene signature as a measurement of tumor biology will be the most obvious
marker to incorporate in the Adjuvant! model. The signature will probably explain part ofthe residual variation and increase the discriminatory accuracy of the model and therefore
could provide the opportunity to improve personalized treatment. In addition, other
(new) prognostic factors could be added to the model and potentially improve outcome
prediction, such as Her2 status or Ki67.55,56 In the MINDACT trial, an adapted version of
Adjuvant! including Her2 is used.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 191/248
Discussion & future prospects
207
10
Figure 1. Calibration and discriminatory accuracy of a hypothetical prognostic marker.
The predicted distant metastases-free survival of 70% is in good agreement with the actual
observed DMFS of 70%, reflecting the good calibration of the marker. However, the 30% who
were identified by the prognostic marker as patients who are at risk of developing distantmetastases are completely different from the patients in whom distant metastases were
observed, depicting the poor discriminatory accuracy.
The white figures represent patients who were predicted to remain free of distant metastases
by the marker and/or in whom no distant metastases were observed. The gray figures represent
patients who are predicted to develop metastases according to a prognostic marker. The black
and white striped figures are patients in whom distant metastases were observed.
Method of detection
A new marker that is currently ignored when selecting patients for AST is method of
detection, i.e. whether a tumor is detected by screening mammography or by the cause
of symptoms. Adding method of detection to models such as Adjuvant! could improve
the individual prediction of disease outcome. In chapter 9 we show that Adjuvant!
underestimated disease outcome in patients with screen-detected tumors. Furthermore,
results of our study show that, even after adjusting for factors associated with tumor
advancement and aggressiveness, patients with screen-detected tumors have a better
survival compared with patients with nonscreening-related tumors. This suggests that
Group level: Good calibration
Individual patient level: poor discriminatory accuracy
Predicted outcome Observed outcome

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 192/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 193/248
Discussion & future prospects
209
10
value seems limited since the vast majority of these patients will be classified as high risk
according to the signature.
Future prospective
The introduction of microarray technology will increasingly impact the management of
breast cancer. It will increase our understanding about breast cancer biology and further
elucidate its heterogeneity. The studies described in this thesis show that the 70-gene
signature, which was developed in a well-defined subset of breast cancer patients, has
prognostic value in several other breast cancer subgroups, suggesting that one prognostic
test fits all patients. However, there is still room for improvement and with the currently
increasing knowledge about tumor biology it is likely that new markers will be developed
in more specific subgroups, such as in estrogen receptor negative or triple negative
tumors. In the future we might be able to perform one assay in a certain subgroup in
order to determine a patient’s prognosis but also the likelihood of response to different
therapies and the presence of drug targets. These developments will also influence clinical
trial design, in which patients will be stratified by both prognostic and predictive markers,
thereby identifying targeted therapy that will be highly effective in a (small) subgroup of
patients who indeed need additional systemic treatment.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 194/248
Chapter 10
210
Reference List
1. Veronesi U, Saccozzi R, Del VM, et al. Comparing radical mastectomy with quadrantectomy, axillary
dissection, and radiotherapy in patients with small cancers of the breast. N Engl J Med 1981; 305: 6-11.
2. Veronesi U, Viale G, Paganelli G, et al. Sentinel lymph node biopsy in breast cancer: ten-year results of a
randomized controlled study. Ann Surg 2010; 251: 595-600.
3. Veronesi U, Paganelli G, Viale G, et al. A randomized comparison of sentinel-node biopsy with routine
axillary dissection in breast cancer. N Engl J Med 2003; 349: 546-553.
4. Bergkvist L, de Boniface J, Jonsson PE, et al . Axillary recurrence rate after negative sentinel node biopsy
in breast cancer: three-year follow-up of the Swedish Multicenter Cohort Study. Ann Surg 2008; 247: 150-
156.
5. Giuliano AE, Haigh PI, Brennan MB, et al. Prospective observational study of sentinel lymphadenectomy
without further axillary dissection in patients with sentinel node-negative breast cancer. J Clin Oncol 2000;
18: 2553-2559.
6. Giuliano AE, McCall L, Beitsch P, et al. Locoregional recurrence after sentinel lymph node dissection with
or without axillary dissection in patients with sentinel lymph node metastases: the American College
of Surgeons Oncology Group Z0011 randomized trial. Ann Surg 2010; 252: 426-432.
7. della Rovere GQ and Benson JR. Ipsilateral local recurrence of breast cancer: determinant or indicator
of poor prognosis? Lancet Oncol 2002; 3: 183-187.
8. Halsted WS. I. The results of operations for the cure of cancer of the breast performed at the Johns
Hopkins Hospital from June, 1889, to January, 1894. Ann Surg 1894; 20: 497-555.
9. Fisher B. The evolution of paradigms for the management of breast cancer: a personal perspective.
Cancer Res 1992; 52: 2371-2383.
10. Fisher B and Anderson SJ. The breast cancer alternative hypothesis: is there evidence to justify replacing
it? J Clin Oncol 2010; 28: 366-374.
11. Van Steenbergen LN, Van de Poll-Franse LV, Wouters MW, et al . Variation in management of early breast
cancer in the Netherlands, 2003-2006. Eur J Surg Oncol 2010; 36 Suppl 1: S36-S43.
12. Sukel MP, van de Poll-Franse LV, Nieuwenhuijzen GA, et al . Substantial increase in the use of adjuvant
systemic treatment for early stage breast cancer reflects changes in guidelines in the period 1990-2006
in the southeastern Netherlands. Eur J Cancer 2008; 44: 1846-1854.
13. Harlan LC, Clegg LX, Abrams J, Stevens JL, Ballard-Barbash R. Community-based use of chemotherapyand hormonal therapy for early-stage breast cancer: 1987-2000. J Clin Oncol 2006; 24: 872-877.
14. CBO Richtlijn Mammacarcinoom 2008. http://www.cbo.nl/product/richtlijnen/folder20021023121843/rl_mamma_08.pdf.
15. Goldhirsch A, Ingle JN, Gelber RD, et al . Thresholds for therapies: highlights of the St. Gallen International
Expert Consensus on the primary therapy of early breast cancer 2009. Ann Oncol 2009; 20:1319–1329.
16. Ravdin PM, Siminoff LA, Davis GJ, et al. Computer program to assist in making decisions about adjuvant
therapy for women with early breast cancer. J Clin Oncol 2001; 19: 980-991.
17. Todd JH, Dowle C, Williams MR, et al. Confirmation of a prognostic index in primary breast cancer. Br J
Cancer 1987; 56: 489-492.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 195/248
Discussion & future prospects
211
10
18. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for
early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet
2005; 365: 1687-1717.
19. Brown PO and Botstein D. Exploring the new world of the genome with DNA microarrays. Nat Genet 1999;
21: 33-37.
20. DeRisi J, Penland L, Brown PO, et al. Use of a cDNA microarray to analyse gene expression patterns in
human cancer. Nat Genet 1996; 14: 457-460.
21. Schena M, Shalon D, Davis RW, Brown PO. Quantitative monitoring of gene expression patterns with a
complementary DNA microarray. Science 1995; 270: 467-470.
22. Van ‘t Veer LJ, Dai H, Van de Vijver MJ, et al . Gene expression profiling predicts clinical outcome of breast
cancer. Nature 2002; 415: 530-536.
23. Buyse M, Loi S, Van ‘t Veer L, et al . Validation and clinical utility of a 70-gene prognostic signature for
women with node-negative breast cancer. J Natl Cancer Inst 2006; 98: 1183-1192.
24. Van de Vijver MJ, He YD, Van ‘t Veer LJ, et al . A gene-expression signature as a predictor of survival in
breast cancer. N Engl J Med 2002; 347: 1999-2009.
25. Bueno de Mesquita JM, Linn SC, Keijzer R et al. Validation of 70-gene prognosis signature in node-
negative breast cancer. Breast Cancer Res Treat 2009; 117: 483–495.
26. Ishitobi M, Goranova TE, Komoike Y, et al . Clinical utility of the 70-gene MammaPrint profile in a Japanese
population. Jpn J Clin Oncol 2010; 40: 508-512.
27. Wittner BS, Sgroi DC, Ryan PD, et al. Analysis of the MammaPrint breast cancer assay in a predominantly
postmenopausal cohort. Clin Cancer Res 2008; 14: 2988-2993.
28. Albain KS, Barlow WE, Shak S, et al . Prognostic and predictive value of the 21-gene recurrence score
assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on
chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol 2010; 11: 55-65.
29. Habel LA, Shak S, Jacobs MK, et al. A population-based study of tumor gene expression and risk of breast
cancer death among lymph node-negative patients. Breast Cancer Res 2006; 8: R25.
30. Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative
breast cancer. N Engl J Med 2004; 351: 2817-2826.
31. Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-
negative, estrogen receptor-positive breast cancer. J Clin Oncol 2006; 24: 3726-3734.
32. NCCN Clinical Practice Guidelines in Oncology. Breast Cancer V.1.2009. www.nccn.org 2009.33. National Cancer Institute The TAILORx Breast Cancer Trial Available at: http://www.cancer.gov/
clinicaltrials/digestpage/TAILORx.
34. Bueno de Mesquita JM, Van Harten WH, Retel VP, et al . Use of 70-gene signature to predict prognosis of
patients with node-negative breast cancer: a prospective community-based feasibility study (RASTER).
Lancet Oncol 2007; 8: 1079-1087.
35. Kok M, Koornstra RH, Mook S, et al. Additional value of the 70-gene signature and levels of ER and PR for
the prediction of outcome in tamoxifen-treated ER-positive breast cancer. Submitted.
36. Ries LAG, Melbert D, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2005 , National Cancer Institute. Bethesda,
MD. http://seer.cancer.gov/csr/1975_2005/, based on November 2007 SEER data submission, posted to
the SEER web site.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 196/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 197/248
Discussion & future prospects
213
10
55. Harris L, Fritsche H, Mennel R, et al. American Society of Clinical Oncology 2007 update of
recommendations for the use of tumor markers in breast cancer. J Clin Oncol 2007; 25: 5287-5312.
56. Soerjomataram I, Louwman MW, Ribot JG, Roukema JA, Coebergh JW. An overview of prognostic
factors for long-term survivors of breast cancer. Breast Cancer Res Treat 2008; 107: 309-330.
57. Knauer M, Cardoso F, Wesseling J, et al. Identification of a low-risk subgroup of HER-2-positive breast
cancer by the 70-gene prognosis signature. Br J Cancer 2010; 103: 1788-1793.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 198/248
Chapter 11
Summary

