PJNM6-Draft Online Final 2pjnm.net/uploads/3/3/0/9/3309018/pjnm6-draft_online_final_2.pdf · Dr...
Transcript of PJNM6-Draft Online Final 2pjnm.net/uploads/3/3/0/9/3309018/pjnm6-draft_online_final_2.pdf · Dr...


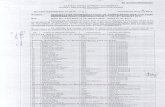
Official journal of Pakistan Society of Nuclear Medicine
EDITOR-IN-CHIEFQaisar Hussain Siraj
ASSOCIATE EDITORSDr Khalid NawazDr Ahmad QureshyDr Abida RazaDr Shoaib ShahDr Aakif Ullah Khan
Dr Maseeh uz ZamanDr Akhtar AhmedDr M Babar ImranDr Sadiq Hussain Nohario
Pakistan Journal ofNuclear Medicine
INTERNATIONAL EDITORIAL BOARD
Dr John Zaknun, IAEA, ViennaProf Seyed Rasoul Zakavi, IranProf A H Elzaggar, KuwaitProf G T Krishnamurthy, USAProf Hee-Seung Bom, S KoreaDr Kottekatu K Balan, UKProf G S Pant, Saudi ArabiaProf Omar Alonso, UruguayDr John R Buscombe, UK
Dr Frederic Fahey, USAProf Giuliano Mariani, ItalyDr G M Shah, Saudi ArabiaDr Thomas Pascal, PhilippinesProf Ali Nawaz Khan, UKDr Michael Masoomi, UKDr Jamshed B Bomanji, UKProf Richard Underwood, UKProf A J B McEwan, Canada
NATIONAL EDITORIAL BOARD
Dr Humayun BashirDr Saima HaiderDr Nasir MahmoodDr H Ghulam AbbasDr Mujahid Khalid AliDr Riffat HussainDr Syed Shahid IqbalDr Shahab Fatimi
Dr Mohsin Saeed SheikhDr Amjad Aziz KhanDr M Numair YounisMr Asdar ul HaqMr Farrukh HameedDr M Adnan SaeedDr Saima Riaz
P J N MMANAGING EDITORMohammad Sohaib
FOUNDING EDITORSQaisar Hussain SirajDurr-e-Sabih

Editorial Office
Department of Medical Sciences,
Pakistan Institute of Engineering and Applied Sciences (PIEAS)
Nilore, Islamabad-45650, PAKISTAN
(+92 (51) 1111 74327 (3310); 7+92 (51) 924 8600
PJNM Pakistan Journal ofNuclear Medicine

Durr-e-Sabih. Whither Nuclear Medicine Training in Pakistan? Pak J Nucl Med 2016;6:1-2.
Akhtar M, Hussain JA, Ali A, Akhtar S. Estimation of time for release of patients after theadministration of I-131 to thyrotoxicosis patients. Pak J Nucl Med 2016;6:3-10.
Rasulova N, Arybzhanov D, Lyubshin V, Abdikhakimov A, Sagdullaev S, Nishonov S, ArifhodjaevG, Shakirova Y, Krylov V, Khodjibekov M. Lactate dehydrogenase (LDH) as predictive factor ofthe pain free syndrome duration after radionuclide treatment of bone metastases in patientswith breast cancer. Pak J Nucl Med 2016;6:11-18.
Sohaib M, Shenoy MU, Kellett MJ, Duffy PG, Gordon I. Assessment of renal parenchymal damageby DMSA after PCNL procedure in children using adult-sized equipment . Pak J Nucl Med2016;6:19-24.
Jabeen A, Mushtaq S, Raza H, Memon MA. Vitamin B12 deficiency: prevalence and evaluationof a reversible co-morbidity in hypothyroid patients. Pak J Nucl Med 2016;6:25-31.
Qureshi SZ, Shah FH, Waqar MA. Validation of Ottawa ankle rule utilizing radionuclide skeletalscintigraphy. Pak J Nucl Med 2016;6:32-41.
Khan AU, Hameedullah, Shah AS, Khattak MR. Radiosynoviorthesis in pigmented villonodularsynovitis using rhenium-188 labelled tin colloid: a case report. Pak J Nucl Med 2016;6:42-47.
Sahel OA, Ghfir I, Guerrouj H, Benameur Y, Benraiss N. Unusual spinal metastases from anadenoid cystic carcinoma of the maxillary sinus seen on a bone scan: a case report. Pak J NuclMed 2016;6:48-52.
Ghfir I, Achir A, Guerrouj H, Oueriagli SN, Sahel OA, Aouad NB. SPECT/CT imaging of primarymediastinal goitre: case report and literature review. Pak J Nucl Med 2016;6:53-58.
Almenieir N, Hassoun H, MacKenzie K, Derbekyan V. SPECT/CT for the accurate localization of67Ga uptake in mycotic abdominal aortic aneurysm. Pak J Nucl Med 2016;6:59-62.
Rasulova N, Siraj QH, Javaid A, Al-Banna A. Functional ectopic cystic parathyroid adenomas:case reports and literature review. Pak J Nucl Med 2016;6:63-68.
Khaled K, Javaid A, Siraj QH. Pulmonary arteriovenous malformation diagnosed on 18F-fluorodeoxyglucose PET/CT scan. Pak J Nucl Med 2016;6:69-71.
Nabih SO, Guerrouj HE, Ghfir I, Raïs NB. Multifocal osteomyelitis on bone scan performed formandibular mass with uncertain malignancy. Pak J Nucl Med 2016;6:72-74.
Siraj QH, Javaid A, Khaled K, Al-Banna A. Unsuspected chronic multifocal osteomyelitis diagnosedon a whole-body 18F-FDG PET/CT scan. Pak J Nucl Med 2016;6:75-78.
PJNM Pakistan Journal ofNuclear Medicine

Whither Nuclear Medicine Training in Pakistan?
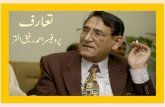
Durr-e-Sabih
EDITORIAL
I hear there is stirring in the usually ossifiedhalls of nuclear medicine higher learning andthose at the helm of affairs are realizing, orsaying that they are realizing, the importanceof teaching cross-sectional anatomy to theyoung trainees of this fascinating specialty.This is the only way of keeping nuclearmedicine physicians relevant.
Hats-off to the current PSNM executive councilto have taken on this project with somethingof a missionary zeal, and thus the plethora ofshort courses in cross-sectional anatomy.While this is good, it does not replace need offormal training for young trainees andretraining with some sort of certification andassurance of basic competence of thepractitioners of this art.
As an examiner of the Asian Nuclear MedicineBoard, I get to interact with young (and somenot-so-young) nuclear medicine physiciansfrom many countries of Asia. I have yet to beimpressed by a candidate from our country.In the small sample that I have had theprivilege of interacting, I have realized that itis not only the lack of knowledge thatdistinguishes our candidates, it is the lack of"thinking", the lack of trying to use all of theavailable information and the lack ofconfidence in clinical problem solving and thelack of any understanding of a CT or MR image.Why is this resistance to learn cross-sectionalimaging, hasn't it been an issue for almost 20years [1].
It hurts because I see so many highlyintelligent physicians doing nuclear medicine.That they should be so mediocre whenreporting a nuclear medicine procedure is
disappointing and even demoralizing.
Our statistics say a lot, something that I havebeen heckled at for quoting. Even today ourtrainee numbers show a depressing trend withonly 17 FCPS trainees and 14 MS trainees; MDtraining positions remain unfilled as do the PETfellowship positions. Generally, we have hadmore faculty in nuclear medicine than trainees,and that is also true today. Being "faculty"looks good on your CV and who cares ifyouearn your title or not.
In a country that graduates over 14000physicians annually, a country where radiologyhas about a thousand trainees at any giventime, less than 30 nuclear medicine traineesmeans that this specialization is not attractive.Everyone who argues otherwise is misguidedat best.
In fact we conducted a professionalsatisfaction survey in 2013 and found thatalmost 60% of practicing nuclearmedicinephysicians were unhappy professionally, mostcommonly with the quality of training they hadreceived [2]. Of those who trained in nuclearmedicine, almost a fifth changedtheirspecialization [3], something quite unheardof in any other specialty. This was somethingthat should have sent our faculty at institutesof training into a huddle. They did huddle, butto circle their wagons instead of trying to figureout what to do to address this issue. Onegentleman from one institute suggested thatthe placement of nuclear medicine trainingopportunities in a shared newspaper ad wasthe reason for lack of interest…. I wish he was
PJNM 2016, 6:1-2 331691 © 2016 Pakistan Society of Nuclear Medicine
www.pjnm.net 2221-0288(201601/01)6:1<01:WNMTIP>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 2
joking but he wasn't. Another very seniorperson starts all nuclear medicine trainingdiscussions with his opinion that the PAEC'smandate does not include nuclear medicineor nuclear medicine training.. another gentleman,again a shining tower of nuclear medicinetraining sat for several years on a file witha new training curriculum.
As we slowly reach a critical mass of PETscanners and, as attractive business modelsdevelop that can justify this investment,we will attract another kind of attention,that of our imaging big brothers, the radiologists….I have heard the argument as I am sureall of you have too, that they are alreadytrained in cross-sectional anatomy; theyhave trained in the PET technique and theycan chase a hot spot as well as any nuclearmedicine physician… so it makes sense forthem to take ownership of this techniqueand the associated resources.
This has already happened in many places,and in the US there was a move to doaway with nuclear medicine residenciesaltogether, thankfully this was aborted inthe face of international opposition fromthe nuclear medicine community. The clamourhas died down for now, but surely not forlong and we will see turf battles and newwars for resources.
PET-CT will live on, patients will continueto get services, and very competently Iam sure, but whereas radiology is solid,structured and overt, nuclear medicine issubtle and abstract and has one eye alwayson the lab bench.
Nuclear medicine physicians can join dotsthat are only faintly visible, their conclusionsare often interpolative and their art is atacquiring moving targets, biochemistry,radiochemistry, pathology, physiology, etc.,which all interplay before a nuclear medicineopinion is formed… it would be unfortunateif nuclear medicine physicians were to becomeextinct, to be replaced only by full timeresearchers in labs and full time radiologistsin the imaging suites.
After this jeremiad, you would expect meto come up with solutions too…. Well hereis what comes to mind. Strengthen, strengthen,strengthen the training programmes, makeit more broad based. It takes time to overcomeinertia of changing curriculum at the universityor college level, but a Pakistan School ofNuclear Medicine, sponsored by the PSNMbut not controlled by it so that it can remain
non-partisan and focused only on its job,would be one solution. The only job thatthe school would have is look at the weaknessesin the current training programs and offercertification courses to fill these knowledgegaps. We can get this expertise locally oruse our network with the Asian School ofNuclear Medicine to get faculty and courses.I am very happy that this idea (initiallyfloated by the present President PSNM) isgetting traction among those in the Pakistaninuclear medicine community who feel thereis need to fix things.
Frankly I think those at the helm of trainingaffairs have played their innings and needto go home. A changing of the guards islong due, let younger, more mentally agile,more committed members of the communitytake on the training challenge. We needsomeone new, someone who can rise tothe challenge; design a new curriculum,weed out the obsolete and include the relevant.We should look at the success stories aroundus, even Iran, living under such heavy constraintsfor so long has managed to train superbnuclear medicine physicians (an Iranian ladyphysician stood first in the last year's ANMBexam); India can boast of world class facilitiesmanned by world class personnel. Whathave we not that the others have? Onlythe will to give all; once we have that will,I am there will be no turning back.
PS: Please disagree, I would love to seeopinion to the contrary and hope this wouldbe published in these very pages.
References
1. Sabih D. Nuclear Medicine in the ThirdWorld; Which way to go? Nucl Med Commun,1997;18:2.
2. Sabih D. Professional satisfaction surveyamong young nuclear medicine physiciansof Pakistan. the Challenges ahead. PJNM,2012;2(2):6.
3. Sabih D. Future Nuclear Medicine Physiciansin Pakistan. Rare and Valuable or Extinctand Unnoticed? PJNM, 2012. 2(1):3.
Note
The views expressed in the Editorial are thoseof the author alone with the journal or thePSNM taking no responsibility for the contentsor the opinion.
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:1-2

