Mastigophora Zoomastigophora Phytomastigophora Intestinal & Urogenital F. Blood & Tissue F. Pathogen...
-
Upload
suzanna-lindsey -
Category
Documents
-
view
218 -
download
2
Transcript of Mastigophora Zoomastigophora Phytomastigophora Intestinal & Urogenital F. Blood & Tissue F. Pathogen...
MastigophoraMastigophoraZoomastigophora PhytomastigophoraZoomastigophora Phytomastigophora
IntestinalIntestinal & Urogenital F. Blood & Tissue F.& Urogenital F. Blood & Tissue F.
Pathogen F. : 1-Giardia lambliaPathogen F. : 1-Giardia lamblia
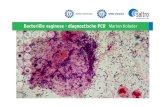
2-Trichomonas vaginalis2-Trichomonas vaginalis
3- Dientamoeba fragilis3- Dientamoeba fragilis
Non-pathogen F. : T. tenaxNon-pathogen F. : T. tenax
T. hominisT. hominis
Chilomastix mesniliChilomastix mesnili
……………………… ………………………....
Giardia LambliaGiardia Lamblia
History:History: Leeuwenhoek in 1681Leeuwenhoek in 1681 Geographic distribution: Geographic distribution: cosmopolitan parasite, more common in warm cosmopolitan parasite, more common in warm than in cool climates and in children than in cool climates and in children
Giardia LambliaGiardia Lamblia
History:History: Leeuwenhoek in 1681Leeuwenhoek in 1681 Geographic distribution: Geographic distribution: cosmopolitan parasite, more common in warm cosmopolitan parasite, more common in warm than in cool climates and in children than in cool climates and in children
Morphology:Morphology: ( body length 9 to 21 and width 5 to 15( body length 9 to 21 and width 5 to 15 µm)µm)
-Habitat: -Habitat: upper part of the small intestine, sometimesupper part of the small intestine, sometimes
in the gallbladder and in biliary drainagein the gallbladder and in biliary drainage
-anterior portion of ventral surface contain sucking disk -anterior portion of ventral surface contain sucking disk
-progressive , “ falling leaf “ motility-progressive , “ falling leaf “ motility
-pear-shaped body with attenuated posterior end-pear-shaped body with attenuated posterior end
-two nuclei and two median bodies-two nuclei and two median bodies
-three pairs flagella-three pairs flagella
Cyst form of GiaridiaCyst form of Giaridia
Cyst:Cyst:- are ovoid and measure 8 to 14 by 7 to 10 µmare ovoid and measure 8 to 14 by 7 to 10 µm- Four nuclei; four median body, Four nuclei; four median body, - numerous refractile thread in cytoplasmnumerous refractile thread in cytoplasm
Giardia lamblia cyst, Trichrome stain
Giardia lamblia cyst, Trichrome stain
PathenogensisPathenogensisPredispose factorsPredispose factors
to symptomatic giardiasis:to symptomatic giardiasis:
-Achlorhydia-Achlorhydia
-Hypogammaglobulinemia -Hypogammaglobulinemia
-Deficiency in secretory IgA -Deficiency in secretory IgA
in the small bowel in the small bowel
-Blood group A in Children-Blood group A in Children
-Bacterial colonization of the jujenum-Bacterial colonization of the jujenum
-Role of sucking disk -Role of sucking disk
-Lactose intolerance-Lactose intolerance
-Capability of normal human milk-Capability of normal human milk
to kill trophozoite of giardia in vitroto kill trophozoite of giardia in vitro
Clinical Features:Clinical Features:
The spectrum varies from asymptomatic The spectrum varies from asymptomatic carriage to severe diarrhea and malabsorption.carriage to severe diarrhea and malabsorption.
Acute giardiasis develops after an incubation Acute giardiasis develops after an incubation period of 1 to 14 days (average of 7 days) and period of 1 to 14 days (average of 7 days) and usually lasts 1 to 3 weeks.usually lasts 1 to 3 weeks.