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 199/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 200/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 201/248
Chapter 11
218
clinicopathological criteria (adjusted hazard ratio (HR) for distant metastases as a first event
was 4.6; 95% confidence interval (CI) 2.3–9.2; p < 0.001). These results were confirmed by
a second and independent validation study in 302 lymph node negative patients who did
not receive AST and were diagnosed in 5 European hospitals. Furthermore, the so-called
RASTER (MicroarRAy PrognoSTics in Breast CanceR) study, showed the feasibility of using
the signature for adjuvant treatment decision-making in 16 community based hospitals in
the Netherlands. In a European pilot study, which is also described in detail in chapter 3,
the logistics for the prospective MINDACT (Microarray In Node-negative and 1-3 positive
lymph node disease may Avoid ChemoTherapy) study were tested and optimized. This
study showed that it is feasible to collect good quality fresh frozen tissue in different
European hospitals and that frozen samples can be shipped to a central microarray facility
on a real-time basis. The success rate of the 70-gene signature was 77% (46/60) when
a tumor sample could be obtained. The main reason for exclusion from profiling was a
non-representative sample of the tumor; 18% (11/60) of the samples contained < 50%
tumor cells. Based on these results and the experience gained in this pilot study standard
operating procedures, which are currently used in the MINDACT trial, were developed. The
prospective MINDACT trial is discussed in more detail in the appendix of this thesis. This
international randomized trial will evaluate whether patients who are considered high
risk according to the currently available prognostic tool Adjuvant! but classified as low
risk by the 70-gene signature can be spared chemotherapy without jeopardizing disease
outcome. Recruitment of the trial is anticipated to be completed mid 2011.
Up to now, the 70-gene signature has been developed and validated in a selected group
of patients: predominantly premenopausal patients with lymph node negative disease.
In order to assess the potential improvement of prognostication by using the 70-gene
signature thereby broaden its application, we assessed the prognostic value of the 70-gene
signature in several clinically relevant breast cancer subgroups. In Chapter 4 we report on
the prognostic value and clinical utility of the signature in 148 postmenopausal patients
who were aged between 55 and 70 years and diagnosed with lymph node negative breast
cancer. Patients classified as good prognosis by the signature had a 5-year breast cancer-
specific survival (BCSS) of 99% (Standard error (SE) 1%), compared with 80% (SE 3%) inpatients with a poor prognosis signature respectively ( p = 0.036). Furthermore, the 70-
gene prognosis-signature was a significant and independent predictor of BCSS, especially
during the first 5 years of follow-up with an adjusted HR of 14.4 (95% CI 1.7-122.2; p = 0.01).
The benefit of chemotherapy in postmenopausal patients seems to be most pronounced
in the first 5 years after diagnosis, therefore results of this study indicated a more accurate
allocation of AST using the signature. In Chapter 5 we describe the validation of the 70-gene
signature in an independent retrospective series of breast cancer patients with 1-3 positive
lymph nodes. The aim of this study was to identify patients with 1-3 positive nodes who are
likely to remain free of distant metastases. Among the 241 patients, 99 (41%) were classified

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 202/248
Summary
219
11
as good prognosis by the 70-gene signature, whereas 142 (59%) patients were classified as
poor prognosis. The 10-year distant metastasis-free (DMFS) and BCSS probabilities were
91% (SE 4%) and 96% (SE 2%) for patients with a low risk 70-gene signature, respectively
and 76% (SE 4%) and 76% (SE 4%), respectively for patients with a high risk signature. The
signature was associated with disease outcome independent of traditional prognostic
factors, with an adjusted HR of 7.17 (95% CI 1.81-28.43; p = 0.005). In contrast to the 70-
gene signature, Adjuvant! Classified only 32 patients (13%) as clinical low risk and 209
patients (87%) as clinical high risk, resulting in discordant risk assessments in 32% (72
patients). Remarkably, among the patients who were classified as high risk by Adjuvant! the
signature could identify 72 patients (34%) who had a low risk signature and indeed a good
disease outcome (10-year BCSS of 94% (SE 3%)). Furthermore, the signature was associated
with disease outcome in patients who did not receive adjuvant chemotherapy. The results
of this study showed that the 70-gene signature could identify patients with an excellent
disease outcome, even among patients with lymph node positive disease who might be
safely spared chemotherapy. Based on these results the MINDACT trial has extended its
eligibility criteria to include patients with up to 3 positive nodes.
The aim of the study described in chapter 6 was to evaluate the accuracy of the 70-
gene signature in patients with tumors less than 2.1 cm (pT1). With the introduction
of mammographic screening the proportion of small breast tumors has increased
tremendously. In a pooled database of 964 patients the signature accurately distinguished
patients with a good outcome from those with a poor outcome; this prognostic value was
independent of clinicopathological characteristics with an adjusted HR of 3.25 (95% CI 1.92-5.51; p < 0.001) for BCSS at 10 years. The results of this study emphasize that a considerable
proportion of small tumors metastasize, supporting the idea that metastatic capacity is
an early inheritance that can be identified by the 70-gene signature (28% distant relapse
rate at 10 years in tumors classified as poor prognosis by the signature). Therefore, the 70-
gene signature can be useful to optimize and individualize treatment decision-making in
patients with pT1 tumors.
In Chapter 7 we analyzed 541 patients from a retrospective pooled database who had
received adjuvant systemic therapy and who were classified by the 70-gene signature.
Among the 541 patients who received either endocrine therapy alone (n=315) or incombination with chemotherapy (n=226) the 70-gene signature classified 252 patients as
low risk and 289 patients as high risk. Patients with a high risk 70-gene signature treated
with chemotherapy followed by endocrine therapy had a significantly better 5-year distant
disease-free survival (DDFS) compared with high risk patients who were treated with
endocrine therapy alone (88% versus 76%, respectively; p < 0.01). Conversely, patients with
a low risk 70-gene signature who were treated with chemotherapy followed by endocrine
therapy had similar disease outcomes as low risk patients treated with endocrine therapy
alone (5-year DDFS 99% versus 93%, respectively; p = 0.62). This suggests that patients
classified as high risk by the signature do benefit from adjuvant chemotherapy in addition

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 203/248
Chapter 11
220
to endocrine therapy. Moreover, the benefit of chemotherapy appears to be absent in
patients with a low risk signature, which will further justify withholding chemotherapy in
these patients.
In Chapter 8 we describe a validation study of the computer tool Adjuvant! in 5,380 Dutch
breast cancer patients. Adjuvant! is a web-based tool that predicts disease outcome and
treatment benefit for the individual patient, based on clinicopathological characteristics
such as age, co-morbidity, tumor size, tumor grade, lymph node status and estrogen receptor
status. The program has been developed and validated on American and Canadian breast
cancer patients. The aim of this study was first to assess the accuracy of predicted outcome
by Adjuvant! in (subgroups of) Dutch breast cancer patients. In addition, we investigated
its ability to discern patients having good outcomes from those having poor outcomes
(discriminatory accuracy). Results showed that the model could accurately predict outcome
on group level (differences between predicted and observed outcomes were within 2%
for most clinically relevant subgroups) and could be applied to most patients, with the
exception of patients younger than 40 years. Adjuvant! overestimated outcome in these
patients by approximately 4.5% and predictions of Adjuvant! in patients less than 40 years
should be treated with caution, especially in patients with an estrogen receptor positive
tumor. The discriminatory accuracy of Adjuvant! was only moderate, suggesting that the
model’s predictions could be improved by adding additional prognostic information, such
as provided by the 70-gene signature.
As we have shown in the previous chapter, models such as Adjuvant! can predict disease
outcome but are still suboptimal. Therefore, we investigated whether method of detection
has additional prognostic value that could improve the estimation of prognosis. This question
is addressed in chapter 9, where we studied the accuracy of prediction by Adjuvant! in
patients with a screen-detected carcinoma as well as assessed the independent prognostic
value of screen-detection in a retrospective patient cohort of 2,592 breast cancer patients
aged 50-69 years, with invasive breast cancer. Method of detection was classified as (1)
screen-detected carcinomas, defined as carcinomas that were mammographically detected
in the first or subsequent screening rounds (n = 958); (2) interval carcinomas, defined assymptomatic carcinomas that were diagnosed within 24 months of a negative screening
(n = 417); and (3) nonscreening-related carcinomas, defined as symptomatic carcinomas
in patients who were not participating in the screening program (n = 1,217). Adjuvant!
predicted the outcome among patients with nonscreening-related carcinomas accurately
(predicted survival was within 2% of the observed survival and/or not significantly different
in all but one group), whereas Adjuvant! predictions underestimated overall survival
and breast cancer-specific survival among patients with screen-detected and interval
carcinomas. Prediction of breast cancer-specific survival was underestimated by Adjuvant!
for patients with screen-detected carcinomas by -3.2%. Screen-detected carcinomas were

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 204/248
Summary
221
11
associated with a significant reduced mortality compared with nonscreening-related
carcinomas. The prognostic value of screen-detection was independent of the well-known
stage shift that is caused by screening (i.e. earlier stage at diagnosis), with an adjusted HR of
0.62 (95% CI 0.50-0.78; p < 0.001). In addition, the prognostic value of method of detection
was similar across tumor size and lymph node status categories, again indicating its
prognostic value beyond stage migration. As a consequence of these results, we propose
that method of detection should be used in combination with traditional markers of tumor
burden and aggressiveness to estimate prognosis for each patient, and to guide their
decision to receive adjuvant systemic therapy.
In chapter 10 the major results presented in this thesis are discussed and put in
perspective of current clinical practice. In general, the 70-gene signature could improve the
prediction of disease outcome in several subgroups. Most likely the combination of (new)
clinicopathological factors and gene expression signatures could even further improve
accurate estimation of prognosis.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 205/248
Chapter 12
Nederlandse samenvatting
List of publications
Dankwoord
Curriculum vitae