Estimation of time for release of patients afterthe administration of I-131 to thyrotoxicosis
patients
Muhammad Akhtar*, Jawad Akhtar Hussain, Akbar Ali,Sheraz Akhtar
Institute of Nuclear Medicine, Oncologyand Radiotherapy (INOR), Abbottabad
REVIEW ARTICLE
*Correspondence
Muhammad Akhtar Institute of Nuclear Medicine, Oncology & Radiotherapy (INOR) Abbottabad, Pakistan Tel: +923135877199 Email: [email protected]
Abstract
Radioactive iodine (I-131) has been used formore than six decades for the treatment ofthyrotoxicosis. Radiation safety is ofparamount importance in I-131 basedtreatment of thyroid diseases, as treatedpatients become a potential radiation hazardfor other individuals [1]. The purpose of thisarticle is estimation of the time period forradiation safety restrictions throughassessments of total effective dose equivalent(TEDE) in individuals exposed to I-131 forthyrotoxicosis therapy, by incorporating intothe calculations, various factors such asrelevant socioeconomic conditions.
For performing patient-specific dosecalculations, we have used published data ofuptake fractions & effective half-lives andtriexponential model for total body clearanceof iodine-131 [2].
Results obtained showed that the TEDEto other individuals (especially the family
members, particularly children) and generalpublic may be much higher than the annualdose limits recommended by the InternationalAtomic Energy Agency (IAEA) andInternational Commission for RadiationProtection (ICRP) in some situation especiallywhen the administered activity is greater than15 mCi and occupancy factor greater than0.125 and proper precautionary measures arenot taken after the release from hospital [1,3].
It is therefore suggested that a fixed dose limitof 15 mCi (550 MBq) instead of 30 mCi (1100MBq) be recommended for release of I-131thyrotoxicosis therapy patients in order toreduce undesired exposure to caregivers andgeneral public in countries like Pakistanbecause of factors such as poor socio-economic conditions and low literacy rates,etc.
Key words: Iodine-131 therapy,thyrotoxicosis, patient release
Introduction
Use of unsealed radionuclide therapy to treata variety of diseases has become commonthroughout the world for several decades.I-131 is a useful reference therapeuticradionuclide because of its widespread use
PJNM 2016, 6:3-10 331691 © 2016 Pakistan Society of Nuclear Medicine
www.pjnm.net 2221-0288(201601/01)6:1<03:ETRPAI>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 4
and the presence of an external radiation fieldfrom its energetic gamma emissions [1].
The only disadvantage of this method is thatit may lead to higher radiation exposure to thefamily members of the patient and the generalpublic if precautionary measures are not takenafter release from the hospital.
The dose received by the family members andgeneral public depends totally upon theconduct of the patient. This is because of thefact that a member of public will not realisethat the person sitting next to them is highlyradioactive [4].
The physical half-life of I-131 is about 8 days.The main decay product is xenon-31, which israpidly washed out of the body. In addition,damaged thyroid cells lose their capacity toorganify iodine and consequently, the iodine isreleased back to the blood stream, resulting inexcretion. Thus, I-131 is removed from thebody reasonably quickly, either due toradioactive decay or by metabolic excretion.The total amount of I-131 reduces to half itsoriginal value at a rate which depends on thestate of disease: between 1 day, in the case ofthyroid cancer and total ablation of thyroidtissue, and 7 days for patients with euthyroidgoitre. In the case of hyperthyroidism, theeffective half-life is about 4-5 days [2, 5].
When the patient is kept in the hospitalfollowing radionuclide therapy, the people atrisk of exposure include hospital staff, who mayor may not be radiation workers or carers. Thisis a significant problem. However, it isgenerally felt that it can be effectively managedwith well-trained staff and appropriatefacilities. On the other hand, once the patienthas been released, the group at risk includemembers of the patient's family, includingchildren and carers. They may also includeneighbours, visitors to the household, co-workers, those encountered in public places,on public transport or at public events andfinally the general public. To avoid theseproblems, certain precautionary measureshave to be taken to minimise the dosedelivered to the general public. Therefore, to
keep the doses to general public as-low-as-reasonably-achievable (ALARA), the patientand his/her attendant should be properlyeducated in this regard.
There are significant radiation protectionproblems relating to management ofradioactive patients. The pattern of practicearound the World with regard to the release ofpatients from hospital after therapy withunsealed radionuclides is quite varied.Specifically, there is no agreement on whetherit is necessary to hospitalize patientsundergoing therapy, and, if so, when and underwhat conditions they can be released. [1].
Current recommendations in accordance withregulatory requirements, regarding release ofpatients after therapy with unsealedradionuclides is based on one of the followingoptions:1. Release of patients based on patient-
specific dose calculations/dose limits2. Release of patients based on administered
activity/residual activity3. Release of patients based on measured
dose rate at 1 m
The United States Nuclear RegulatoryCommission (NRC) regulations for the releaseof patients administered radioactive material(10 CFR 35.75) authorize patient releaseaccording to a dose-based limit, i.e., the doseto other individuals exposed to the patient. Alicensee may release patients, regardless ofadministered activity, if it can be demonstratedthat the TEDE to another individual fromexposure to a released patient is not likely toexceed 5 mSv and the TEDE to a member ofthe general public is not likely to exceed 1 mSv.Furthermore, in a case where the dose couldexceed 1 mSv, the patient is also to beprovided with instructions on how to maintaindoses to others as per ALARA principle [2, 6].
The Radiation Protection unit of the EuropeanCommission, in its last guide, proposed doselimits related to age and family bonds. Forfamily and close friends, the proposed limitswere 1 mSv/y for children (including unborn
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:3-10

PJNM 2016, Volume 6, Number 1 5
children), 3 mSv/y for adults ≤60y old, and 15mSv/y for adults >60y old. For third parties orthe general public, the proposed limit was 0.3mSv/y [7].
The IAEA recommends that the dose to anycomforter or visitor shall be constrained so thatit is unlikely that his or her dose will exceed 5mSv during the episode of a patient'sdiagnostic examination or treatment. The doseto children visiting patients who have receivedradioactive materials should be similarlyconstrained to less than 1 mSv [1, 8].
This article provides some guidance/help tothe medical professionals involved in releaseof patients after therapy with I-131. Also thereis suggestion for local regularity body forre-considering of the existing release limit inthe light of our own socioeconomic conditions,family traditions etc. instead of fixed limit of1100 MBq (30 mCi).
Methods & Materials
The methodology for calculation of absorbeddose (or TEDE) from an external source, suchas a patient or a spill on the floor, wasdescribed in Appendix-I of NCRP 37. Othermethods were suggested in the more recentAppendix-U of NUREG-1556 Vol. 9 (the NRCguidance associated with the patient releaserule pursuant to 10 CFR 35.75), NCRP ReportNo. 155, a Society of Nuclear Medicine (SNM)guidance document, and other references atthe end of this document.
Equation to calculate the TEDE from a patientadministered I-131 may have threecomponents. Dose for the first eight-hournon-void period (pre-equilibrium period) withan occupancy factor of 0.75, the dose fromthe extrathyroidal component from 8 hours tototal decay and the dose from the thyroidalcomponent from 8 hours to total decay.
During the first 8 hours (0.33 day) afteradministration, little biologic elimination ofI-131 occurs. Effective half-life of I-131 duringthis period is considered constant, although
some inter-patient variability exists andestimated to be 80% of physical half-life [2,5, 6].
After the pre-equilibrium period, the remainingI-131 is considered to be divided betweenthyroidal component and extrathyroidalcomponent. The effective half-lives of I-131 ineach of these components is different. Theeffective half-lives of I-131 for thyroidal andextrathyroidal components also vary frompatient to patient but were assume to beconstant in our calculations as given in Table1.
These equations do not include the dose frominternal intake by household members andmembers of the public, because the dose fromintake by other individuals is expected to besmall (less than a few percent), relative to theexternal gamma dose [5]. Specific gamma rayconstants (Г) for I-131 is 2.2 rem-cm2/mCi-h.
Occupancy Factor (OF) is the fraction of time,a person spends near the patient (~at 100 cmdistance) in 24 hr cycle. OF is the estimate ofthe patient's proximity to people at home orin the community after dose administration.
OF=0.125 (3 hr/24 hr) 12.5% timeOF=0.33 (8 hr/24 hr) 33% timeOF=0.5 (12 hr/24 hr) 50% timeOF=01 (24 hr/24 hr) 100% time
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:3-10
Extra thyroidalComponent
Thyroidal Component
Medical Condition UptakeFraction(F1)
EffectiveHalf-lifeT eff-1 (day)
UptakeFraction(F2)
EffectiveHalf-lifeT eff-2(day)
Hyperthyroidism 0.20 0.32 0.80 5.2
thyroid cancer * 0.95 0.32 0.05 7.3
*Post-thyroidectomy
Table 1 Uptake fraction and effective half-lives for I-131 [4, 8]