Symptoms include diarrhea, abdominal pain, Symptoms include diarrhea, abdominal pain, bloating, nausea, and vomiting.bloating, nausea, and vomiting.
In chronic giardiasis the symptoms are In chronic giardiasis the symptoms are recurrent and malabsorption and debilitation recurrent and malabsorption and debilitation may occur.may occur.
Laboratory Diagnosis:Laboratory Diagnosis:
Giardiasis is diagnosed by the identification of cysts or Giardiasis is diagnosed by the identification of cysts or trophozoites in the feces, using direct mounts as well as trophozoites in the feces, using direct mounts as well as concentration procedures. Repeated samplings may be concentration procedures. Repeated samplings may be necessary. necessary.
In addition, samples of duodenal fluid (e.g., Enterotest) In addition, samples of duodenal fluid (e.g., Enterotest) or duodenal biopsy may demonstrate trophozoites.or duodenal biopsy may demonstrate trophozoites.
Alternate methods for detection include antigen Alternate methods for detection include antigen detection tests by enzyme immunoassays, and detection detection tests by enzyme immunoassays, and detection of parasites by immunofluorescence. Both methods are of parasites by immunofluorescence. Both methods are available in commercial kits.available in commercial kits.
Treatment:Treatment:
Several prescription drugs are available to treat Several prescription drugs are available to treat giardiasis including metronidazole and giardiasis including metronidazole and tinidazole. tinidazole.
Nitazoxanide has provided some encouraging Nitazoxanide has provided some encouraging results in the management of giardiasis in results in the management of giardiasis in children. children.
Trichomonas tenaxTrichomonas tenax(T. buccalis)(T. buccalis)
It is a small organism( 6 to 1o µm)It is a small organism( 6 to 1o µm)
Occure most frequently I pyorrheal pockets and Occure most frequently I pyorrheal pockets and tonsillar cryptstonsillar crypts
Trichomonas hominisTrichomonas hominis
Trophozoite size: 7 to 15 µm longTrophozoite size: 7 to 15 µm long
Recurrent flagellum parallels the body , running to the Recurrent flagellum parallels the body , running to the posterior end, projects behind the body as a free posterior end, projects behind the body as a free flagellumflagellum
Causal Agent:Causal Agent:
Trichomonas vaginalisTrichomonas vaginalis, a flagellate, is the , a flagellate, is the most common pathogenic protozoan of most common pathogenic protozoan of humans in industrialized countries.humans in industrialized countries.
Geographic DistributionGeographic Distribution
Worldwide. Higher prevalence among Worldwide. Higher prevalence among persons with multiple sexual partners or persons with multiple sexual partners or other venereal diseases.other venereal diseases.
Predispose factorsPredispose factors::- Ph changes- Ph changes- Bacterial flora change- Bacterial flora change- Physiological changes- Physiological changes
Pathogenesis:Pathogenesis:-At least four surface protein contribute in host cell -At least four surface protein contribute in host cell
adherence.adherence.
-Contact- dependent cytopathic effect-Contact- dependent cytopathic effect
( kill target cells by direct contact without phagocytosis)( kill target cells by direct contact without phagocytosis)
-Produce a cell-detaching factor-Produce a cell-detaching factor
Clinical Features:Clinical Features:
Trichomonas vaginalisTrichomonas vaginalis infection in women is infection in women is frequently symptomatic. frequently symptomatic.
Vaginitis with a purulent discharge is the Vaginitis with a purulent discharge is the prominent symptom, and can be accompanied prominent symptom, and can be accompanied by vulvar and cervical lesions, abdominal pain, by vulvar and cervical lesions, abdominal pain, dysuria and dyspareunia. dysuria and dyspareunia.
The incubation period is 5 to 28 days. In men, The incubation period is 5 to 28 days. In men, the infection is frequently asymptomatic; the infection is frequently asymptomatic; occasionally, urethritis, epididymitis, and occasionally, urethritis, epididymitis, and prostatitis can occur. prostatitis can occur.