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 206/248
Chapter 12
224

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 207/248
Nederlandse samenvatting
225
12
Borstkanker is de meest voorkomende maligniteit bij vrouwen in de wereld. In 2008 werden
er in Nederland 13.005 vrouwen gediagnosticeerd met een invasief mammacarcinoom en
overleden er 3.327 patiënten aan de gevolgen van borstkanker. Hoewel de incidentie van
borstkanker stijgt, wordt er, ten gevolge van de invoering van screening op borstkanker
en het toegenomen gebruik van adjuvant systemische therapie (AST), een afname van
de mortaliteit gezien. De nieuwere adjuvante systemische therapieën zijn bovendien
effectiever en leiden tot een verdere reductie van de mortaliteit. Volgens de huidige
richtlijnen komt het merendeel van de borstkankerpatiënten in aanmerking voor een vorm
van AST. Hoewel de behandeling met AST de overleving in de borstkankerpopulatie in zijn
geheel verbetert, zullen er ook patiënten zijn die geen baat van deze behandeling hebben
omdat ze door alleen locoregionale behandeling genezen zijn. Voorts kan chemotherapie
ernstige acute en late bijwerkingen hebben, waardoor in een bepaalde groep patiënten
AST dan ook meer schadelijk dan nuttig zal zijn.
Aanvullende systemische therapie wordt geadviseerd op grond van prognostische en
predictieve kenmerken van het primaire tumorproces. Van oudsher wordt met behulp
van klinische en pathologische factoren een inschatting gemaakt van de prognose
van een patiënt. Patiënten met een ongunstige prognose, d.w.z. een hoog risico op
het ontwikkelen van afstandsmetastasen en/of het overlijden aan de gevolgen van
borstkanker, komen in aanmerking voor AST. Laagrisico patiënten zijn patiënten die met
alleen locoregionale behandeling een grote kans op genezing hebben en waarbij AST
naar verwachting geen of slechts een geringe verbetering van de overleving zal geven.De klinisch-pathologische kenmerken die gebruikt worden voor de voorspelling van de
prognose van de individuele patiënt blijken echter maar van beperkte waarde, vooral
omdat patiënten met morfologisch identieke tumoren een heel verschillend ziektebeloop
kunnen hebben. Het gebrek aan nauwkeurige identificatie van patiënten met een laag
risico op het ontwikkelen van afstandsmetastasen resulteert in overbehandeling, gepaard
gaande met onnodige toxiciteit, terwijl een onjuiste selectie van hoogrisico patiënten
onderbehandeling kan veroorzaken en daarmee de overlevingskansen van patiënten
kan verminderen. Behandeling op maat, de zogenaamde “patient-tailored treatment”, zal
over- en onderbehandeling terugdringen, maar kan alleen worden gerealiseerd indiener nieuwe en betere prognostische en predictieve markers worden geïdentificeerd.
Dit proefschrift richt zich op het nut van een nieuwe prognostische test (het 70-genen
profiel of MammaPrint™; hoofdstuk 2-7), een reeds veelgebruikt prognostisch model
(Adjuvant!; hoofdstuk 8) en een potentieel nieuwe prognostische factor (methode van
detectie; hoofdstuk 9). Bovendien hebben we de toepasbaarheid van deze prognostische
markers in verschillende subgroepen geëvalueerd.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 208/248
Chapter 12
226
Hoofdstuk 1 geeft naast een algemene inleiding over de behandeling van borstkanker en
het gebruik van traditionele prognostische markers en genexpressieprofielen, een beknopt
overzicht van het onderzoek beschreven in dit proefschrift en de klinische vraagstellingen
die er aan ten grondslag liggen.
Het eerste deel van dit proefschrift richt zich op de toepasbaarheid en de klinische waarde
van het 70-genen profiel. In hoofdstuk 2 geven we een overzicht van de ontwikkeling
en eerste validatie van het 70-genen profiel. Dit profiel is ontwikkeld met behulp van een
retrospectieve serie van 78 patiënten, jonger dan 55 jaar en gediagnosticeerd met een
invasief mammacarcinoom kleiner dan 5.1 cm (pT1-2) zonder axillaire lymfekliermetastasen.
Vierenveertig van de 78 patiënten hadden een ziektevrije overleving van minimaal 5 jaar
(goede prognose), terwijl 34 patiënten binnen 5 jaar na diagnose afstandsmetastasen
ontwikkelden (slechte prognose). Met behulp van gesuperviseerde analyses werden 70
genen geselecteerd die verschillend tot expressie kwamen in de 2 prognostische groepen en
die het sterkst correleerden met het ontwikkelen van afstandsmetastasen. Het profiel werd
vervolgens gevalideerd in een consecutieve serie van 151 patiënten met lymfekliernegatief
en 144 patiënten met lymfeklierpositief mammacarcinoom. Deze validatiestudie
toonde aan dat het profiel in staat was om patiënten met een goede prognose (n=115)
nauwkeurig te kunnen onderscheiden van patiënten met een slechte prognose (n=180).
Bovendien was de voorspellende waarde van het profiel onafhankelijk van traditionele
klinisch-pathologische criteria (gecorrigeerde hazard ratio (HR) voor afstandsmetastasen
als eerste event was 4.6; 95% confidence interval (CI) 2.3–9.2; p < 0.001). In een volgendeinternationale en onafhankelijke validatiestudie werd in 302 lymfekliernegatieve patiënten
uit 5 Europese ziekenhuizen de prognostische waarde van het profiel bevestigd. Deze
patiënten waren geen van allen adjuvant systemische behandeld. Naast de validatiestudies
worden in hoofdstuk 2 ook twee studies naar de uitvoerbaarheid van het 70-genen profiel
in de dagelijkse praktijk beschreven. De eerste studie, de zogenaamde RASTER (MicroarRAy
PrognoSTics in kanker van de borst) demonstreerde de haalbaarheid van het gebruik
van het profiel voor de besluitvorming betreffende AST in 16 algemene ziekenhuizen in
Nederland. In een Europese pilot studie, welke ook in detail beschreven staat in hoofdstuk
3, werd de logistiek voor de prospectieve gerandomiseerde MINDACT (Microarray InNode-negative and 1-3 positive lymph node disease may Avoid ChemoTherapy) studie
getest en geoptimaliseerd. Deze studie toonde aan dat het goed mogelijk is om vers
gevroren tumorweefsel van voldoende kwaliteit voor microarray analyse te verzamelen
in verschillende Europese ziekenhuizen en daarvandaan te verzenden naar een centrale
microarray faciliteit. Indien de patholoog een tumorsample kon verkrijgen was het in 77%
(46/60) van de gevallen mogelijk om een 70-genen profiel te bepalen. In 18% (11/60) was
het tumorsample niet representatief voor de tumor (< 50% tumorcellen) en kon er geen
70-genen profiel worden bepaald. Op basis van deze resultaten en de opgedane ervaring
in deze pilot studie werden zogeheten “standard operating procedures” ontwikkeld, welke

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 209/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 210/248
Chapter 12
228
voor patiënten met een hoogrisico profiel. De prognostische waarde van het profiel was
opnieuw onafhankelijk van traditionele prognostische factoren, met een gecorrigeerde
HR van 7.17 (95% CI 1.81-28.43; p = 0.005). In tegenstelling tot het 70-genen profiel
classificeerde het Adjuvant! model (op basis van traditionele klinisch-pathologische
kenmerken) slechts 32 patiënten (13%) als laag risico en 209 patiënten (87%) als klinisch
hoog risico wat resulteerde in een discordante risico-inschatting in 32% van de patiënten
(72 patiënten). Opmerkelijk is dat binnen de patiënten die werden geclassificeerd als hoog
risico door Adjuvant! het profiel nog 72 patiënten (34%) kan identificeren die een laagrisico
profiel en inderdaad een goede overleving hebben (10-jaars borstkankerspecifieke
overleving van 94% (SE 3%)). Het profiel bleek eveneens geassocieerd met overleving
van de patiënten die niet waren behandeld met adjuvante chemotherapie. De resultaten
van deze studie tonen aan dat het 70-genen profiel patiënten weet te identificeren die
ondanks 1-3 lymfekliermetastasen een uitstekende prognose hebben en waarbij adjuvante
chemotherapie wellicht overbodig is. Op basis van deze resultaten zijn de inclusiecriteria
voor de MINDACT studie uitgebreid tot patiënten met maximaal 3 positieve lymfeklieren.
Hoofdstuk 6 beschrijft de waarde van het 70-genen profiel voor patiënten met een
mammacarcinoom kleiner dan 2.1 cm. Door de introductie van het bevolkingsonderzoek
naar borstkanker, waar vrouwen van 50 jaar en ouder middels mammografie worden
gescreend, is het percentage kleine mammacarcinomen dat gediagnosticeerd wordt de
afgelopen jaren sterk toegenomen. Hoewel een kleine tumordiameter over het algemeen
beschouwd wordt als een indicator voor een goede prognose, blijkt het 70-genen profiel ook
in deze groep patiënten met een goede prognose nauwkeurig te kunnen onderscheidenvan patiënten met een slechte prognose. In 964 patiënten met een tumor kleiner dan 2.1
cm (pT1) had het profiel opnieuw prognostische waarde onafhankelijk van de klinisch-
pathologische kenmerken, met een gecorrigeerde HR van 3.25 (95% CI 1.92-5.51; p < 0.001)
voor 10-jaars borstkankerspecifieke overleving. De resultaten van deze studie benadrukken
dat een aanzienlijk deel van de kleine tumoren metastaseert, en ondersteunen daarmee
het idee dat het vermogen tot metastaseren al vroeg in de tumorontwikkeling wordt
bepaald. Met behulp van het 70-genen profiel kan dit vermogen tot metastaseren
nauwkeuriger worden bepaald (van patiënten geclassificeerd door het profiel als hoog
risico recidiveert 28% binnen 10 jaar) en kan de behandeling van borstkankerpatiëntenmet relatief kleine tumoren (pT1) worden geoptimaliseerd en geïndividualiseerd.
In Hoofdstuk 7 hebben we 541 adjuvant systemisch behandelde patiënten geanalyseerd
die zijn geselecteerd uit een retrospectieve gepoolde database. Van de patiënten
die behandeld waren met endocriene therapie alleen (n = 315) of in combinatie met
chemotherapie (n = 226) werden 252 patiënten geclassificeerd als laag risico en 289 patiënten
als hoog risico door het 70-genen profiel. Patiënten met een hoogrisico 70-genen profiel
die behandeld waren met endocriene therapie gevolgd door chemotherapie hadden een
significant betere 5-jaars afstandsmetastasen-vrije overleving vergeleken met hoogrisico
patiënten die behandeld werden met endocriene therapie alleen (respectievelijk 88% en

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 211/248
Nederlandse samenvatting
229
12
76%; p < 0.01). Omgekeerd hadden patiënten met een laagrisico profiel die behandeld
werden met endocriene therapie gevolgd door chemotherapie een vergelijkbare
uitkomst als laagrisico patiënten die behandeld werden met alleen endocriene therapie
(5-jaars afstandsmetastasen-vrije overleving van respectievelijk 99% en 93%; p = 0.62).
Dit suggereert dat patiënten geclassificeerd als hoog risico door het profiel baat zullen
hebben bij additionele chemotherapie, terwijl voor patiënten met een laagrisico profiel het
toevoegen van chemotherapie aan adjuvante endocriene therapie geen overlevingswinst
geeft. Deze resultaten ondersteunen de conclusies van bovengenoemde studies dat voor
patiënten met een laagrisico profiel het onthouden van chemotherapie gerechtvaardigd
is, enerzijds omdat de prognose van deze patiënten zeer goed is en anderzijds omdat de
winst van chemotherapie zeer beperkt lijkt te zijn.
In hoofdstuk 8 wordt de validatiestudie van het computerprogramma Adjuvant! in 5.380
Nederlandse borstkankerpatiënten gepresenteerd. Adjuvant! is een online beschikbaar
computerprogramma dat met behulp van klinisch-pathologische kenmerken de
prognose en de te verwachten winst van AST voor de individuele patiënt voorspeldt.
Voor het berekenen hiervan maakt het model gebruik van leeftijd en comorbiditeit
van de patiënt, tumor grootte en graad, aantal positieve lymfeklieren en de oestrogeen
receptorstatus. Het programma is ontwikkeld met behulp van gegevens van Amerikaanse
borstkankerpatiënten en werd reeds gevalideerd in een Canadese borstkankerpopulatie.
Het doel van deze studie was allereerst om te beoordelen of de voorspellingen van prognose
en behandelwinst door Adjuvant! ook toepasbaar zijn in (subgroepen van) Nederlandseborstkankerpatiënten. Bovendien is onderzocht of Adjuvant! in staat was om patiënten
met een goede prognose te onderscheiden van patiënten met een slechte prognose; deze
zogenaamde discriminatory accuracy zegt meer over de waarde van een marker of test
voor de individuele patiënt. De voorspelling van overleving op groepsniveau blijk zeer
nauwkeurig (verschil tussen voorspelde en geobserveerde overleving was < 2% voor de
meeste klinisch relevante subgroepen), met uitzondering van de voorspellingen voor
patiënten onder de 40 jaar. Adjuvant! overschat de overleving in deze groep patiënten met
ongeveer 4.5% waardoor enige voorzichtigheid is geboden bij het gebruik van Adjuvant!
in deze patiëntengroep, voornamelijk in geval van oestrogeen receptorpositieve tumor.De nauwkeurigheid van de voorspellingen op individueel niveau (discriminatory accuracy)
blijkt niet optimaal en kan worden verbeterd door het toevoegen van prognostische
informatie, zoals die van het 70-genen profiel.
Zoals hierboven beschreven zijn de voorspellingen van prognose door modellen als
Adjuvant! nog altijd suboptimaal. Het toevoegen van nieuwe prognostische factoren kan
deze predictie wellicht verbeteren. In Hoofdstuk 9 hebben we onderzocht of Adjuvant! de
prognose van patiënten met een screen-detected mammacarcinoom accuraat voorspelde
en of methode van detectie (d.w.z. carcinomen gedetecteerd in het kader van screening