PJNM 2016, Volume 6, Number 1 6
Equations
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:3-10
( ) ( ) ( ){ st component nd component rd component }D 0®t) = 1 - + 2 - + 3 -(
WhereD (0 ® t ) Total effective dose equivalent at time t, in rem (1 rem=10 mSv)34.6 Conversion factor, 24 hrs/day times the total integration of decay(1.44)0.75 is the occupancy factor for first 8 hours8.04 (d) physical half- life of I-1310.8 factor of 80%for first 8 hours clearance through physical decayG Specific gamma ray constant in rem/mCi-h at 1 cm (2.2 for I-131)A Activity in mCi at the time of the releaseOF Occupancy Factor from 8 hours to total decayF1 Extrathyrodial Uptake FractionF2 Thyrodial Uptake FractionTeff Effective half-life in daysT Exposure time in daysr Distance from the source to the point of interest in cm (1 m=100cm)
( )A(mCi)e 1 1( )
2( 2 )
0.693
8.040.33-0.693́2
)(8
eff 11 e T34.6
)(2ndr cm
dTFOFhmCi
cmrem
remDthyroidalextra-
t
eff
thr®
ïþ
ïýü
ïî
ïíì
÷÷
ø
´ ö
çç
è
æ-´´´÷÷
ø
öççè
æ-
-G´
==
-
-
-
( )A(mCi) 2 2 ( )
2 ( 2 )
0.693
8.040.33-0.693́2
)(8
eff 21 e T34.6
)(3rdr cm
dTFOFehmCi
cmrem
remDthyroidal
t
eff
thr®
ïþ
ïýü
ïî
ïíì
÷÷
ø
´ ö
çç
è
æ-´´´÷÷
ø
öççè
æ-
-G´
==
-
-
-
( )( ) 0.75
2 ( 2 )
8.040.330.6932
)8(0
1)8.04(d0.834.6
1st =r cm
emCi´ AhmCi
cmrem
remD ® hr
ïþ
ïýü
ïî
ïíì
÷÷ø
öççè
æ-´´÷÷
ø
öççè
æ-
-G´
=
´-
Results & Discussion
Figures 1 (a, b, c, d, e & f) are showingvariation of TEDE with time for differentadministered activities (10, 15, 20, 25 and 30mCi) at fixed distance of 100 cm (1m) and0.125, 0.25, 0.33, 0.5, 0.75 & 1.0 occupancyfactors respectively.
Fig. 1(a) shows that TEDE approaches to andexceeds from limit of 1 mSv (i.e. for childrenand general public) if patient withadministrative activity of I-131 > 15 mCi,spends 3 hour per day (OF=0.125) close toother individuals for first 15 days after therapy.Similarly, from Fig. 1 (d, e, f) it is clear thatTEDE to other individuals who spends more

PJNM 2016, Volume 6, Number 1 7
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:3-10
0123456789
10
0 5 10 15 20 25
TEDE
(mSv
)
Time (days)
a (OF=0.125)
10 mCi
15 mCi
20 mCi
25 mCi
30 mCi
0123456789
10
0 5 10 15 20 25
TEDE
(mSv
)
Time (days)
b (OF=0.25)
15 mCi
10 mCi
20 mCi
25 mCi
30 mCi
0123456789
10
0 5 10 15 20 25
TEDE
(mSv
)
Time (days)
c (OF=0.33)
10 mCi
15 mCi
20 mCi
25 mCi
30 mCi
0123456789
10
0 5 10 15 20 25
TEDE
(mSv
)
Time (days)
d (OF=0.5)
10 mCi
15 mCi
20 mCi
25 mCi
30 mCi
0123456789
10
0 5 10 15 20 25
TEDE
(mSv
)
Time (days)
e (OF=0.75)
10 mCi
15 mCi
20 mCi
25 mCi
30 mCi
0123456789
10
0 5 10 15 20 25
TEDE
(mSv
)
Time (days)
f (OF=1.0)
10 mCi
15 mCi
20 mCi
25 mCi
30 mCi
Figure 1 Total Effective Dose Equivalent (TEDE) to other individual w.r.t time he/she spentwith patient having I-131 therapy for different administered activities (10, 15, 20, 25 and30 mCi) taking fixed distance of 100 cm and for Occupancy Factors (a) 0.125, (b) 0.25,(c) 0.33, (d) 0.5, (e) 0.75 & (f) 1.0

PJNM 2016, Volume 6, Number 1 8
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:3-10
Figure 2 Total Effective Dose Equivalent (TEDE) to other individual w.r.t distance frompatient having I-131 therapy for different administered activities (10, 15, 20, 25 and 30mCi) during first 30 days from I-131 administration and for Occupancy Factors (a) 0.125,(b) 0.25, (c) 0.33, (d) 0.5, (e) 0.75 & (f) 1.0
0123456789
10
25 50 75 100 125 150 175 200
TEDE
(mSv
)
Distance (cm)
a (OF=0.125)
10 mCi
15 mCi
20 mCi
25 mCi
30 mCi
0123456789
10
25 50 75 100 125 150 175 200
TEDE
(mSv
)
Distance (cm)
b (OF=0.25)
10 mCi
15 mCi
20 mCi
25 mCi
30 mCi
0123456789
10
25 50 75 100 125 150 175 200
TEDE
(mSv
)
Distance (cm)
c (OF=0.33)
10 mCi
15 mCi
20 mCi
25 mCi
30 mCi
0123456789
10
25 50 75 100 125 150 175 200
TEDE
(mSv
)
Distance (cm)
d (OF=0.5)
10 mCi
15 mCi
20 mCi
25 mCi
30 mCi
0123456789
10
25 50 75 100 125 150 175 200
TEDE
(mSv
)
Distance (cm)
e (OF=0.75)10 mCi
15 mCi
20 mCi
25 mCi
30 mCi
0123456789
10
25 50 75 100 125 150 175 200
TEDE
(mSv
)
Distance (cm)
f (OF=1.0)
10 mCi
15 mCi
20 mCi
25 mCi
30 mCi

PJNM 2016, Volume 6, Number 1 9
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:3-10
time per day (i.e. OF>0.5) with I-131 (>15mCi) therapy of patients, approaches to andexceeds from 5 mSv (limit for adult familymembers/caregivers) within 2-3 weeks.
Figure 2 (a, b, c, d, e & f) shows variation ofTEDE (during first 30 days after I-131administration) with distance from patient fordifferent administered activities (10, 15, 20,25 and 30 mCi) for 0.125, 0.25, 0.33, 0.5,0.75 & 1.0 occupancy factors respectively.
Figure 2a shows that if the patient withadministered activity of I-131 >15 mCi doesnot maintain the distance of 1m or greaterfrom other individuals, the limit of 1 mSv (i.e.for children and general public) will exceedvery quickly, even for OF=0.125 (i.e. if he/shespends 3 hour per day closer to otherindividual) for 1 month after I-131administration.
Similarly, Figure 2(d,e,f) shows that for OF >0.5, TEDE approaches to and exceeds 5 mSvwhen the patient does not maintain thedistance of 1m or greater from other individualfor administered activity of I-131 >15 mCi.
After I-131 therapy, doses to comforters &carers, family members, the public, co-workersand others need to be limited or constrainedin accordance with the National andInternational Regulations. The controlarrangements should focus on the dose limitsor dose constraints that are generally applied.The decision to hospitalise or release a patientshould be determined on an individual basis.Individuals differ not only in their socialsituations but also in the activity clearancerates from the body. This decision should takeinto account many factors, including thepatient's wishes, their medical circumstances,the regulatory environment, occupational andpublic exposures, family considerations, costand environmental factors [1].
The first few hours after administration of theI-131 are crucial. If someone spends 3 to 4hours closer than 50 cm to the patient afteradministration, the dose limit could quicklybe reached or exceeded. Exposures to other
individuals can be effectively managed by theeducated patient (or parent or guardian) afterrelease if that patient follows the instructionsprovided. There are three major elementsinvolved in successfully meeting a performancestandard of maintaining exposure of membersof the public to released I-131 therapypatients:
1. The evaluation of the patient's living andworking conditions to ascertain whether ornot a given patient can be safely released.
2. The appropriate performance of a patient-specific dose calculation to ensure that noindividual member of the public will likelybe exposed to a dose in excess of limits.
3. To provide verbal and written instructionsthat are simple in order for the patient tolimit the radiation dose to others as perALARA principle. This requires patienteducation and an assessment by theauthorized physician that patientcompliance with these instructions is highlylikely.
Conclusion
Existing fixed release limit of 30 mCi (1100MBq) for I-131 therapy of thyrotoxicosispatients may be re-evaluated and should bedetermined on individual basis, consideringtheir life style, socioeconomic conditions andfamily background etc. for a country likePakistan where mostly families do not haveadequate facilities for isolating the patients attheir home and many of them are unable tofollow instructions given to them at the timeof release from the hospital due to ignorance,i.e. low literacy rate. Alternatively, a fixeddose limit of 15 mCi (550 MBq) instead of thestandard 30 mCi (1100 MBq) dose, may berecommended for release of I-131thyrotoxicosis therapy patients.
References
1. Release of Patients after RadionuclideTherapy, Safety Reports Series No.63, IAEAVIENNA, 2009.