Laboratory Diagnosis:Laboratory Diagnosis:Microscopic examination of wet mounts may establish Microscopic examination of wet mounts may establish the diagnosis by detecting actively motile rganisms. This the diagnosis by detecting actively motile rganisms. This is the most practical and rapid method of diagnosis is the most practical and rapid method of diagnosis (allowing immediate treatment), but it is relatively (allowing immediate treatment), but it is relatively insensitive.insensitive.
Direct immunofluorescent antibody staining is more Direct immunofluorescent antibody staining is more sensitive than wet mounts, but technically more complex.sensitive than wet mounts, but technically more complex.
Culture of the parasite is the most sensitive method, but Culture of the parasite is the most sensitive method, but results are not available for 3 to 7 days.results are not available for 3 to 7 days.
In women, examination should be performed on vaginal In women, examination should be performed on vaginal and urethral secretions. and urethral secretions.
In men, anterior urethral or prostatic secretions should In men, anterior urethral or prostatic secretions should be examined.be examined.
TreatmentTreatment
Treatment should be implemented under Treatment should be implemented under medical supervision, and should include all medical supervision, and should include all sexual partners of the infected persons. sexual partners of the infected persons.
The drugs of choice for treatment are The drugs of choice for treatment are metronidazole and tinidazole; therapy is usually metronidazole and tinidazole; therapy is usually highly successful. Strains of highly successful. Strains of Trichomonas Trichomonas vaginalisvaginalis resistant to both drugs have been resistant to both drugs have been reported. reported.
Balantidium coliBalantidium coliCausal Agent:Causal Agent:
Balantidium coliBalantidium coli, a large ciliated protozoan , a large ciliated protozoan parasite parasite
Geographic DistributionGeographic Distribution
Worldwide. Because pigs are an animal Worldwide. Because pigs are an animal reservoir, human infections occur more reservoir, human infections occur more frequently in areas where pigs are raised. Other frequently in areas where pigs are raised. Other potential animal reservoirs include rodents and potential animal reservoirs include rodents and nonhuman primates.nonhuman primates.
Clinical FeaturesMost cases are asymptomatic. Clinical
manifestations, when present, include persistent diarrhea, occasionally dysentery, abdominal pain, and weight loss. Symptoms can be severe in debilitated persons
Laboratory DiagnosisLaboratory Diagnosis
Diagnosis is based on detection of trophozoites in Diagnosis is based on detection of trophozoites in stool specimens or in tissue collected during stool specimens or in tissue collected during endoscopy. Cysts are less frequently endoscopy. Cysts are less frequently encountered. encountered.
Balantidium coliBalantidium coli is passed intermittently and once is passed intermittently and once outside the colon is rapidly destroyed. Thus outside the colon is rapidly destroyed. Thus stool specimens should be collected repeatedly, stool specimens should be collected repeatedly, and immediately examined or preserved to and immediately examined or preserved to enhance detection of the parasite enhance detection of the parasite
































![&ï D 1* 2( q...2014/05/09 · オF4*FヤFクFGFF#ユq7F&リFG&KF64FGFケ FFヲFアFンFFワ1GGGFⅶヤメFク>FンF4E・FFFFツp'g$ラFテFFFヤFリ FFヤFケ ゥF0ヲFGFンFFクィ]F4E・G"+FFGp'g$ラFDリFS(F・F瓰Fクp'g](https://static.fdocuments.nl/doc/165x107/5e9de550f51c446c6f01eeef/-d-1-2-q-20140509-if4fififgffiq7fifgkf64fgfi.jpg)


![f,f]il[ Ë=ffi ffi](https://static.fdocuments.nl/doc/165x107/5875e8641a28ab457b8ba96e/ffil-effi-ffi.jpg)