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 212/248
Chapter 12
230
versus symptomatische carcinomen gediagnosticeerd buiten screening) zelf onafhankelijke
prognostische waarden had. Hiertoe zijn 2.592 patiënten in de leeftijd van 50-69 jaar,
met een invasief mammacarcinoom geselecteerd uit de database die is gebruikt voor
de validatie van Adjuvant! zoals beschreven in hoofdstuk 8. Methode van detectie is als
volgt gedefinieerd (1) screen-detected carcinomen, niet-symptomatische carcinomen
die werden gediagnosticeerd op basis van het mammogram gemaakt in het kader van
screening (n = 958); (2) interval carcinomen, gedefinieerd als symptomatische carcinomen
die werden gediagnosticeerd binnen 24 maanden na een negatieve screening (n = 417); en
(3) niet-screeninggerelateerde carcinomen, gedefinieerd als symptomatische carcinomen
gediagnosticeerd in vrouwen die niet aan de screening deelnamen (n = 1.217). Screen-
detected carcinomen werden geassocieerd met een aanzienlijk betere overleving in
vergelijking met niet-screeningsgerelateerde carcinomen. De prognostische waarde van
screen-detectie was onafhankelijk van de verschuiving naar een vroegtijdiger stadium
bij diagnose zoals die wordt gezien bij screening (stage shift), met een gecorrigeerde HR
van 0.62 (95% CI 0.50-0.78; p < 0.001). Bovendien was de voorspellende waarde van de
methode van detectie gelijk in patiëntgroepen onderverdeeld op basis van tumorgrootte
en lymfeklierstatus, wat nogmaals bevestigt dat de prognostische waarde van methode
van detectie niet afhankelijk is van de verschuiving naar een vroeger stadium bij diagnose.
Gezien bovenstaande lijkt het gebruik van methode van detectie als marker in combinatie
met traditionele prognostische factoren tot een betere voorspelling van prognose te
kunnen leiden, en zal het op die manier de keuze voor wel of geen AST betrouwbaarder
maken.
In hoofdstuk 10 worden de belangrijkste resultaten van dit proefschrift besproken
en gerelateerd aan de huidige klinische praktijk. In het algemeen zal het gebruik van
het 70-genen profiel de voorspelling van ziektebeloop verbeteren, niet alleen in de
patiëntengroep waarin het profiel is ontwikkeld, maar ook in andere subgroepen zoals
postmenopauzale patiënten. Waarschijnlijk zal het combineren van (nieuwe) klinisch-
pathologische factoren met genexpressieprofielen de voorspelling van prognose verder
kunnen verbeteren.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 213/248
Chapter 12
Nederlandse samenvatting
List of publications
Dankwoord
Curriculum vitae

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 214/248
Chapter 12
234
Mook S, Van ’t Veer LJ, Rutgers EJ, Ravdin PM, Van de Velde AO, Van Leeuwen FE, Visser O,
Schmidt MK. Independent prognostic value of screen detection in invasive breast cancer.
JNCI, accepted for publication.
Knauer M, Mook S, Rutgers EJ, Bender RA, Hauptmann M, Van de Vijver MJ, Koornstra RH,
Bueno-de-Mesquita JM, Linn SC, Van ‘t Veer LJ. The predictive value of the 70-gene signature
for adjuvant chemotherapy in early breast cancer. Breast Cancer Res Treat 2010; 120: 655-661.
Mook S, Knauer M, Bueno-de-Mesquita JM, Retel VP, Wesseling J, Linn SC, Van ‘t Veer LJ,
Rutgers EJ. Metastatic potential of T1 breast cancer can be predicted by the 70-gene
MammaPrint signature. Ann Surg Oncol 2010; 17: 1406-1413.
Mook S, Schmidt MK, Weigelt B, Kreike B, Eekhout I, Van de Vijver MJ, Glas AM, Floore A,
Rutgers EJ, Van ‘t Veer LJ. The 70-gene prognosis signature predicts early metastasis in
breast cancer patients between 55 and 70 years of age. Ann Oncol 2010; 21: 717-722.
Mook S, Schmidt MK, Rutgers EJ, van de Velde AO, Visser O, Rutgers SM, Armstrong N, Van
‘t Veer LJ, Ravdin PM. Calibration and discriminatory accuracy of prognosis calculation for
breast cancer with the online Adjuvant! program: a hospital-based retrospective cohort
study. Lancet Oncol 2009; 10: 1070-1076.
Bedard PL, Mook S, Piccart-Gebhart MJ, Rutgers ET, Van ‘t Veer LJ, Cardoso F. MammaPrint70-gene profile quantifies the likelihood of recurrence for early breast cancer. Expert Opinion on
Medical Diagnostics 2009; 3: 193-205.
Mook S, Bonnefoi H, Pruneri G, Larsimont D, Jaskiewicz J, Sabadell MD, MacGrogan G, Van
‘t Veer LJ, Cardoso F, Rutgers EJ. Daily clinical practice of fresh tumour tissue freezing and
gene expression profiling; logistics pilot study preceding the MINDACT trial. Eur J Cancer 2009;
45: 1201-1208.
Mook S, Schmidt MK, Viale G, Pruneri G, Eekhout I, Floore A, Glas AM, Bogaerts J, CardosoF, Piccart-Gebhart MJ, Rutgers ET, Van ‘t Veer LJ. The 70-gene prognosis-signature predicts
disease outcome in breast cancer patients with 1-3 positive lymph nodes in an independent
validation study. Breast Cancer Res Treat 2009; 116: 295-302.
Reyal F, van Vliet MH, Armstrong NJ, Horlings HM, de Visser KE, Kok M, Teschendorff AE,
Mook S, Van ‘t Veer L, Caldas C, Salmon RJ, van de Vijver MJ, Wessels LF. A comprehensive
analysis of prognostic signatures reveals the high predictive capacity of the proliferation,
immune response and RNA splicing modules in breast cancer. Breast Cancer Res 2008; 10: R93.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 215/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 216/248
Chapter 12
Nederlandse samenvatting
List of publications
Dankwoord
Curriculum vitae

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 217/248
Chapter 12
238

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 218/248
Dankwoord
239
12
Zo, dit is het dan. Het is bijna klaar. Rest mij alleen nog het schrijven van het meest gelezen
gedeelte van een proefschrift, het dankwoord. De afgelopen vijf jaar heb ik, steeds een
beetje meer, naar dit moment uitgekeken. Dankzij geweldige collega’s, vrienden en familie
is het uiteindelijk dan toch gelukt. Een aantal personen wil ik graag in het bijzonder
bedanken.
Allereerst gaat mijn dank uit naar mijn beide promotores.
Prof. dr. Laura J van ’t Veer, beste Laura, dat mijn lidmaatschap van U.S.R. Triton zou leiden
tot dit proefschrift en tot jouw eerste promovenda hadden we allebei nooit kunnen
bedenken. Dank voor je vertrouwen in mij. Ik bewonder jouw pioniersmentaliteit en heb
van je geleerd dat gewoon beginnen vaak het beste is. Dank ook voor je enthousiasme
en optimisme. Dat optimisme heeft iemand zoals ik, met een licht pessimistische inslag,
wel nodig af en toe. Zoals bij de TRANSBIG vergadering waar jij me, tijdens een verhitte
discussie, influisterde dat ik wel moest blijven lachen. Daarnaast wist jij altijd als geen ander,
op de momenten dat ik het allemaal even niet meer overzag, orde en rust te scheppen. De
traditie om mooie momenten (de dag dat alle samples voor de pilot studie uit Milaan in
een keer arriveerden, het tekenen van het MINDACT contract, de eerste MINDACT patiënt)
te vieren (met een flesje bubbels of geheel in stijl met een Turkse massage in Istanbul) vind
ik geweldig. Helaas ben je inmiddels vertrokken naar San Francisco, maar ik weet zeker dat
in de toekomst door een mooie samenwerking onze wegen weer zullen kruisen.
Prof. dr. Emiel J Th Rutgers, beste Emiel, bij onze eerste ontmoeting stond jij verstopt achtereen deur en maakte je een goede grap. Jij kunt je dat waarschijnlijk niet meer herinneren,
maar het heeft zeker een rol gespeeld in mijn komst naar het NKI. De afspraken met jou
waren constructief, stimulerend en gezellig. Ik denk dat we minstens de helft van de tijd
praatten over andere dingen in het leven. De paar momenten waarop ik echt vond dat
de dingen anders moesten en dat wilde bespreken, was jij me net voor en had je al over
een oplossing nagedacht. Een unieke en kostbare gave, zeker naarmate er meer vrouwen
in het vak komen! Dank voor de mogelijkheden die je me hebt gegeven. Dank ook voor
de waardevolle input en kritische klinische blik op mijn werk, maar zeker ook voor alle
gezelligheid!
Mijn dank gaat ook uit naar de leden van de promotiecommissie, Prof. dr. R. Bernards, Prof.
dr. J.W. Coeberg, Prof. dr. C.C.E. Koning, Prof. dr. J.W.R. Nortier, Prof. dr. S. Rodenhuis, Prof. dr.
M.J. van de Vijver en Dr. J.H.G. Klinkenbijl, voor het beoordelen van mijn manuscript.
Lieve Marjanka, dat jij mijn paranimf moest worden stond vast. Onze samenwerking begon
in Aspen, bij de AACR cursus. Onze vriendschap begon ook daar, bij de ontmoeting met
een bruine beer, geweldig! Ik heb veel van je geleerd op het gebied van epidemiologie
en statistiek, maar ook van jouw rust en kwaliteit om altijd dicht bij jezelf te blijven. Jouw

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 219/248
Chapter 12
240
kritische blik als ik er eigenlijk helemaal klaar mee was, en andersom, hebben tot 2 mooie
publicaties geleid. Door de drukte spreken we elkaar veel te weinig. Onze volgende
afspraak moet er een in een restaurant of op de rug van een paard zijn!
Lieve Inge, zonder jou had dit proefschrift zeker langer op zich later wachten. Jouw komst
bij de MINDACT was geweldig. Samen langs de Nederlandse ziekenhuizen, nieuwsbrieven
schrijven en de logistieke obstakels oplossen, we waren een goed team! Het was heerlijk
om de MINDACT werkzaamheden op een gegeven moment aan jou over te dragen en
me meer op mijn promotie te kunnen richten. Ik heb goede herinneringen aan onze
congresbezoeken. Zo weinig voorbereid als ik onderweg ging, zo goed voorbereid was jij.
In elke stad regelde jij een tafeltje in een leuk en trendy restaurant en zorgde je voor een
kamer in dat geweldige hotel. Lieve Ing, ik ken geloof ik weinig mensen die zo zorgzaam en
warm zijn als jij. Laten we snel weer eens een hapje gaan eten. Dan zoek ik een restaurant
uit…
Marleen, lieve Lena, allebei in Utrecht gestudeerd, maar pas in Amsterdam elkaar echt
gevonden. Wat hebben we een goede tijd gehad! Veel gepraat, gelachen, gehuild,
geklaagd en gedronken. Gegeten op de een of andere manier dan weer minder, we
kwamen vaak niet verder dan een portie bitterballen. Ik wil je bedanken voor de vele
discussies over het onderzoek: wat is nou de beste statische methode, wat is nou de
optimale patiëntenselectie. Met jouw gedrevenheid, enthousiasme en brede kennis ga
je ongetwijfeld een geweldige internist worden. Het enige minpuntje van jou als roomiewaren de met exotische zwammen begroeide koffiekopjes... Lieve Lena, ik mis je. Het wordt
tijd voor weer een blauwe-schoenen-borrel (zonder laptop), en dan beloof ik dat ik niet de
hele dag op jouw bank blijf hangen!
En dan natuurlijk Marieke, lieve dokteur Fulliburghhhh! Wat jammer dat je weg bent uit
het NKI. Miami Beach met jou was geweldig. De voorpret (en jouw angst dat ik een week
lang niets zou eten) ook. Behalve dat je een ster bent in relativeren en analyseren (en dat
dan ook nog razendsnel) ben je vooral ook een heel lief mens met een briljant gevoel voor
humor! Het komt allemaal goed!
Lieve Olga, hoe heerlijk is het om bij jou in je stoel neer te ploffen om gewoon even lekker
te kletsen! En hoe heerlijk ook dat jij, als ik bijna helemaal in de stress schoot, mij een
mailtje stuurde dat me deed schaterlachen of weer eens iets voor me regelde. Dank, je
bent een held!
Prof. dr. F.E. van Leeuwen en dr. M. Rookus, beste Floor en Matti, graag wil ik jullie bedanken
voor jullie kritische commentaar op manuscripten en presentaties. Otto Visser en Tony van
de Velde, wil ik bedanken voor het elke keer weer nauwkeurig aanleveren van data. Sterre,