PJNM 2016, Volume 6, Number 1 10
2. US Nuclear Regulatory Commission.Specific Guidance about Medical UseLicenses (NUREG-1556, Vol. 9, Rev. 2)2008
3. International Commission of RadiologicalProtection, Release of Patients afterRadionuclide Therapy with UnsealedRadionuclides, Publication 94, Elsevier,Oxford (2004).
4. Wazir Muhammad et all, Release Criteriafrom Hospitals Of I-131 ThyrotoxicosisTherapy Patients in Developing Countries-Case Study, Radiation Protection Dosimetry(2006), Vol. 121, No. 2, pp. 136-139
5. Radiation Safety in the Treatment ofPatients with Thyroid Diseases byRadioiodine I-131: PracticeRecommendations of the American ThyroidAssociation, THYROID Volume 21, Number4, 2011
6. US Nuclear Regulatory Commission,Release of Patients AdministeredRadioactive Materials: Regulatory Guide8.39, April 1997.European Commission,Radiation Protection Following Iodine- 131Therapy (Exposures due to Out-patients orDischarged In-patients), RadiationProtection 97, European Commission,Luxembourg (1998).
7. IAEA, Radiological protection for medicalexposure to ionizing radiation, Safety Guideno. RS-G-1.5. 2002, Vienna.
8. Carlos D. Venencia et al., Hospitaldischarge of patient with thyroid carcinomatreated with 131I, The Journal of NuclearMedicine, Vol. 43, No. 1, January 2002.
9. International Commission on RadiologicalProtection, Recommendations of the ICRP,Publication 103, Elsevier, Oxford (2008).
Pak J Nucl Med 2016;6:3-10 2221-0288(201601/01)6:1<03:ETRPAI>2.0.TX;2-M

Lactate dehydrogenase (LDH) as predictivefactor of the pain free syndrome duration afterradionuclide treatment of bone metastases in
patients with breast cancer
Nigora Rasulova1, Dauranbek Arybzhanov2, VladimirLyubshin3, Abdulla Abdikhakimov5, Shamsutdin Sagdullaev5,Sherzod Nishonov6, Gayrat Arifhodjaev1,Yuliya Shakirova1,
Valery Krylov4,Marat Khodjibekov1
1Nuclear Medicine Department, Republic Specialized Centre of Surgery,Tashkent, Uzbekistan
2Department chemotherapy and endovascular oncology, South KazakhstanOntological Clinic, Shimkent, Kazakhstan
3Private Clinic "Vegamed" Tashkent, Uzbekistan4Department of Radionuclide Therapy, Medical Radiological Research
Center, Obninsk, Russia5Department of Combined Therapy, Regional Tashkent Oncology Clinic
6Radiopreparat Government's Enterprise, Tashkent, Uzbekistan
ORIGINAL ARTICLE
*Correspondence
Dr Nigora RasulovaDepartment of Nuclear MedicineRepublic Specialized Center of Surgery10 Farkhadskaya StreetTashkent 1000115, UzbekistanEmail: [email protected]
Abstract
Aims The purpose of this study was toinvestigate a possible role of serum LDH as apredictor of cancer cell activity and todetermine if serum LDH levels canprognosticate the duration of pain-free periodafter radionuclide therapy.
Methods The We selected 62 breast cancerpatients with ages ranging from 29-67 years
(mean age 53.2±9.5 years) who had asuccessful response to radionuclide therapywith 153Sm-oxabifore and had their serum LDHlevels determined prior to the therapy.Patients with a history of a benign disease,which could possibly influence the serum LDHlevels, or those suffering from complicationssuch as a vertebral fracture or impending cordcompression, were excluded from the study.
153Sm-oxabifore was administrated in astandard dose of 37 MBq per kg body weight.All patients were on bisphosphonate therapy,both before and after samarium-153treatment. Group 1 comprised of 23 patientswho had received combined 153Sm-oxabiforeand zoledronic acid therapy. Group 2comprised of 39 patients who had additionallyreceived therapy for their primary tumour. For
PJNM 2016, 6:11-18 331691 © 2016 Pakistan Society of Nuclear Medicine
www.pjnm.net 2221-0288(201601/01)6:11<01:LDPFPF>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 12
each of these two groups, the correlationbetween serum LDH levels and duration of thepain-free syndrome was estimated.
Results There was a strong negativecorrelation (r = -0.84) between the serum LDHlevels and the duration of pain-free period inGroup 1, but no significant correlation (r = 0.1)was seen between the LDH levels and theduration of pain-free period in Group 2. Theduration of pain-free period in the secondgroup was longer in comparison to the firstgroup and was statistically significant(p<0.0001).
Conclusion Serum LDH level canprognosticate the duration of the pain-freeperiod after radionuclide therapy and could beuseful in selecting patients who in addition tosamarium-153 therapy may additionallybenefit from treatment of the primary tumour.
Key words: Lactate dehydrogenase (LDH),breast cancer, bone metastasis, zoledronicacid, radionuclide therapy
Introduction
Breast cancer has a propensity towardsskeletal metastases, leading to osteolysis andabnormal new bone formation. Within the first2 years of diagnosis, 10 - 15 % of patients mayhave distant metastases, 27.9% of which arebone secondaries. [1] Bone pain is a commonand significant cause of morbidity affecting60-90% of terminal patients of breast cancer.[2]
Bisphosphonates and radionuclide therapy arethe both widely used for the treatment ofpainful bone metastatic disease. Whilebisphosphonates are indicated for preventionof skeletal-related events, radionuclide therapywith bone seeking radiopharma ceuticals like153Sm-EDTMP (ethylenediaminetetramethylenephosphonic acid), Sr-89, etc.,have affinity for skeletal tissue, and, afterintravenously administration, concentrate inactive bone turnover, mostly in metastaticlesions, allowing site-directed radiotherapy for
painful bone secondaries. Combination of bothtreatments is more effective as compared toeither one in isolation [3-5].
In our earlier studies, we have demonstratedthat combined therapy of bone metastases byzoledronic acid together with radionuclidetherapy by 153Sm-oxabifore, was an effectivetherapeutic approach with statisticallysignificant reduction of the pain syndrome;however, the duration of pain-free syndromewas different in different patients [6].
It is known that most cancer cells have analtered metabolism involving a shift to aerobicglycolysis with lactate production coupled witha higher uptake of glucose as the main sourceof energy. Lactate dehydrogenase-5 (LDH-5)catalyzes the reduction of pyruvate bynicotinamide adenine dinucleotide hydrate(NADH) to maintain the continuity ofglycolysis, being an important control point inthe system of cellular energy release [7].Inhibition of LDH-A has demonstrated markedchanges in metabolic processes and overallsurvival in carcinoma cells [8-9]. LDH has alsobeen included in prognostic scores for severaltypes of cancer [10]. However, the value ofLDH as prognostic impact factor is unclear[11-13].
Progression of the primary tumour may leadto progression of the bone metastases anddevelopment of new bone secondaries, whichwill lead to reappearance of the painsyndrome. Recurrent pain or new sites of pain,often are the first indications of cancerprogression and should be promptly evaluated.
The objective of our study was to estimate ifserum LDH level can play a role as a predictorof cancer cell activity and proliferation of theprimary tumour, and also to evaluate its valuein predicting pain-free duration afterradionuclide therapy.
Patients & Methods
Patients
As 300 patients received radionuclide therapy
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:11-18

PJNM 2016, Volume 6, Number 1 13
for the pain syndrome from November 2009to July 2013 and were followed-up till July2015. We selected 62 breast cancer patientsaccording to the inclusion criteria: 1) patientswith known serum LDH level before combined153Sm-oxabifore and bisphosphonate therapy,2) without any non-cancer diseases whichcould influence the LDH level, 3) withoutcomplications such as vertebral fractures orof impending cord compression, and 4) withcomplete or almost complete response totherapy and being on follow-up withdocumented duration of pain-free period afterradionuclide treatment.
The patients were divided into two groups:Group 1 (n=23) included patients who hadreceived treatment of bone metastases byzoledronic acid and 153Sm-153 oxabifore ;Group 2 (n=39) included patients who hadreceived radionuclide and bisphosphonatetherapies together with the treatment of theprimary tumour according to individualsituation.
153Sm-oxabifore and bisphosphonate therapy
Inclusion criteria for radionuclide therapywere: 1) intense uptake in projection of painfulbone metastases on recent (2-4 weeks priorto therapy) 99mTc-methylene diphosphonate(MDP) whole-body (WB) bone scan; 2)satisfactory routine haematology(haemoglobin level >90 g/L; white blood cellcount >4x109/L; platelet count of >100x109/L); and 3) sufficient renal functionaccording to Cockroft and Gault formula -creatinine clearance >50ml/min.
Prior to the administration of the radio-pharmaceutical, the patients received verbalas well as written instructions and informationabout the procedure. This included: a) anexplanation of the therapeutic procedure andradiation protection guidelines; b) estimatedtime when to expect possible pain relief; c) awarning that a transient flare effect of painmay occur; and d) a note on general radiationprotection guidelines.
153Sm-oxabifore was administered to allpatients at the standard bone palliation doseof 37 MBq/kg body weight. Whole-bodypost-treatment scans were obtained within3-6 hours after 153Sm-oxabifore administration.
All patients received zoledronic acid before(2-6 months) and after (whole period offollow-up) treatment as per protocol in thestandard dosage, 4 mg every 28 days undercontrol of serum urea and creatinine levels.The period of time between theadministrations of zoledronic acid and153Sm-oxabifore was approximately ±2-7 days.
Pain assessment was based on visual analogscale (VAS), with 0 representing no pain and9 representing intolerable pain. The timeperiod between the occurrence of pain relief(when the patient stopped receivinganalgesics) and the onset of pain syndromerecurrence was monitored and recorded bythe local oncologists.
Statistical analysis
The results are expressed as the mean ± SEMfor each index. Comparison of data amongvarious groups was performed with Student’sunpaired t-test. P <0.05 was consideredstatistically significant. For calculatingcorrelation between the LDH level and theduration of pain-free period, the Spearman’srank correlation coefficient and simple linearregression for building the curves were used.
Results
The patient,s ages ranged from 29-67 years(mean age 53.2±9.5 years). Initial therapyfor all patients included mastectomy,chemotherapy, radiotherapy and hormonaltherapy (where receptor status was positive).See Table 1.
Time to developing bone metastases wasbetween 2-7 years after initial treatment.Bisphosphonate and radionuclide therapy wasgiven to all the patients; however, the second
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:11-18

PJNM 2016, Volume 6, Number 1 14
additionally received therapy for the primarytumour. Between the patient’s groups (Table2) there was no statistically significantdifference in T or N stages, visual assessmentscores (before and after therapies) and LDHlevels. However, the pain-free period wasalmost twice as long in the second comparedto the first group.
We found a strong negative correlation (R=-0.84) between the LDH levels and theduration of the pain-free period in the firstgroup of patients (Figure 1a) but there was
no correlation (R=0.1) between the LDH levelsand the duration of the pain-free period in thesecond group (Figure 1b).
21 out of 39 patients in the second grouprestarted to receive hormonal therapy afterdeveloping bone secondaries. On follow-upscans, one patient from the first group hadsignificant progression of bone metastases inthe left sacroiliac area and thoracic vertebrae5 months after radionuclide therapy (Figure2). Figure 3 shows a patient from the secondgroup, who received chemotherapy and
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:11-18
Table 1 Treatment characteristics of the patients
Table 2 Patients' characteristics and results
Initial therapy Group 1 Group 2
Mastectomy + +Chemotherapy + +Radiotherapy + +Hormonal therapy ±*(6/23) ±* (21/39)
Time to developing bone metastases 0.87-7.8 years(3.09±1.75)
1.6-10.8 years(4.8±2.5)
Bisphosphonates + +Radionuclide therapy by 153Sm-oxabifore + +Chemotherapy - +Hormonal therapy - ±*(21/39)
Group 1 Group 2 p
LDH level in IU/L 631.7±213.7 (284-918) 566.2±183.6 (244-985) 0.2
T 2.6±1 (1-4) 2.46±0.78 (2-4) 0.31
N 1,47±0.5 (1-2) 1.25±0.84 (0-3) 0.26
VAS pre therapy 7.56±1.34 (5-9) 7.87±1.32 (5-9) 0.38
VAS post therapy 1.04±0.82 (0-2) 0.85±0.75 (0-2) 0.33
Pain-free period(months)post 153Smtherapy
10.6±9.06 (3-36)CI-95%±3.68(6.9-14.3)
25.5±13.04 (5-57.9)CI-95%±4.09(21.41- 29.5)
0.00001
VAS- visual assessment score

PJNM 2016, Volume 6, Number 1 15
restarted hormonal treatment, has someprogression of bone metastases (together withsigns of regression) 36 months afterradionuclide therapy.
Discussion
The synergetic and simultaneous influence onbone metastases of medications like the last
generation of bisphosphonates (Zoledronicacid) and radionuclide therapy, can bebeneficial in treatment of the bone pain,especially in the earlier stage, beforedevelopment of complications such as avertebrae fracture or impending cordcompression. Moreover, some authors reportthat Zoledronic acid may have some anti-tumour effect on disseminated tumor cells [15].
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:11-18
a bFigure 1 Correlation between LDH level and the duration of the pain-free period after153Sm-oxabifore therapy: (a) in Group 1 and (b) in Group 2
Figure 2 Example whole-body bone scanof a patient from Group 1 (57-year-oldfemale 4.5 years after mastectomy for T2N1adeno- carcinoma; LDH level before 153Sm-oxabifore therapy 800IU/L; pain-free periodafter 153Sm-oxabifore plus bisphosphonatetherapy 5 months) showing progression ofmetastatic disease
Figure 3 Example whole-body bone scanof a patient from Group 2 (55-year-oldfemale 5 years after mastectomy for T2N1adenocarcinoma; LDH level before 153Sm-oxabifore therapy 886 IU/L; pain-free periodafter combined 153Sm-oxabifore plusbisphosphonate plus chemotherapy at >36months) showing regression

PJNM 2016, Volume 6, Number 1 16
Possible mechanism of pain relief usingradionuclide therapy was described byKairemo et al. [16] suggesting that βparticlesmay irradiate the red bone marrow (cancercells), and specific populations of nerve fibersthat innervate skeleton; both thesemechanisms may lead to disruption of the“vicious circle” [17-18] with possibletermination of VEGF production andproduction of growth factors.
According to Warburg's observation, cancercells have a high consumption of glucose andproduce large amounts of lactate [19]. LDHplays an important role in the final step ofaerobic glycolysis by converting pyruvate tolactate, which is coupled with oxidation ofNADH to NAD+ and allows maintaining thecontinuity of glycolysis [20]. Glycolysis is themain route of energy production with a minoruse of oxidative phosphorylation.
In a meta-analysis conducted by Zhang et al.[21], high LDH level was associated with poorprognosis, suggesting that LDH may be auseful biomarker for therapeutic selection ofhigh-risk patients who would need a intensivetherapy. Elevated LDH level is thought toreflect tumour aggressiveness and hightumour burden. Dynamic measurement of LDHlevel could be a useful tool in outcomeprognosis after therapy.
In our study, the patients who receivedcombined treatment with bisphosphonatesand radionuclide therapy only, the progressionof bone metastasis and recurrence of the painsyndrome were faster in comparison to thegroup of patients who additionally receivedchemotherapy and hormonal therapy. Thisdifference was presumably due to the fact thatonly 26% of the patients in the first group hadresponded to hormonal therapy versus 53%in the second group.
Our study demonstrates that there is strongnegative correlation between LDH level andduration of the pain-free period afterradionuclide therapy and no correlation ingroup of patients whom therapy of primarytumour was added. Since LDH levels reflects
cancer progression, according to our data,patients even with high LDH level• whoreceived treatment for their primary tumour,had longer pain-free periods• and reduction inbone metastases as documented on the WBbone scans. This underscores the importanceof the elevated LDH levels prognosticating theneed for more intensive treatment of theprimary tumour.
The two limitations of our study are the studysample heterogeneity and the small numberof patients in our study. In the first group ofpatients, initially 74% had no favourableprognosis since they were triple negativeversus 46.3% in the second group. Initialstage for developing metastases also couldplay a role. Further investigation on a largerand more heterogeneous group is needed.
Conclusion
Based on the results of this study of breastcancer patients, serum LDH levels canprognosticate the duration of the pain-freeperiod after radionuclide therapy. Further, asevidenced by the significantly longer pain-freeperiod in Group 2, it appears that serum LDHlevels could be useful in selecting patients whomay need treatment for their primary tumourin addition to samarium-153 therapy.
References
1. Mendoza ESR, Moreno E, Caguioa PB. JCancer Res Clin Oncol. 2013;139(4):645-52.
2. Mercadante S. Malignant bone pain:Pathophysiology and treatment. Pain.1997;69:1-19.
3. Storto G, Klain M, Paone G, Liuzzi R, MolinoL, Marinelli A, et al. Combined therapy ofSr-89 and zoledronic acid in patients withpainful bone metastases. Bone2006;39:35-41.
4. Koutsikos J, Leondi A. Treatment efficacyof combined bisphosphonates and 186Re-
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:11-18

PJNM 2016, Volume 6, Number 1 17
HEDP treatment in cancer patients withbone metastases. Eur J Nucl Med MolImaging 2008;35:1392-3.
5 Lam MG, Dahmane A, Stevens WH, vanRijk PP, de Klerk JM,Zonnenberg BA.Combined use of zoledronic acid and153Sm-EDTMP in hormone-refractoryprostate cancer patients with bonemetastases. Eur J Nucl Med Mol Imaging2008;35:1392-3.
6 Nigora Rasulova, Vladimir Lyubshin,Dauranbek Arybzhanov, Sh. Sagdullaev,Valery Krylov,Marat Khodjibekov. Optimaltiming of bisphosphonate administrationin combination with samarium-153oxabifore in the treatment of painfulmetastatic bone disease. World J Nucl Med2013;12:14-18.
7 Augoff K, Hryniewicz-Jankowska A, TabolaR. Lactate dehydrogenase 5: an old friendand a new hope in the war on cancer.Cancer Lett. 2015;358(1):1-7.
8 Granchi C, Roy S, Giacomelli C, MacchiaM, Tuccinardi T, Martinelli A, et al.Discovery of N-hydroxyindole-basedinhibitors of human lactate dehydrogenaseisoform A (LDH-A) as starvation agentsagainst cancer cells. J Med Chem.2011;54(6):1599-612.
9 Granchi C, Calvaresi EC, Tuccinardi T,Paterni I, Macchia M, Martinelli A,Hergenrother PJ, Minutoloa F. Assessingthe differential action on cancer cells ofLDH-A inhibitors based on the N-hydroxyindole-2-carboxylate (NHI) andmalonic (Mal) scaffolds. Org Biomol Chem.2013 Oct 14;11(38):6588-96.
10 International Prognostic Factors StudyGroup, Lorch A, Beyer J, Bascoul-MolleviC, Kramar A, Einhorn LH, Necchi A,Massard C, De Giorgi U, Fléchon A,Margolin KA, Lotz JP, Germa Lluch JR,Powles T, Kollmannsberger CK.Collaborators (107) Prognostic factors inpatients with metastatic germ cell tumorswho experienced treatment failure withcisplatin-based first-line chemotherapy. JClin Oncol 2010;28:4906-4911.
11. Kamiya N , Suzuki H , Ueda T , Sato N ,Nakatsu H , Mikami K , Sato N , NomuraK , Akakura K , Okano T , Ooki T , NayaY , Ota S , Masai M , Ichikawa T. Clinicaloutcomes by relative docetaxel dose anddose intensity as chemotherapy forJapanese patients with castration-resistant prostate cancer: a retrospectivemulti-institutional collaborative study.Int J Clin Oncol 2014;19:157-164.
12. He WZ, Guo GF, Yin CX, Jiang C, WangF, Qiu HJ, Chen XX, Rong RM, Zhang B,Xia LP. Gamma-glutamyl transpeptidaselevel is a novel adverse prognosticindicator in human metastatic colorectalcancer. Colorectal Dis 2013;15: e443-e452.
13. Sau, S., Biswas, A., Roy, A., Sau, S. &Ganguly, S. Retrospective analysis of theclinical and demographic variables on theoutcomes after second-line treatment inadvanced non-small cell lung cancer.Indian J Med Paediatr Oncol 2013;34:274-279.
14. Xu HN, Kadlececk S, Profka H, GlicksonJD, Rizi R, Li LZ (2014). "Is HigherLactate an Indicator of Tumor MetastaticRisk? A Pilot MRS Study UsingHyperpolarized (13)C-Pyruvate."2013.Acad Radiol 21 (2): 223-31doi:10.1016/j.acra.2013.11.014. PMID24439336.
15. Banys M, Erich-Franz S, Gebauer G, JanniW, Krawczyk N, Hans-Joachim L, BeckerS, Huober J, Kraemer B, Wackwitz B, etal. Influence of zoledronic acid ondisseminated tumor cell in bone marrowand survival" results of prospectiveclinical trial. BMC Cancer 2013;13:480.
16. Kairemo K et al. "Radionuclide Treatmentwith 153Sm-EDTMP is Effective for thePalliation of Bone Pain in the Context ofExtensive Bone Marrow Metastases: ACase Report. Asia Oceania J Nucl MedBiol. 2014;2(2):131-134.
17. Roodman GD." Mechanisms of bonemetastasis". 2004. N Engl J Med. 35:1655-64. ceptor kinase A". 2011.Neuroscience. 178: 196-207.
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:11-18