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 220/248
Dankwoord
241
12
dank voor het eindeloos en nauwkeurig invoeren van data, wat heeft geleid tot een mooie
publicatie, één met twee Rutgers’s in de auteurslijst.
Dank aan iedereen op de afdeling pathologie, waar ik de eerste 2 jaar van mijn onderzoek
heb doorgebracht. Lieve Jolien en Valesca, roomies op de pathologie, dank voor alle steun
en gezelligheid. Jolien, wat hebben we een hoop meegemaakt! Laten we snel weer eens
echt bijkletsen!
Marieke, Leonie en Roelien, van jullie heb ik de kunst kunnen afkijken. Wat is het lang
geleden!
Ook wil ik graag alle H6ers en/of C2ers bedanken. Thea, dank voor je gezelligheid, ik kom
snel weer eens buurten. Annegien, Richard, Linde, Sjoerd B, Lorenza, Hans, Renske, Astrid
en de rest, dankzij jullie hoorde ik eindelijk eens echt ergens bij…
Huug, roomie van het laatste uur, wat goed dat ook jouw proefschrift binnenkort klaar is!
Dear Michael, thank you for the collaboration!
Sjoerd E, beste Sjoerd, straks heb ik eindelijk tijd om aan ons project te werken. Ik kijk er
naar uit.
Veel artikelen in dit proefschrift zijn mede mogelijk gemaakt door Agendia. In het bijzonder
wil ik Annuska, Arno, Bas, Femke, Guido, Ilja, Iris en Lisette bedanken voor de plezierige
samenwerking.
It has been an honor to be part of TRANSBIG. Dear Fatima, thank you for all the great
conversations and for your valuable input. Thanks also for taking the time to discuss my
future plans in Bordeaux. Radiation Oncology is such a great profession.
It has been a great pleasure and honor to work with Peter Ravdin. Dear Peter, thank you for
sharing all the Adjuvant! data with us. Our meetings were always stimulating. I admire your
broad knowledge about epidemiology and the clinical aspects of breast cancer, but also
your great sense of humor! Even at 4 o’ clock in the morning!
Thanks to professor Giuseppe Viale and Giancarlo Pruneri we were able to collaborate with
the European Institute of Oncology in Milan. Dear Beppe and Giancarlo, thank you and
hopefully we will meet somewhere soon at an international conference!
Dear Mahasti, working with you has always been a pleasure. We were not the most efficient
team, but definitely the team who had the best laughs.
I would also like to thank the EORTC, especially Jillian Harrison, Frederic Henot and Gaston
Demonty for the great collaboration. Hope to see you soon at an EORTC meeting!

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 221/248
Chapter 12
242
Medewerkers van de afdeling radiotherapie in het NKI-AVL, van stafleden tot laboranten,
van secretaresses tot doktersassistenten, het is een voorrecht mijn opleiding te mogen
volgen op een afdeling waar de sfeer zo goed is!
En dan natuurlijk de assistent van de radiotherapie. Lieve collega’s, dank voor alle
gezelligheid. Ik kan me geen betere collega’s wensen. Brian, dank voor het beantwoorden
van al mijn computervragen. Gerben, dank voor het beantwoorden van ongeveer alle
andere vragen (wanneer moet nou precies het manuscript naar de drukker??). Brenda, jouw
liefde voor de ani heeft heel wat gezellige en productieve avondjes op het NKI opgeleverd.
Laten we snel weer borrelen!
Lieve Utrechtse meiden, wat heb ik vaak verstek laten gaan… Het is altijd weer gezellig om
elkaar te zien. Ik ga er meer tijd voor vrij maken, dat beloof ik.
Lieve Anne & Sander, jullie zijn een goed stel, en niet in de laatste plaats omdat het ontstaan
is bij een kampvuurtje in Frankrijk, zonder jullie aanwezigheid... Ik hoop dat jullie snel weer
naar Haarlem komen, zodat we weer wat makkelijker een (of een paar) drankje(s) kunnen
drinken. Geniet van de kleine.
Lieve Baselga-gangers, dank voor de prachtweek, in het heetst van de strijd, toen ik het zo
nodig had!
Lieve Jantien, geweldig dat jouw werk op de cover van mijn proefschrift staat. Minstens zo
leuk is het om je weer te spreken! Je hebt een etentje van me te goed!
Lieve Jaap en Rina, met het afronden van mijn proefschrift komt er hopelijk weer meer tijd
om te fietsen. Hoewel het best frustrerend is om eraf gefietst te worden door 2 mannen
‘op leeftijd’ heb ik het er graag voor over. Zeker ook omdat het naborrelen bij jullie altijd zo
gezellig is!
Lieve Juul, dank voor je interesse en betrokkenheid. En voor al je lieve kaartjes op bijzonderemomenten!
Lieve Saakje, ook jij bedankt voor je interesse in mij en in mijn werk. We komen snel weer
eens jouw kant op! En wat heb je toch een leuke zoon!
Lieve El(les), super dat je mijn paranimf bent! Wat is er een hoop gebeurt de laatste jaren,
ongelooflijk. Ik heb enorme bewondering voor hoe je je staande houdt. Je bent een
supervriendin (en dat al zoo lang) en mooi mens!

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 222/248
Dankwoord
243
12
Lieve Myra, schoonzussie en pechvogel. Ik hoop dat de komende jaren meer geluk met zich
mee brengen! Dank voor je gastvrijheid, ik vind het heerlijk om bij jullie te zijn. Dank ook
voor het vertrouwen in Marcel en mij als oom en tante!
Lieve, lieve Merle & Luke, wat een rijkdom dat jullie er zijn. Als niets me meer vrolijk maakt,
laten jullie de zon weer schijnen! Komen jullie snel weer eens logeren?
Lieve Matijs, grote broer, wat ben ik blij met je. Hoewel we elkaar niet heel veel zien is het
altijd goed. Groter wederzijds respect en waardering is denk ik niet mogelijk.
Pap & mam, dank voor het grenzeloze vertrouwen en de onvoorwaardelijke liefde.
Lieve mam, geweldig om weer een week met je te schaatsen in Baselga, wat hebben we
gelachen (het was tenslotte allemaal voor de l..). Geweldig ook dat we zo veel kunnen
delen.
Lieve Pap, onze schaatszondag is heilig, vooral omdat het zo leuk is om iets samen met jou
te doen. Dank dat ik nooit iets hoef uit te leggen en dat je me af en toe komt redden! Die
deuk in mijn waguh is me dierbaar!
Ik hou van jullie.
Lieve, lieve Marcel (ik durf geen Marce meer te schrijven), mijn grote liefde. Dat ik jou 15 jaar
geleden toch ben tegen gekomen! Jouw optimisme, nuchterheid, humor en liefde maken
het leven tot een feestje. Dank voor alle steun en hulp, zonder jou was dit proefschrift erecht niet gekomen. Dank ook dat je bent wie je bent! Ik hoop dat de komende tijd je heel
veel goeds gaat brengen. Vanaf nu gaan we weer leuke dingen doen in het weekend! Ik
hou zielsveel van je.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 223/248
Chapter 12
Nederlandse samenvatting
List of publications
Dankwoord
Curriculum vitae

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 224/248
Chapter 12
246

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 225/248
Curriculum vitae
247
12
Stella Mook is geboren op 21 februari 1977 te Hoorn. Na het behalen van haar VWO
diploma aan de Openbare Scholengemeenschap te Hoorn begon zij in 1996 met de studie
geneeskunde aan de Universiteit van Utrecht. Tijdens haar studie deed zij gedurende 1 jaar
onderzoek naar het metabolisme van vrije vetzuren op de afdeling vasculaire geneeskunde
van het Universitair Medisch Centrum Utrecht, onder supervisie van dr. Manuel Castro
Cabezas. Na het behalen van het artsenexamen in 2003 werkte zij tot eind 2004 als
assistent-niet-in-opleiding op de afdeling interne geneeskunde van het Diakonessenhuis
te Zeist/Utrecht.
In mei 2005 begon de auteur als research fellow bij het Nederlands Kanker Instituut-Antoni
van Leeuwenhoek Ziekenhuis met de coördinatie van een Europese pilot studie. Deze
aanstelling werd een jaar later omgezet in een promotietraject, onder supervisie van prof.
dr. Laura J van ’t Veer en prof. dr. Emiel J.Th. Rutgers. Een gedeelte van dit onderzoek deed
zij in het kader van haar TRANSBIG fellowship.
In 2009 is zij begonnen aan de opleiding tot radiotherapeut in het Nederlands Kanker
Instituut-Antoni van Leeuwenhoek Ziekenhuis te Amsterdam, onder supervisie van
opleider dr. R.L.M. Haas en plaatsvervangend opleider en afdelingshoofd prof. dr. M. Verheij.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 226/248
Appendix
Gene signature evaluation as a prognostic
tool: challenges in the design of
the MINDACT trial
Jan Bogaerts
Fatima Cardoso
Marc Buyse
Sofia Braga
Sherene Loi
Jillian A Harrison
Jacques Bines
Stella Mook Nuria Decker
Peter Ravdin
Patrick Therasse
Emiel Rutgers
Laura J Van ’t Veer
Martine Piccart
on behalf of the TRANSBIG consortium
Nat Clin Pract Oncol 2006; 3: 540-551.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 227/248
Chapter 12
250
Summary
This Review describes the work conducted by the TRANSBIG consortium in the development
of the MINDACT (Microarray In Node negative Disease may Avoid ChemoTherapy) trial. The
goal of the trial is to provide definitive evidence regarding the clinical relevance of the 70-
gene prognosis signature, and to assess the performance of this signature compared with
that of traditional prognostic indicators for assigning adjuvant chemotherapy to patients
with node-negative breast cancer. We outline the background work and the key questions
in node-negative early-stage breast cancer, and then focus on the MINDACT trial design
and statistical considerations. The challenges inherent in this trial in terms of logistics,
implementation and interpretation of the results are also discussed. We hope that this
article will trigger further discussion about the difficulties of setting up and analyzing trials
aimed at establishing the worth of new methods for better selection of patients for cancer
treatment.
Review criteria
A formal literature search for this review was not performed; this review includes a summary
of the authors’ own work and knowledge, which covers various fields relating to oncology
and molecular biology.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 228/248
Appendix. Design of the MINDACT trial
251
12
Introduction
In the past 20 years, little progress has been made in identifying new prognostic markers
that can assist oncologists in treatment decision-making relating to node-negative
early-stage breast cancer. As a result, considerable differences exist worldwide in the
selection of women who require adjuvant chemotherapy based on their risk of breast
cancer recurrence. The breast cancer TNM (tumor–node–metastases) staging system is
based on anatomical extent (e.g. the size and lymph-node status) of the tumor, but this
classification gives little insight into breast cancer biology. Clinicians have long recognized
the heterogeneity of human breast cancers, not only in terms of their diverse natural
histories despite identical morphological features, but also in their variation in response
to treatment.1 These differences are also evident in the small ( i.e. <2 cm), node-negative
tumors that would generally be associated with a good clinical outcome. Attempts have
been made to identify good and poor prognosis groups based on pathological features
such as tumor grade, lymphatic invasion and S-phase fraction,2 which might better reflect
tumor biology. In recent years, numerous molecular prognostic and predictive markers
in oncology have been reported (Box 1). These tumor markers have had little impact in
routine clinical practice. Studies are often based on small, heterogeneous retrospective
series that have not been reported in a rigorous enough fashion to provide sufficient
information, particularly with regard to their methodology.3 Many follow-up studies have
shown inconsistent data compared with original results, which has been attributed to a
lack of statistical power, different patient populations, and technical limitations associatedwith such studies. There is also a paucity of well-designed, prospective assessments of the
clinical value of these tumor markers. As a result, the value of many promising prognostic
markers is still uncertain. We have yet to fully translate our increased understanding of
breast cancer biology into improved outcome for those with this heterogeneous disease.
The prognostic factors accepted by the NIH 2000 Consensus Development Conference
on Adjuvant Therapy for Breast Cancer did not include any molecular markers relevant
to breast cancer biology apart from the hormone receptors.4 The most recent St Gallen
consensus panel (2005)5 established three risk categories: minimal, intermediate and high.
Hormone receptors, tumor size, tumor grade and age remain key discriminating factors,and HER2 status, lymphatic or vascular invasion, or both in the primary tumor are new
accepted prognostic factors. In the UK, the Nottingham Prognostic Index is commonly used
to predict clinical outcome; this index is based on tumor size, tumor grade and lymph-node
status, and has a key role in discriminating node-negative patients for whom chemotherapy
should or should not be considered.6 All these consensus recommendations, however,
have important limitations and, in this era of evidence-based medicine, it is not possible to
reliably identify a group of women with excellent long-term clinical outcome.
By using gene-expression profiling, the Netherlands Cancer Institute developed a 70-
gene prognostic signature for node-negative breast cancer.7 The signature was developed

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 229/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 230/248
Appendix. Design of the MINDACT trial
253
12
criteria and the Adjuvant! software,11 which can calculate a 10-year survival probability
based on the patient’s age, tumor size, grade and ER status. 12 A recent evaluation of the
Adjuvant! software found that known clinical prognostic factors were able to predict overall
survival (OS), breast-cancer-specific survival, and event-free survival quite accurately in
4,083 patients diagnosed with breast cancer in British Columbia from 1989 to 1993, with
the exception of very young patients diagnosed under the age of 35.13 This independent
validation of the software reinforced its credibility as an accurate clinical tool to evaluate
breast cancer prognosis, making the ability of the 70-gene signature to outperform this
tool all the more notable.
The 70-gene signature remained a significant prognostic indicator of time to distant
metastasis and OS even after adjustment for all clinicopathologic factors known to have
prognostic value in this disease. The consortium decided that the low clinical risk group
would consist of patients with a 10-year breast cancer survival probability of at least 88% if
their tumors were 1% or greater positive for expression of ER using immunohistochemistry,
and of at least 92% if they were not. These two cutoffs were chosen to reflect the fact
that patients with ER-positive tumors now receive adjuvant endocrine therapy (with an
estimated absolute 10-year benefit of about 4% overall), whereas patients in the validation
series were all untreated regardless of their ER status. When adjusted for clinical risk based
on 10-year survival probability using the Adjuvant! software, the gene-signature adjusted
hazard ratios (Box 1) were 2.13 (95% CI 1.19–3.82) for time to distant metastasis, 2.66 (95% CI
1.46–4.84) for OS, and 1.36 (95% CI 0.91–2.03) for disease-free survival. Similar hazard ratios
were found in Cox multivariate regression analysis. These results indicate that the genesignature adds independent prognostic information to that provided by a risk assessment
based solely on clinicopathologic factors. Central pathology review of ER and tumor grade
and an independent source verification of all data by external auditors give these findings
significant strength. Furthermore, within each gene-signature risk group, the Kaplan–Meier
estimates of 10-year OS were almost identical to the two clinical risk groups as assessed by
the Adjuvant! software: patients classified as gene-signature low risk had 10-year survival
rates of 88% and 89%, respectively, for low and high clinical risk as defined by Adjuvant!,
while for patients classified as gene-signature high risk, the 10-year survival rate was 69%
for both clinical risk groups. The external and independent validation therefore confirmed the original findings that the
gene signature added significant independent prognostic information to that produced
by current clinicopathologic factors, and provided strong support for the initiation of the
MINDACT (Microarray In Node negative Disease may Avoid ChemoTherapy) trial.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 231/248
Chapter 12
254
The MINDACT study
The MINDACT trial is an international prospective, randomized study comparing the
70-gene signature classifier with commonly used clinicopathologic criteria for selecting
node-negative breast cancer patients for adjuvant chemotherapy. The trial is intended to
address whether a tool such as this can improve on existing methods of risk assessment
and treatment decision-making by assisting oncologists to select between node-negative
women who need adjuvant chemotherapy and those who do not. We will discuss
the challenges that arose in incorporating this question into a suitable design for the
prospective clinical trial. Studies similar in purpose to MINDACT might become more
frequent in the future as more prognostic and/or predictive signatures require validation
before their use in clinical practice.
The need for a randomized trial
Given the available retrospective validation data of the 70-gene prognostic signature, is
there any need to perform a large randomized trial? Although the available validation data
are compelling, we believe that before being accepted as standard practice, new biological
diagnostic tools must go through the same strict validation process as, for example, a new
drug or treatment approach. While phase II results may be promising, a new therapy might
only become a standard of care after being evaluated in at least one large prospective
randomized phase III trial. This is especially true with this technology given its high cost- €2,000 per patient - and the complexity and costs associated with the collection of
frozen tumor samples. The 21-gene recurrence score, developed by the National Surgical
Adjuvant Breast and Bowel Project and Genomic Health, and based solely on retrospective
validations, is marketed under the name Oncotype DX® (Genomic Health, Inc., Redwood
City, CA) and has not yet been approved by the FDA. The scientific community shares our
belief that a full prospective validation must be performed before this tool can be accepted
as standard of care, and such a validation is about to start via a large phase III prospective
trial - Tailor x - which is a joint effort between several American groups, funded by the
National Cancer Institute. The design of Tailor x is quite similar to that of the MINDACT trial,and collaborations and discussions are underway between the two consortia utilizing the
two trials. Only this type of large, prospective, biologically driven phase III trial can provide
the necessary level 1 evidence (Box 1) for any new biological marker or tool.
The huge research efforts in the development of microarray-based gene signatures are
often weakened by restricted numbers of patients. The supervised analysis of expression
data of thousands of genes for a limited number of patients has well-known pitfalls.14,15
For the external validation data set of the 70-gene signature, while the hazard ratios were
smaller than the previously published series, the result was still more powerful than any
other available covariate for this data set, providing evidence that the prognosis provided

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 232/248
Appendix. Design of the MINDACT trial
255
12
by the gene signature was robust and the technology reproducible. Nonetheless, as
retrospective patient series can also be biased by unknown factors leading to patient
selection, a prospective evaluation is vital. Furthermore, the use of the signature to guide
chemotherapy decision-making has not been tested by external validation, which dealt
only with the prognostic (as opposed to the predictive) value of the signature (Box 1).
It can also be argued that the patients selected for participation in a randomized trial will
be an investigator-selected subset of the population under consideration. This is indeed an
important point, and to evaluate selection bias during accrual an additional step has been
incorporated into the MINDACT trial design. Following enrollment of 800 patients (termed
the ‘pilot’ stage; see below), the data will be examined not only for logistical problems, but
also for potential bias of investigators and compliance with the randomization.
Some questions have arisen over whether it is too early to initiate this trial, given the
current rapid evolution of the technology, the previous methodological criticisms, and
the real possibility that the technology may be outdated at the completion of the trial.
Undoubtedly, there are and will be many predictive and prognostic signatures derived
from high-throughput technology reported in the future. It is clear that gene signatures
must be independently and externally validated before they proceed to prospective clinical
assessment and widespread use. Furthermore, like all diagnostic approaches, the ultimate
diagnostic gene signature may need refining as our knowledge advances. In our opinion,
prospective studies are the only way to provide level 1 evidence (Box 1) about the clinical
relevance of genomic signatures, and therefore the only way to endorse their widespread
clinical use, thereby allowing patients to benefit from these advances. Participation in thistrial should be strongly encouraged so that this issue can be addressed as soon as possible.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 233/248
Chapter 12
256
Box 1. Common statistical terms relevant to theMINDACT trial.
Prognostic
Defines patient outcome based on overall survivalor relapse-free survival in a group of patients
independent of exposure to therapy
PredictivePredictive factors should define sensitivity of a
tumor to a distinct therapeutic agent
Hazard ratiosIn survival analysis, the hazard ratio is an indication
of the difference between two survival curves,
representing the reduction in the risk of death withtreatment compared with control, over the period
of follow-up; the hazard ratio is a form of relative
risk
Level 1 evidence
Evidence arising from a randomized controlledclinical trial
Specificity The percentage of patients with a negative testresult who were not diagnosed with malignancy
Sensitivity
The number of patients with a true positive testresult (positive test result and tumor) divided by
the
total number of patients diagnosed withmalignancy
Key Points
In the past 20 years, little progress has beenmade regarding new prognostic markers that
can assist oncologists in treatment decision-making for node-negative early-stage breast
cancer

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 234/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 235/248
Chapter 12
258
axillary clearance. No patients treated with previous chemotherapy or radiotherapy will be
enrolled.
Determining the control arm
The trial objective is to prove that the 70-gene signature will safely assign fewer node-
negative patients to chemotherapy, and is directly related to the control criteria. For these
control criteria, two conditions are essential: the criteria should reflect current practice,
and they should be applied as homogeneously as possible in the trial. Satisfying both
conditions at the same time is a real challenge. Currently, oncologists decide whether
to prescribe chemotherapy according to several methods and guidelines, and it is
reasonable to assume that many modified versions of these criteria are being applied
in practice. Thus, there is no straightforward way of deciding on one set of rules as the
standard chemotherapy assignment method. One practical approach could be to allow the
participating investigational sites to apply their own predefined set of rules to represent
the current standard. Such an approach, however, would lead to considerable variability,
and the rate of chemotherapy assignment of such ‘standard’ criteria would depend on
the accrual at each participating site, rather than on the characteristics of the population
studied.
As the Adjuvant! software uses information from the San Antonio database, the SEER
(Surveillance, Epidemiology and End Results) database, the Overviews of clinical trials,
individual clinical trial results, and the literature in general, it is considered appropriatefor analysis of available patient prognosis data. It should be noted that the whole risk
assignment method is largely prognosis-based, in contrast to other attempts to base
the method on predictions of chemotherapy effect. Calculation of prediction has only
been applied to some level for ER status, where the method acknowledges the effect of
endocrine therapy in ER-positive patients, and the possibly greater effect of chemotherapy
in ER-negative patients, leading to a sizable benefit even for good-prognosis ER-negative
patients.
Also of note is the fact that the current version of the Adjuvant! software does not include
HER2 status, a marker that many believe has considerable data supporting its prognosticvalue.20 In addition, preliminary data indicate that HER2 status may have important
predictive implications particularly related to endocrine therapy.21 To tackle this issue, a
new version of the Adjuvant! software is being developed that will incorporate HER2
status. An additional consideration for HER2-positive patients is the need to administer
adjuvant trastuzumab, which, with its very important efficacy results, could interfere with
the detection of any difference between the chemotherapy and the endocrine therapy
arms of the trial. How this effect will influence treatment decisions will be evaluated in the
pilot phase of the first 800 patients.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 236/248
Appendix. Design of the MINDACT trial
259
12
Design of the trial
The initial concept of the trial design was straightforward. Each enrolled node-negative
patient would be randomized to chemotherapy treatment decision according to either
clinicopathologic criteria (control) or gene signature (experimental). The trial would then
aim to prove that a lower rate of chemotherapy administration in the experimental arm did
not result in inferior efficacy. With this approach, only half of the patients would need to
have their microarray analysis performed on a real-time basis.
There were two major and interrelated objections to this design. The first objection was
that, while this design tested the two approaches (experimental and control) against each
other in an overall fashion, it did not take into account the fact that for more than half
of the patients both approaches were in agreement. From a methodological perspective,
it is clear that any benefit of either approach would be greatly diluted in such overall
comparison, because a majority of patients could achieve the same result regardless of the
arm of randomization. Additionally, since it is impossible to ‘blind’ the investigators to the
clinicopathologic prognostic factors, in practice this design would actually compare the
combination of the methods with the clinicopathologic risk assessment alone because of
selection bias. This issue is related to the second limitation of this approach. Apart from the
discussion of defining an appropriate noninferiority threshold (delta), for the time being,
let us say we want to reject an inferiority null hypothesis (H 0) on the overall population
of H 0 = θE ÷ θC ≥ 1.25, where θE and θC represent the experimental and control hazards,
respectively, for some time to event endpoint (DMFS or OS). For any reasonably sized trial,it would be very hard to come up with a credible scenario wherein such a noninferiority
test would be likely to fail. In a noninferiority testing situation in which one can assume a
hazard ratio between two randomized arms, a one-sided 95% confidence noninferiority
test for the above null hypothesis would require about 512 events to perform the analysis
with 80% power. We performed simulations for such a trial and primary test, and showed
that in a situation in which the clinical criteria would perform very well (identifying
90% of patients who will metastasize), and the gene signature would select patients for
chemotherapy at random, the study would still yield powers of up to 50%. For less extreme,
but equally unacceptable situations, in which the gene signature should be identified asinferior, the power of ‘proving’ noninferiority would be even higher.
A trial using an overall (i.e. using all patients) noninferiority test would need to have an
inferiority threshold hazard ratio of at least 0.90, and probably at least 0.95, to convincingly
exclude performances of a gene signature that would still be considered to be very
poor. Thus, a noninferiority trial that would reliably exclude the poor performance of a
gene signature would need to be huge or of extremely long duration. Even under such
conditions, it is likely that a scenario of underperforming gene tests that would yield
reasonably nice hazard ratios in an overall comparison would arise. The addition of a large
fraction of observations that are the same irrespective of the arm they are randomized