PJNM 2016, Volume 6, Number 1 18
18. Castañeda-Corral G, Jimenez-AndradeJM, Bloom AP, Taylor RN, Mantyh WG,Kaczmarska MJ. et al. The majority ofmyelinated and unmyelinated sensorynerve fibers that innervate bone expressthe tropomyosin receptor kinase A.Neuroscience 2011.;178:196-207.
19. Hsu, PP, Sabatini DM. Cancer cellmetabolism: Warburg and beyond. Cell2008;134:703-707.
20. Serganova I, Rizwan A, Ni X, Thakur SB,Vider J, Russell J, Blasberg R, KoutcherJA. Metabolic imaging: a link betweenlactate dehydrogenase A, lactate, andtumor phenotype. Clin Cancer Res2011.;17:6250-6261.
21. Zhang J, Yao YH, Li BG, Yang Q, ZhangPY, Wang HT. Prognostic value ofpretreatment serum lactatedehydrogenase level in patients withsolid tumors: a systematic review andmeta-analysis. Sci Rep. 2015;22(5):9800.
Pak J Nucl Med 2016;6:11-18 2221-0288(201601/01)6:11<01:LDPFPF>2.0.TX;2-M

Assessment of renal parenchymal damage byDMSA after PCNL procedure in children using
adult-sized equipment
Mohammad Sohaib1,*,Manoj U Shenoy2,Michael J Kellett3, Patrick G Duffy3, Isky Gordon4
1Department of Medical Sciences, Pakistan Institute of Engineeringand Applied Sciences (PIEAS), Nilore, Islamabad, Pakistan.
2Department of Paediatric Urology, NottinghamUniversity Hospitals NHS Trust, Nottingham,UK.
3Department of Urology, Great Ormond Street Hospital,NHS Trust,London, UK.
4Department of Radiology, UCL Institute of Child Health, London, UK.
ORIGINAL ARTICLE
*Correspondence
Muhammad Sohaib Department of Medical Sciences, Pakistan Institute of Engineering & Applied Sciences (PIEAS PO Nilore, Islamabad-45650, Pakistan. Tel: +92 51 2208361 Fax: +92 51 2208070 Email: [email protected]
Abstract
Aims Percutaneous nephrolithotomy (PCNL)is an established technique for the manage-ment of renal calculi. The recent advances inthis procedure in children include miniaturizingthe endoscopic instruments used for renalaccess. However, there is limited data on thefunctional effects of PCNL on the renalparenchyma, performed using adult-sizedequipment in the paediatric population. Thisstudy was therefore aimed to determine theeffects of PCNL on the renal parenchyma inchildren with renal calculi using technetium-99mlabelled dimercaptosuccininc acid (99mTc-DMSA)
scans.
Methods Pre and post-surgery DMSA scansof 26 paediatric patients who had undergonePCNL over a five-year period were reviewed.The ages of the patients ranged from 1 yearto 12.5 years (median: 3.75 years) at the timeof PCNL. The procedures were done with 18Fr or higher sized Amplatz sheath. DMSA scanswas performed from 1 day to 47 monthsbefore the PCNL and 2 months to 27 monthsafter the procedure and interpreted by twoindependent observers. Regions-of-interestaround each kidney were drawn to determinedifferential renal function (DRF) of the kidneys.
Results Twenty patients (77 %) showed nochange or showed improvement in post-procedure scans. Mean±SD DRF was44.1±9.7% before and 44.6±10.6% after theprocedure (p=0.52, n=21).
Conclusion We conclude that the PCNLprocedure in children undertaken with adult-sized equipment may show renal defects innearly one-fourth of children but there is nosignificant change in their global renal function.
PJNM 2016, 6:19-24 331691 © 2016 Pakistan Society of Nuclear Medicine
www.pjnm.net 2221-0288(201601/01)6:1<19:ARPDDP>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 20
Key words: Percutaneous nephrolithotomy;99mTc-DMSA; children; adult-sized equipment
Introduction
Open surgery for the management of upperurinary tract calculi has been largely replacedby percutaneous nephrolithotomy (PCNL) orextracorporeal shock wave lithotripsy (ESWL).PCNL is a surgical procedure in which renalcalculi are removed through a one centimeterskin puncture. A track down to the kidney isestablished under x-ray guidance and anephroscope is passed into the kidney. Smallstones are removed directly and the largerones are broken into small pieces with anultrasonic or electrohydraulic probe, or aholmium laser lithotripter. ESWL due to itslower morbidity is the procedure of choice butPCNL is preferred for calculi more than 2 cmin diameter. In children, the latter isperformed cautiously due to the concerns ofdamage to renal parenchyma when it ispierced by nephroscope. PCNL was firstperformed in paediatric patient in 1985 andwith the advances in the technique thefrequency has significantly increased sincethen [1-3]. Nephroscopes of sizes rangingfrom 19.5 to 27-Fr were used initially while17-Fr was introduced in late 1980s [2].Today, 15-Fr nephroscopes are easilyavailable. Smaller nephroscopes maytheoretically cause lesser damage to therenal parenchyma; however, their benefitin children is yet to be established. Traxeret al. reported no significant difference inscar tissue measured in sacrificed pigs withright kidney nephrostomies by 30-FrAmplatz sheath than left kidneys puncturedwith 11-Fr sheaths [4]. The growing child'skidney may be affected more by the PCNLsize than full-grown kidneys. Althoughseveral studies have reported that theadult-sized PCNL equipment is safe inchildren [5-8], other researchers incontrast, have reported significantcomplications [9-11]. The assessment ofsafety of the procedure in all these studieswas undertaken by measuring parameterslike stone-free rates and the need for blood
transfusions. Scanning with technetium-99mlabelled dimercaptosuccininc acid (99mTc-DMSA) is a practical option for the assessmentof renal parenchymal damage before and afterthe procedure. Identifying new photon-deficient areas or significant reduction indifferential renal function of the operated side,indicates renal parenchymal damage. Wevisually and quantitatively compared pre- andpost-PCNL 99mTc-DMSA scans of paediatricpopulation who had procedures performedwith adult-sized PCNL tracts.
Materials and Methods
Medical records of four consecutive years ofUrology and Nuclear Medicine departments atGreat Ormond Street Hospital, London, UK,were examined retrospectively from 1999 to2003, and 37 patients who had undergone PCNLwith ≥18-Fr Amplatz sheath were selected.Patients who had either preoperative withpostoperative, or a normal postoperative DMSAscan were included. Eleven patients wereexcluded due to lack of adequate details ofimaging. Twenty-six patients with ages rangingfrom 1 to 12.5 years (median: 3.75 years) weretherefore available for the review. Twenty-onepatients had both pre- and post-procedure scanavailable, while 5 patients had only post-procedure scans, which were normal. 62%patients had calculi in the left kidney.
The PCNL tracts were established and thestones were disintegrated with ultrasonic probeand removed. The size of the Amplatz sheathused varied from 18-Fr to 28-Fr (median:24-Fr). After the PCNL a nephrostomy tube wasplaced (range 6-Fr to 28-Fr; median 24-Fr) in22 patients; 4 patients did not have a tubeplaced after the procedure. Thirty-threepunctures were attempted, with 7 kidneysperforated both in the upper and the lowerpoles. Five perforations were made in upperpoles only, 6 in lower only and 8 in the mid-portion of the kidneys. In those cases whereboth the poles were punctured, Amplatzsheaths of the same size were used except inone case in which upper pole was perforatedwith a 26-Fr and the lower with a 24-Fr sheath.
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:19-24

PJNM 2016, Volume 6, Number 1 21
DMSA scans were performed from 1 day to 47months (median = 2 months) before the PCNLand 2 months to 27 months (median = 3.5months) after the procedure. The child wasinjected using an intravenous line, with amaximum of 80 MBq of 99mTc-DMSA andscintigraphy was started 2-4 hours after theinjection. Images were acquired on one of twosingle-headed gamma cameras fixed withhigh-resolution parallel-hole collimators.Posterior and both posterior-oblique, i.e.left-posterior-oblique (LPO) and right-posterior-oblique (RPO) projections wererecorded for 250-500 k-counts on digitalmatrix of 256×256.
Visually, DMSA scans were interpreted for anyabnormality by two independent observers.The decision on any disagreement ininterpretation was established after mutualconsensus. The scans were also assessedsemi-quantitatively by measuring differentialrenal functions (DRF) of the two kidneys andcompared where both pre- and post-PCNLscans were available. Student's t test wasapplied for this comparison and p-value lessthan 0.05 was considered significant.
Results
Table 1 shows the patients grouped on thebasis of visual interpretation and comparisonsof pre-procedure and post procedure DMSAscans. Twenty patients (77%) had eithernormal post-procedure scans (n=12, 46%)or had no change in pre-procedure abnormalscans (n=8, 31%). In those with normalpost-procedure scans, the pre-PCNL scanswere normal in five, abnormal in two and notavailable in five patients. Remaining 23%(n=6) patients showed new areas of uptakedefects in previously normal or abnormal331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:19-24
Pre procedure scan Post procedure scan No. of patients OutcomeNormal Normal 5 Favourable
n=20No scan available Normal 5Abnormal Normal 2Abnormal No change from previous 8Normal Abnormal 3 Deteriorated
n=6Abnormal Abnormal with new defects 3*
Table 1 The visual interpretations of DMSA scans
Figure 1 99mTc-DMSA scans comparing preand post PCNL images. (A) normal; (B) uptakedefect in pre-procedure (arrow) and normalpost-procedure; (C) same defect (arrow) in preand post procedure; (D) normal pre-procedureand new defect (arrow) in post-procedure; (E)persistent defect in pre-procedure (arrow) anda new defect in post-procedure (arrowhead)

PJNM 2016, Volume 6, Number 1 22
scans. Images of selected case are shown inFigure 1.
Pre-procedure scans had 44.1±9.7% DRFwhich after the procedure was 44.6±10.6%(p=0.52, n=21). DRF of the cases havingfavourable outcome on visual analysis was43.5±11.3% before and 44.3±12.1% afterthe procedure (p=0.83, n=15). Those casesshowing deterioration of DMSA scans on visualanalysis had DRF 45.7±3.7% before and
44.7±5.0% after PCNL (p=0.54, n=6). Figures2 and 3 demonstrate these changesindividually.
Discussion
The pros and cons of PercutaneousNephrolithotripsy (PCNL) versus Extra-corporeal Shockwave Lithotripsy (ESWL) haveoften been highlighted when one discusses themanagement of renal stones. ESWL has an
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:19-24
Figure 2 (A) Values of differential renal function (DRF) in pre- and post-PCNL scans in patientsthat showed favourable outcome after surgery on visual analysis with the dotted line representingsame data seen in two different patients; (B) difference in DRF between the two scans
Figure 3 (A) Values of differential renal function (DRF) in pre- and post-PCNL scans in patientsthat showed deterioration after surgery on visual analysis; (B) difference in DRF between the twoscans