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 237/248
Chapter 12
260
to makes any equivalence test procedure highly suspect. Such observations increase the
likelihood of ‘random noise’, which makes statistically significant rejection of inferiority
more likely. Such a situation, in general, is not acceptable for equivalence or noninferiority
testing.22 This design, therefore, was not selected, and other possibilities were considered.
Two other options that could be considered were the following: to assign chemotherapy
according to the 70-gene classifier risk model while assessing the clinical risk, or to assign
chemotherapy according to clinical criteria while assessing the 70-gene risk. The first
option is a much too big leap forward and the second would not test the 70-gene signature
appropriately.
As an outcome of the above considerations, attention and discussion started focusing on
discordant patients, and considered such patients as the core group. Using the original
approach, this group would have been identifiable only in patients randomized to use
the gene signature, as the signature would not have been performed for the other arm. It
became clear that one should perform the gene signature on all patients entered into the
trial, in order to identify all patients who would be treated differently by the two methods.
This group of patients would consist of two distinct subgroups: those who are at low
risk according to the gene signature and high risk according to clinicopathologic criteria
(stratum A), and those who are at high risk according to the gene signature and low risk
according to clinicopathologic criteria (stratum B; Figure 1). Having a lower chemotherapy
assignment rate with the gene signature is equivalent to saying that stratum A should be
larger than stratum B, because more patients would be at low risk according to the gene
signature.Since the main objective of the trial is to put the gene signature to the test, we concluded
that its design should randomize patients who have discordant risk assessments to one
of the two methods to be used for chemotherapy decision-making. In fact, such a course
is equivalent to randomizing such patients to receive chemotherapy or not. For the
other patients, who have either both risk assessments as high risk, or both as low risk, a
randomization for this type of risk assessment will not have a true value. These patients,
therefore, will not be randomized, but will be treated or not with chemotherapy according
to the concordant risk assessments, and followed further. All patients with hormone-
sensitive disease will also receive endocrine therapy.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 238/248
Appendix. Design of the MINDACT trial
261
12
Figure 1. Randomization of discordant cases in the MINDACT trial.
Abbreviation: CT, chemotherapy.
Sample size
At the time of the first discussions regarding the MINDACT trial design, the noninferiority
design was proposed and a sample size of 5,000 was envisaged, with microarray analysis
performed on half of these patients. As discussions evolved, it was decided that only the
discordant cases would be randomized to treatment decision-making using either thegenomic tool or the clinicopathologic criteria. In order to be able to formulate and answer
questions with regard to the core group of discordant cases, the sample size was increased
from 5,000 to 6,000 patients.
Testing
From the available data on the gene signature and Adjuvant! software, there is a strong
belief that the gene signature will produce a larger fraction of patients designated as low
risk than the clinicopathologic method described above. Assignment fractions accordingto both methods will be evident from the trial design, and both methods will be available
for all patients, so paired data are available for analyzing this endpoint. After the preceding
discussions, it would be fair to conduct a noninferiority test on the selected group of
patients with discordant risk data. Unfortunately, with an expected proportion of discordant
patients of 30–35%, the number of patients needed for the trial would become prohibiting,
particularly considering the high costs associated with the microarray technology and the
complex trial logistics.
Let us revisit the question of what the real objective of such a trial is. We can first clarify what
the objective is not. It is not a trial to find the fractions of high-risk and low-risk patients
Randomized:
decide with clinical tool
Randomized:
Decide with genomic tool
High clinical risk
(low genomic risk)
Low clinical risk
(high genomic risk)
High genomic risk
(low clinical risk)
Low genomic risk
(high clinical risk)
A1: CT
B1: no CT
B2: CT
A2 no CT
Discordant cases-randomized
Stratum A: genomic low, clinical high
Stratum B; genomic high, clinical low

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 239/248
Chapter 12
262
according to the gene signature, because these can be found with an observational trial.
In this context, an observational trial would involve treating the patients according to the
established clinicopathologic guidelines and the patients’ genomic risk, but not making a
decision based on the treatment outcome. Indeed, for this endpoint, the present trial will
function as a very large prospective observational trial. Also, it is not a trial to determine
the effect of chemotherapy in specific subgroups. Such an issue may be of interest, but it is
not the primary goal of the trial to address it. A priori assumption (before having the outcome
of the trial) may be that chemotherapy does have an effect (in terms of a hazard ratio)
for some of the patients that have a good gene signature, but that for these patients the
prognosis is so good that it is not acceptable to treat them all with a toxic treatment. This
is the same rationale whereby not all node-negative patients are given chemotherapy. In
mathematical terms, the hazard ratio may still be different from 1 (and may be more or less
constant for the whole population), but because of the small event rate in an identifiable
good-prognosis group, the absolute effect is outweighed by the acute and long-term
toxicity of chemotherapy.
If we consider a gene signature (or some other set of criteria) as a diagnostic test to detect
those patients who will have recurrent disease that can no longer be treated with curative
intent (i.e. metastasis), we can discuss its performance in terms of specificity and sensitivity
(Box 1). We cannot expect the gene signature to be perfect (i.e. to have 100% sensitivity and
specificity), but we can try to prove that it is good enough in the clinical situation—that is,
sufficient to prevent undertreatment of patients, which relates to the sensitivity of the gene
signature. To address this requirement, we incorporated the following primary test intothe trial design. In the set of patients who have a low-risk gene-signature prognosis and
high-risk clinicopathologic criteria, and who will be randomized to use the gene-signature
prognosis and thus receive no chemotherapy (group A2 in Figure 1), a null hypothesis of a
5-year DMFS of 92% will be tested. With 6,000 patients accrued overall, and based on the
available validation data estimates, this set has an expected size of 672 patients. With an
accrual of 3 years, and a total duration of 6 years ( i.e. 3–6 years’ follow-up for each patient),
a one-sided test at 97.5% confidence level has 80% power to reject this hypothesis if the
true 5-year DMFS is 95%.
The major criticism of this primary test is that it is not a test that compares the randomizedgroups. If the above test is statistically significant, however, and the gene signature does
select fewer patients to be treated with chemotherapy while not adversely affecting DMFS,
then this can be taken to be equivalent to proving that the signature has a very good
sensitivity, as well as a specificity that is better than the clinicopathologic method. In our
opinion, therefore, a significant primary test as described above would establish the role
of such a signature in chemotherapy treatment decision-making in node-negative breast
cancer patients.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 240/248
Appendix. Design of the MINDACT trial
263
12
The pilot phase
All patients must have an available and high-quality frozen tumor sample to be eligible
for the MINDACT trial. The desired number of patients might become impractical because
of logistics problems such as transport problems, insufficient material, insufficient quality
of RNA, and so on. This issue is currently being assessed in a Pilot Logistics Study, run in
seven centers in seven different European countries. Additionally, all these issues and all
the assumptions made will be assessed and corrected if necessary during the pilot phase
of MINDACT, composed of the first 800 patients.
This pilot phase should ensure that the complex logistical framework put in place for
this trial is feasible for the patients, physicians and laboratories involved. Assessment by
Agendia of the quality and quantity of RNA samples will be part of this first phase. The
second aim of the pilot phase is to ascertain that the patient population recruited upfront
for MINDACT is not a biased one. This will be done by checking whether the ratio of low-
risk to high-risk patients is as expected. Third, there is a concern that clinicians might not
comply with the randomization of the treatment decision, violating the protocol. A patient
who is clinically high-risk and has a low genomic risk, who is randomized by use of the
genomic tool, should not be given chemotherapy. By contrast, a patient who is clinically
low-risk and has a high genomic risk and is randomized to decision with the genomic tool
should be given chemotherapy. The compliance with this randomization is to be assessed
in the pilot phase. Following the treatment randomization, there will be two additional
randomizations: chemotherapy and endocrine therapy. The fourth objective of the pilotphase is to check whether at least 66% of those women assigned to chemotherapy are
subsequently randomized in the chemotherapy question. The final aim of the pilot study
is to ensure that there is a statistically significant difference between the percentage of
patients that have a high clinicopathologic risk and those with a high genomic risk, thus
reflecting the expected reduction in chemotherapy administration.
Further randomizations
Since the primary randomization is the most complex and innovative part of this trial, thebulk of this article has focused on this element, but it should be noted that the trial will
also have two further randomizations. Patients who are to receive chemotherapy may be
randomized to receive either an anthracycline-based regimen or a docetaxel–capecitabine
regimen.23,24 This randomization (designated R-C) will ask whether a docetaxel–
capecitabine regimen can safely replace an anthracycline-based regimen in high-risk
node-negative women, with the potential advantage of a reduction in the two long-term
toxicities associated with anthracyclines: cardiac toxicity and secondary leukemia. The
docetaxel–capecitabine combination is currently being evaluated in the adjuvant setting
in the US. As short-term toxicity is of some concern with this regimen, in MINDACT the

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 241/248
Chapter 12
264
first 40–120 patients randomized to this treatment will be closely monitored. Several
commonly used anthracycline-based regimens will be accepted within the trial that have
adequate anthracycline dose intensity, three or more drug combinations, and six cycles of
administration.
Patients eligible for endocrine therapy can participate in the endocrine therapy
randomization stage of the trial (designated R-E), which consists of a randomization to 7
years of letrozole, or to 2 years of tamoxifen followed by 5 years of letrozole.25–27 There will
be stratifications for HER2 status, ER-positive and/or progesterone-negative, and gene-
signature risk. These further randomizations will answer clinically relevant questions by
taking advantage of the power that the large sample size used in MINDACT offers. As the
associated biological material will be collected, there will be also ample opportunity to
develop and identify predictive gene signatures, as well as important genes and proteins
influencing response to administered agents (Figure 2).
Figure 2. Biological material flowchart in the MINDACT trial. (1) Tissue for RNA extraction. (2) Anyremaining tissue and RNA. (3) Paraffin blocks for central pathology review and tumor microarray
production. (4) Serum. (5) Tissue and/ or serum for proteomics.
Abbreviations: EIO, European Institute of Oncology; TBMB, TRANSBIG biological materials bank;
Univ Wales; University of Wales.
Center A
Center B
Center C
Agendia
TBMB
EIO
5
Univ Wales
1
3
4
2

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 242/248
Appendix. Design of the MINDACT trial
265
12
Predictive power of the 70-gene signature
At this time, there are no data on the predictive power of the 70-gene signature. It would be
interesting to have predictive power data on anthracycline–taxane-based chemotherapy,
tamoxifen, and aromatase inhibitors, because these are the treatments administered
in the MINDACT trial. The European Organisation for Research and Treatment of Cancer
(EORTC) Breast Cancer Group is now undertaking a project in which the 70-gene signature
is being evaluated in some of the patients enrolled in the EORTC 10994/BIG 00-01 ‘p53’
trial.28 The p53 trial randomized patients with locally advanced or large operable tumors
to one of two neo adjuvant chemotherapy regimens: six cycles of fluorouracil, epirubicin
and cyclophosphamide (epirubicin 100 mg/m2) or three cycles of docetaxel (100 mg/
m2) followed by three cycles of docetaxel (75 mg/m2) combined with epirubicin (90 mg/
m2). Results are not yet available, but the use of standardized chemotherapy regimens
and the availability of enough good-quality frozen material will probably yield data on the
predictive power of the signature. These results will help adjustment of estimates for the
MINDACT trial, if needed.
The MINDACT trial will provide the setting for prospectively assessing the predictive power
of the 70-gene signature and any other signatures currently being developed in response
to the chemotherapy regimens and endocrine therapy used.
Logistics
The logistics of MINDACT have been one of the most challenging and expensive parts of the
trial. All RNA extraction, quality control and microarray analysis for samples in this trial will
be performed at Agendia in Amsterdam. Indeed, at this stage this technology is probably
too immature for even the RNA extraction to be performed in external laboratories; operator
and technical variability is well known to influence the results of microarray experiments.
Upon diagnosis of a clinically node-negative invasive breast cancer, patients are eligible to
sign the first informed consent prior to surgery to allow for a sample of frozen tumor tissue
obtained during surgery to be sent to Agendia for RNA extraction (screening informed
consent). At this time, only RNA extraction and quality control check will be done. Oncethe local pathology report confirms node negativity, the genomic risk assessment will
be performed. This process will hopefully avoid much unnecessary hybridization and
hence reduce the cost. All tumor specimens will be couriered to Agendia by a specifically
contracted courier agent specialized in global express transport and storage at –80 °C. If a
patient is ineligible for the trial, her tumor material will be returned, stored in the TRANSBIG
biological materials bank, or destroyed.
Simultaneously, the investigator responsible for patient care will assess the
clinicopathologic risk using the Adjuvant! software embedded in a web-based platform
designed specifically for the MINDACT randomization. In Informed consent form 1, the

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 243/248
Chapter 12
266
patient will consent to have her risk assessed by the genomic and clinicopathologic
methods and to enter randomization for treatment (R-T) if she belongs to the discordant
group (Figure 3). If the patient is assigned to receive chemotherapy, she will be proposed to
enter the chemotherapy randomization (R-C) and to sign the Informed consent form 2.
After chemotherapy (if applicable) and radiotherapy, the endocrine therapy randomization
(R-E) will be proposed to endocrine responsive patients in the Informed consent form 3.
Paraffin tumor blocks will be sent every 6 months to the European Institute of Oncology in
Milan, for Construction of tissue arrays and for central pathology review to be performed.
Proteomic analysis of the tumor and serum samples will also be performed in the MINDACT
trial, in collaboration with the University of Wales in Aberystwyth. Additionally, since one
of the aims of MINDACT is to create a biological materials bank, frozen tumor samples (as
well as whole genome microarray data and paraffin-embedded tissue) will be collected for
all patients. The TRANSBIG biological materials bank will be located in Brussels under the
guardianship of TRANSBIG, and hence this trial will have great potential for the identification
and validation of additional gene signatures with prognostic and predictive value in early
breast cancer, as well as other markers and technologies. Figures 2 and 3 summarize some of
the logistics involved in this trial.
Figure 3. Logistics of MINDACT—tumor biopsy collection, shipment, RNA extraction and
eligibility check.
Abbreviations: ICF1, informed consent form 1; ICF2, informed consent form 2; R-T, randomization
to treatment.
Unicentric node-negative tumor
ICF1 Donation of biopsy to research
Surgery
Shipment to Agendia
RNA extractionLocal pathology
Node-positive Poor-quality RNA
Microarray analysis
ICF2 R-T
IneligibleIneligible
Node-negative Good-quality RNA

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 244/248

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 245/248
Chapter 12
268
References
1. Van de Vijver MJ, He YD, Van ‘t Veer LJ, et al. A gene-expression signature as a predictor of survival in
breast cancer. N Engl J Med 2002; 347: 1999-2009.
2. Hutchins L , Green S, Ravdin P, et al. CMF versus CAF with and without Tamoxifen in high-risk node-
negative breast cancer patients and a natural history follow-up study in low-risk node-negative
patients: First results of Intergroup trial INT 0102 [abstract #2]. Proc Am Soc Clin Oncol 1998; 17: a1
3. McShane LM, Altman DG, Sauerbrei W, et al. REporting recommendations for tumor MARKer prognostic
studies (REMARK). Nat Clin Pract Oncol 2005; 2: 416-422.
4. National Institutes of Health Consensus Development Conference Statement: Adjuvant Therapy for
Breast Cancer, November 1-3, 2000. J Natl Cancer Inst 2001; 93: 979-989.
5. Goldhirsch A, Glick JH, Gelber RD, et al. Meeting highlights: International expert consensus on the
primary therapy of early breast cancer 2005. Ann Oncol 2005; 16: 1569-1583.
6. D’Eredita’ G, Giardina C, Martellotta M, Natale T, Ferrarese F. Prognostic factors in breast cancer: the
predictive value of the Nottingham Prognostic Index in patients with a long-term follow-up that were
treated in a single institution. Eur J Cancer 2001; 37: 591-596.
7. Van ‘t Veer LJ, Dai H, Van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast
cancer. Nature 2002; 415: 530-536.
8. Van de Vijver MJ, He YD, Van ‘t Veer LJ, et al. A gene-expression signature as a predictor of survival in
breast cancer. N Engl J Med 2002; 347: 1999-2009.
9. Piccart MJ, Loi S, Van ‘t Veer LJ, et al. Multi-center external validation study of the Amsterdam 70-gene
prognostic signature in node negative untreated breast cancer: are the results still outperforming the
clinical-pathological criteria? [abstract] Breast Cancer Res Treat 2004; 88 (Suppl 1): aS38.
10. Cardoso F et al. Multi-centre independent validation of a gene prognostic signature for patients with
node-negative breast cancer (BC)—final results [abstract]. Breast Cancer Res Treat 2005; 95 (Suppl 1): aS301.
11. Adjuvant! Online [http://www.adjuvantonline.com].
12. Ravdin PM, Siminoff LA, Davis GJ, et al. Computer program to assist in making decisions about adjuvant
therapy for women with early breast cancer. J Clin Oncol 2001; 19: 980-991.
13. Olivotto IA, Bajdik CD, Ravdin PM, et al. Population-based validation of the prognostic model
ADJUVANT! for early breast cancer. J Clin Oncol 2005; 23: 2716-2725.
14. Simon R, Radmacher MD, Dobbin K, McShane LM. Pitfalls in the Use of DNA Microarray Data forDiagnostic and Prognostic Classification. J Natl Cancer Inst 2003; 95: 14-18.
15. Dudoit S et al. Comparison of discrimination methods for the classification of tumors using gene
expression data. JASA 2002; 97: 77–87.
16. De Vita Jr VT et al. (Eds; 2006) Cancer. Principles and Practice of Oncology. Philadelphia: Lippincott
Williams & Wilkins.
17. Cardoso F et al. Multi-centre independent validation of a gene prognostic signature for patients with
node-negative breast cancer (BC)—final results [abstract]. Breast Cancer Res Treat 2005; 95 (Suppl 1): aS301.
18. Buyse M, Loi S, Van ‘t Veer L, et al. Validation and clinical utility of a 70-gene prognostic signature for
women with node-negative breast cancer. J Natl Cancer Inst 2006; 98: 1183-1192.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 246/248
Appendix. Design of the MINDACT trial
269
12
19. Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for
early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet
2005; 365: 1687-1717.
20. Ross JS, Fletcher JA, Linette GP, et al. The Her-2/neu gene and protein in breast cancer 2003: biomarker
and target of therapy. Oncologist 2003; 8: 307-325.
21. Smith IE, Dowsett M, Ebbs SR, et al. Neoadjuvant treatment of postmenopausal breast cancer with
anastrozole, tamoxifen, or both in combination: the Immediate Preoperative Anastrozole, Tamoxifen,
or Combined with Tamoxifen (IMPACT) multicenter double-blind randomized trial. J Clin Oncol 2005; 23:
5108-5116.
22. ICH Harmonised Tripartite Guideline: statistical principles for clinical trials. International Conference on
Harmonisation E9 Expert Working Group. Stat Med 1999; 18: 1905–1942.
23. O’shaughnessy J, Miles D, Vukelja S, et al. Superior survival with capecitabine plus docetaxel
combination therapy in anthracycline-pretreated patients with advanced breast cancer: phase III trial
results. J Clin Oncol 2002; 20: 2812-2823.
24. Jones S et al. Three year results of a prospective randomized trial of adjuvant chemotherapy for
patients (pts) with stage I-III operable, invasive breast cancer comparing 4 courses of doxorubicin/
cyclophosphamide (AC) to 4 courses of docetaxel/ cyclophosphamide (TC) [abstract]. Proc Am Soc Clin Oncol
2003; a59.
25. Goss PE, Ingle JN, Martino S, et al. A randomized trial of letrozole in postmenopausal women after five
years of tamoxifen therapy for early-stage breast cancer. N Engl J Med 2003; 349: 1793-1802.
26. Coombes RC, Hall E, Gibson LJ, et al. A randomized trial of exemestane after two to three years of
tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med 2004; 350: 1081-
1092.
27. Thurlimann BJ et al. BIG 1–98: randomized double-blind phase III study to evaluate letrozole (L) vs.
tamoxifen (T) as adjuvant endocrine therapy for postmenopausal women with receptor-positive
breast cancer [abstract #511]. Proc Am Soc Clin O ncol 2005; 23: 16S.
28. Bonnefoi H, ebold-Berger S, Therasse P, et al. Locally advanced/inflammatory breast cancers treated
with intensive epirubicin-based neoadjuvant chemotherapy: are there molecular markers in the
primary tumour that predict for 5-year clinical outcome? Ann Oncol 2003; 14: 406-413.

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 247/248
© 2011

8/10/2019 Stella Mook T3-108
http://slidepdf.com/reader/full/stella-mook-t3-108 248/248
Stellingen
behorend bij het proefschrift
Prognostic factors in breast cancerOne fits all?
1. Voor optimale moleculaire analyse van een carcinoom zou het invriezen
van vers tumorweefsel routine moeten zijn Dit is logistiek haalbaar (o a dit