PJNM 2016, Volume 6, Number 1 23
advantage over PCNL of not requiring generalanaesthesia. However, this advantage doesnot exist in case of children. There arecontroversial reports published regarding thesafety of renal parenchyma during ESWL inadults as well as children [12, 13]. In case ofPCNL, there is limited data available regardingthe direct assessment of renal parenchymaldamage caused when adult-sizednephroscopes are used.
99mTc-DMSA is an effective and reproduciblemethod for evaluating regional and globalrenal function [14, 15]. It has been used forassessing damage to the renal parenchymathat may follow the PCNL procedure [16-18].Regional assessments on 99mTc-DMSA scansare usually performed by identifying thephoton-deficient areas in the renalparenchyma. Global function may be assessedby visual analysis as well as quantitativeanalysis by measuring differential renalfunction [19-21].
After evaluation of our study data, it wasfound that 5 patients had normal scans beforeand after the procedure; 5 patients had onlyone normal post procedure study available; 2patients showed improvement and 8 hadabnormal pre-procedure scans with no changeseen on the post- procedure scans. All of these20 (77%) cases had a favourable outcome inrenal function after PCNL. The other groupconsisted of 3 patients with normal pre-procedure scans and photon-deficient areasin scans done after the procedure and 3patients with previously abnormal scan anddeterioration seen visually in the renal scansafter PCNL. In our study 23% of the patientsshowed new or additional regions of absentuptake of DMSA. This is in contrast to Samadet al. who demonstrated only 5% [22], buttheir data was based on only four children whohad a pre-procedure scans available. Incontrast, our study was designed to comparepre- and post-procedure scans. Pre-procedurescans were not available in our study onlywhere they were not required, i.e., normalpost-procedure scans. Moreover, Samad et al.used 17-Fr nephroscopes in 75% of their
population while we used Amplatz sheaths ofmore than 18-Fr in all our patients. To ourknowledge there is no study that comparespre- and post-PCNL DMSA scans in childrenwhere adult sized equipment has been used.Many studies have evaluated the use of suchequipment in children by assessing the stone-free rates and complications like the need forblood transfusions, but the reported resultsare conflicting [5-11].
DRF of both pre and post studies wereavailable in 19 patients. There was nosignificant change seen in DFR in the operatedkidneys before and after the procedure. Therewas a slight increase in DRF in patients whoshowed favourable changes visually but wasnot statistically significant (p=0.83). Similarly,the DRF decrease in the patients showingdeterioration visually was also not significant.In a study performed in an adult population,Demirtas et al. found significant differences indifferential functions before and after PCNL[23]. The possible reason is the growingkidneys in children. This may causecompensatory change in overall renal functiondespite the fact that the scars may persistregionally.
Conclusion
The study demonstrated that PCNL procedurewith adult-sized equipment may causeregional uptake defects on the DMSA scan innearly one-fourth of children without asignificant change in global differentialfunction.
References
1. Woodside JR, Stevens GF, Stark GL, BordenTA, Ball WS. Percutaneous stone removal inchildren. J Urol. 1985;134(6):1166-1167.
2. Zattoni J, Passerini-Glanzel G, Tasca A,Artibani W, Pagano F. Pediatric nephroscopefor percutaneous renal stone removal. Urol.1989;33(5):404-406.
3. Landau EH. Modern Stone Management inChildren. Eur Urol Suppl. 2015;14(1):12-19.
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:19-24

PJNM 2016, Volume 6, Number 1 24
4. Traxer O, Smith TG III, Pearle MS, Corwin TS,Saboorian H, Cadeddu JA. Renal parenchymalinjury after standard and mini percutaneousnephrostolithotomy. Invest Urol.2001;165(5):1693-1695.
5. Etemadian M, Maghsoudi R, Shadpour P,Mokhtari MR, Rezaeimehr B, Shati M. PediatricPercutaneous Nephrolithotomy Using AdultSized Instruments. Urol J. 2012;9(2):465-471.
6. Nouralizadeh A, Basiri A, JavaherforooshzadehA, Soltani MH, Tajali F. Experience ofpercutaneous nephrolithotomy using adult-sizeinstruments in children less than 5 years old. JPediatr Urol. 2009;5(5):351-354.
7. Dogan B, Atmaca AF, Canda AE, Isgoren AE,Akbulut Z, Balbay MD. Efficiency of percutaneousnephrolithotomy in pediatric patients usingadult-type instruments. Urol Res.2012;40(3):259-262.
8. Aron M, Yadav R, Goel R, Hemal AK, Gupta NP.Percutaneous nephrolithotomy for completestaghorn calculi in preschool children. J Endourol.2005;19(8):968-972.
9. Zeren S, Satar N, Bayazit Y, Bayazit AK, PayasliK, Ozkeçeli R. Percutaneous nephrolithotomy inthe management of pediatric renal calculi. J.Endourol. 2004;16(2):75-78.
10. Gunes A, Yahya Ugras M, Yilmaz U, Baydinc C,Soylu A. Percutaneous nephrolithotomyforpediatric stone disease--our experience withadultsized equipment. Scand J Urol Nephrol.2009 Jul 9;37:477-481.
11. Desai M. Endoscopic management of stones inchildren. Curr Opin Urol. 2005;15(2):107-112.
12. Lottmann HB, Archambaud F, Traxer O, Mercier-Pageyral B, Helal B. The efficacy andparenchymal consequences of extracorporealshock wave lithotripsy in infants. Brit J Urol Int.2000;85(3):311-315.
13. Lottmann HB, Traxer O, Archambaud F, Mercier-Pageyral B. Monotherapy extracorporeal shockwave lithotripsy for the treatment of staghorncalculi in children. J Urol. 2001;165(6):2324-2327.
14. Camacho V, Estorch M, Fraga G, Mena E, FuertesJ, Hernandez MA, Flotats A, Carrio I. DMSA study
performed during febrile urinary tract infection:a predictor of patient outcome? Eur J Nucl MedMol Imaging. 2004;31(6):862-866.
15. Caione P, Ciofetta G, Collura G, Morano S,Capozza N. Renal damage in vesico-uretericreflux. Brit J Urol Int. 2004;93(4):591-595.
16. Brodiea KE, Lanea VA, Leeb TWJ, Robertsa JP,Raghavanc A, Hughesc D. et al. Outcomesfollowing 'mini' percutaneous nephrolithotomyfor renal calculi in children. A single-centre study.J Pediatr Urol. 2015;11(3): 120.e1-120.e5.
17. Vig M, Vig V, Nagi GS, Suchak S, Goyal S.Percutaneous Nephrolithotomy in TheManagement of Pediatric Renal Calculi. PARIPEX- Indian J Res. 2016;5(4):331-333.
18. Matsuura H, Hioki T, Sakurai M, Arima K,Yanagawa M, Sugimura Y, Tochigi H, KawamuraJ, Kinoshita N, Katoh H. Influence ofextracorporeal shock wave lithotripsy (ESWL)on renal function assessed by 99mTc-DMSAscintigraphy: comparative analysis betweenESWL and percutaneous nephroureterolithotripsy (PNL). Hinyokika Kiyo.1994;40(12):1061-1067.
19. De Sadeleer C, Tondeur M, Melis K, Van EspenMB, Verelst J, Ham H, Piepsz A. A multicentertrial on interobserver reproducibility in reportingon 99mTc-DMSA planar scintigraphy: a Belgiansurvey. J. Nucl. Med. 2000;41(1):23-26.
20. Taylor A Jr. Quantitation of renal function withstatic imaging agents. Semin Nucl Med.1982;12(4):330-344.
21. De Sadeleer C, Bossuyt A, Goes E, Piepsz A.Renal technetium-99m-DMSA SPECT in normalvolunteers. J. Nucl. Med. 1996;37(8):1346-1349.
22. Samad L, Qureshi S, Zaidi Z. Does percutaneousnephrolithotomy in children cause significantrenal scarring? J Pediatr Urol. 2007;3(1):36-39.
23. Demirtas A, Caniklioglu M, Kula M, et al.Assessment of the Effects of access count inpercutaneous nephrolithotomy on renalfunctions by technetium-99m-dimercaptosuccinic acid scintigraphy. Urol. 2013;2013:5pages. doi:10.1155/2013/827121
Pak J Nucl Med 2016;6:19-24 2221-0288(201601/01)6:1<19:ARPDDP>2.0.TX;2-M

PJNM 2016; 6:25-31 331691 © 2016 Pakistan Society of Nuclear Medicine
Vitamin B12 deficiency: prevalence and evaluationof a reversible co-morbidity in hypothyroid patients
Aniqa Jabeen*, Sumaira Mushtaq,Hassan Raza, Mohammd Ali Memon
Department of Nuclear Medicine, Atomic Energy Medical Centre, JinnahPostgraduate Medical Centre (JPMC), Karachi
ORIGINAL ARTICLE
Abstract
Aims The study aimed at assessing theprevalence and clinical features of vitamin B12deficiency in hypothyroid patients and toevaluate clinical response to vitamin B12replacement therapy.
Methods A total of 204 vitamin B12 deficientpatients with primary hypothyroidism whoattended the thyroid clinic at the nuclearmedicine department of Atomic EnergyMedical Centre Karachi, were included in thestudy. Signs and symptoms, haemoglobin(Hb), mean corpuscular volume (MCV),thyroid function tests and B12 levels wererecorded. Patients with low levels of B12 orwho had symptoms suggestive of B12deficiency were given oral vitamin B12treatment and monitored for improvement.
Results A total of 204 hypothyroid patients(197 females, 7 males) were evaluated. 92of 204 patients (45.09%) had low vitamin B12levels. Depression (p value 0.000082),weakness (p value 0.0018), numbness (p
value 0.022), paraesthesia (p value 0.018),and impaired memory (p value 0.027) werestatistically significant in B12-deficienthypothyroid patients. B12-deficient patientshad increased prevalence of anaemia than thesufficient group (32.6% vs. 22.02%). 92B12-deficient and 70 B12-sufficient patientswith symptoms of B12 deficiency were startedon oral vitamin B12 and improvement noted.
Conclusion There is a high (45%) prevalenceof B12 deficiency in hypothyroid patients.Screening of vitamin B12 levels should beundertaken in all hypothyroid patients in theearly course of the disease as it is a potentiallyreversible condition. Weakness, numbnessand neuropsychiatric symptoms point towardsB12 deficiency. Replacement of B12 leads toimprovement in symptoms; however, placeboeffect should be taken into consideration.
Key words: Anaemia, hypothyroidism,neuropsychiatric symptoms, vitamin B12deficiency
Introduction
Vitamin B12 (cobalamin) is one of thecomplex water soluble vitamins. Severalcritical biological processes such as cellularmetabolism, DNA replication and red bloodcell formation depend on vitamin B12.Vitamin B12 deficiency occurs in about 3.8%of the population. Diverse religions, ethnic
*Correspondence
Dr Aniqa Jabeen Atomic Energy Medical Centre (AEMC) Jinnah Postgraduate Medical Centre Rafique Shaheed Road, Karachi Email: [email protected] Tel: +923323132040
www.pjnm.net 2221-0288(201601/01)6:1<25:VBDPAE>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 26
and socio-economic heterogeneity of the peopleof Asian countries leads to under recognition ofits deficiency [1].
Pernicious anaemia is present in subjects withprimary autoimmune hypothyroidism with areported association in up to 12% of patients[1]. Vitamin B12 deficiency may also be due tothe high prevalence of H. pylori infections [2],use of oral contraceptive pills [3], diabeticmedication like metformin [4], malnutrition andmalabsorption. In developing countries, thedeficiency is much more common starting inearly life with the prevalence increasing withage. Classic cobalamin deficiency is associatedwith megaloblastic anaemia and neurologicalsymptoms [8]. The typical haematologicchanges are easy to detect but they occur at alater stage and may even be absent [9].
Hypothyroid patients often present withweakness, fatigue, paraesthesia, numbness ortingling in the fingers and toes, poor balanceand coordination, depression, dementia, and adecline in mental abilities that is severe enoughto interfere with daily life, despite beingeuthyroid on adequate doses of thyroxine.
The increasing frequencies of these symptomsin hypothyroid patients led us to evaluate forthis co-morbid condition as it is a potentiallyreversible burden.
Materials and Methods
Patients with primary hypothyroidism whoattended the thyroid clinic at the nuclearmedicine department of Atomic Energy MedicalCentre Karachi, from October 2015 to march2016 were evaluated. Patients who were strictvegetarians, had history of gastric or ilealresection or malignancies were excluded.
Clinical features including weakness, numbness,abdominal pain, depression, impaired memory,paraesthesia and decreased reflexes were noted.The presence of pallor and impaired reflexes wasrecorded. A note of concomitant illnesses andmedications including gastric acid inhibitors andmetformin was made. Haemoglobin level, meancorpuscular volume, thyroid function tests,
thyroid antibodies and vitamin B12 levels weremeasured.
Patients who had low levels of vitamin B12 orwho had symptoms suggestive of vitamin B12deficiency, were given oral vitamin B12. Thepatients were followed for 6 months and a notewas made of any improvement in symptoms.
Haemoglobin was checked by spectrophoto-meter using cyanide-free technique with patientswith Hb levels of <11 mg/dl in females and <13mg/dl in males were considered as anaemic.Vitamin B12 levels were estimated by theradioimmunoassay technique by a gammacounter using the Diagnostic Product Cooperation(DPC) method, with the normal range of 200-900pg/ml.
Results were expressed as mean ± standarddeviation, median for all continuous variables andnumber (percentages) for categorical data.Statistical analysis was performed by chi-squaretest were appropriate and p value <0.5 wastaken as significant. Statistical interpretation ofdata was performed using SPSS 10.0.
Results
204 hypothyroid patients were evaluatedincluding 197 (96.5%) females and 7 (3%)males. The patients' age ranged from 14-80years with a mean age of 37.24 ± 11.61 (44.28± 16.93 for males and 36.99±11.35 forfemales); 117 (57.35%) patients were below 40years of age.
A total of 92 (45.09%) of 204 patients hadvitamin B12 levels <200 pg/ml (normal 200-900pg/ml); 75 of the 92 patients had levels between100-200 pg/ml, and 17 with levels <100 pg/ml.There was no significant difference in mean ageand sex ratios between the groups with vitaminB12 deficiency and those with normal vitaminB12 levels (Table 1).
Symptoms of depression, weakness, numbness,paraesthesia, impaired memory and hair losswere seen more commonly in vitamin B12-deficient patients. The frequencies of commonsymptoms recognized in our hypothyroidpatients are seen in Table 2. Twenty hypothyroid
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:25-31

PJNM 2016, Volume 6, Number 1 27
patients with vitamin B12 deficiency were seento have pallor. Impaired reflexes wererecorded in 15 of the hypothyroid vitaminB12-deficient patients.
Haemoglobin value was noted in all patients.The mean Hb in vitamin B12-deficient group
was slightly lower than in B12-sufficient group(10.61 ± 1.82 vs. 11.84±1.54). 5 (71%)males had Hb <13.5 while 53 females (57.6%)had Hb <11g/dl. B12-deficient patients hadincreased prevalence of anaemia comparedwith the non-deficient group (32.6% vs.22.02%).
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:25-31
B12 >200 pg/ml B12 <200 pg/ml
No. 112 92
Age 37.47±11.2 yrs 36.96±12.1 yrs
Sex male 1 male 6
female 111 female 86
Table 1 Mean age and sex demographics in vitamin B12-deficient and B12-sufficient groups
Table 2 Frequency of symptoms in B12-deficient and B12-sufficient patients
Symptoms Total patients (n= 204) B12<200 pg/ml B12>200 pg/ml
Depression 150 80 (53.3%) 70 (46.6%)
Weakness 144 75 (52.0%) 69 (47.9%)
Numbness 136 69 (50.7%) 67 (49.2%)
Paresthesia 99 53 (53.5%) 46 (46.4%)
Impaired memory 87 47 (54.0%) 40 (45.9%)
Hair loss 65 35 (53.8%) 30 (46.1%)
Nausea/vomiting 80 34 (37.5%) 46 (57.5%)
Retrosternal burning 57 22 (38.5%) 35 (61.4%)
Abdominal pain 31 15 (48.3%) 16 (51.6%)
Decreased reflexes 21 10 (47.6%) 11 (52.3%)
Shortness of breath 11 6 (54.5%) 5 (45.4%)
Palpitations 3 1 (33.3%) 2 (66.6%)

PJNM 2016, Volume 6, Number 1 28
Associated diseases among the 204 hypothyroidpatients included diabetes (n=15),hypertension (n=34), ischaemic heart disease(n=3) and dyslipidaemia (n=6). Six of the 15diabetic patients were vitamin B12-deficient but2 of them were taking metformin, which mayhave contributed to the vitamin B12 deficiency.Four out of 25 patients who were on protonpump inhibitors or H2 receptor blockers, werefound to be vitamin B12 deficient. Replacementtherapy with oral vitamin B12 was institutedand the patients were followed upsubsequently. Ninety-two vitamin B12-deficientand 70 vitamin B12-sufficient patients withsymptoms suggestive of vitamin B12 deficiencywere started with oral vitamin B12 replacementtherapy. Improvement in symptoms wasdocumented in 122 patients. 87 out of 92(94.5%) was B12-deficient while 35 out of 70(50%) were B12-sufficient. Forty patients didnot show any improvement in symptoms ofwhich 5/40 (12%) were B12-deficient and 35out of 40 (87.5%) were B12-sufficient.
Discussion
Vitamin B12 or cobalamin, is one of the Bcomplex water soluble micronutrient chieflyavailable in animal protein. Several criticalbiological processes such as cellularmetabolism, DNA replication, red blood cellformation depend on vitamin B12; furthermore,metabolism of B12 is essential for myelinsynthesis and maintenance of neuronal integrityas well as neurotransmitter regulation [10, 11].Our study estimated the prevalence of B12deficiency at 45.09% (92 of 204 patientshypothyroid patients), which is higher than the39.6% prevalence reported by Jabbar et al.[12].
Most people obtain sufficient vitamin B12 fromtheir diet. However, in the developingcountries, B12 deficiency is much morecommon, starting in early life, with an increasein prevalence with age in certain groups ofpeople, such as people of low socioeconomicstatus who rely more on a vegetarian diet andpeople older than 50 years of age. In thedeveloped countries 6% of those aged 60years and above are B12-deficient, with the
prevalence in elderly varying from 3-40%likely due to malabsorption [7].
Metformin can cause malabsorption secondaryto its effect on ileal mucosa. Proton pumpinhibitors and H2 receptor antagonist causegastric hypochlohydria and malabsorption ofvitamin B12. Pernicious anaemia inhypothyroid patients may be part of anautoimmune polyglandular endocrinopathy[13]. Intrinsic factor and gastric parietal cellantibody were not available locally andpatients were unable to get tests done due tosocioeconomic constraints; therefore, despiteassociation of hypothyroidism and vitamin B12deficiency, the underlying aetiology wasdifficult to determine.
Vitamin B12 deficiency causes haematological,neurologic, cognitive problems and moodsymptoms. Severe cobalamin deficiency isassociated with megaloblastic anaemia;however, it can occur without the classic signsof anaemia or macrocystosis. The typicalhaematologic changes associated with vitaminB12 deficiency are easy to detect but thesedevelop at a later stage and may even beabsent [9, 14].
In our study haemoglobin value was recordedin all patients. The mean Hb in vitaminB12-deficient group was slightly lower than inB12-sufficient group (10.61 ± 1.82 vs. 11.84± 1.54). 5 (71%) males had Hb <13.5 while53 (57.6%) females had Hb <11g/dl. B12-deficient hypothyroid patients had increasedprevalence of anaemia than the patients in thenon-deficient hypothyroid group (32.6% vs.22.02%). The MCV value was however thesame for both groups (80.79±9.8 vs.80.17±10.87). Unexpectedly, macrocytosiswas rare in the current study population, evenamong those with very low cobalaminconcentrations. One possible reason may bethat an adequacy of folate intake, whichprotects against macrocytosis and therebymasks the effect of cobalamin deficiency [8,15 ].
Hypothyroid and vitamin B12-deficientpatients have similar symptoms of weakness,lethargy, memory impairment and tingling.
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:25-31

PJNM 2016, Volume 6, Number 1 29
We noted that several patients, despite havingadequate thyroxine treatment, had persistenceof symptoms and these were later found to bevitamin B12-deficient. In our study, we notedthat weakness and numbness, although presentin both groups, was significantly higher in thevitamin B12-deficient hypothyroid patients,with p values at 0.0018 and 0.022 respectively.
Clinical signs of vitamin B12 deficiency maytake long to manifest; however, neuropsychiatric symptoms occasionally present asthe earliest clue to B12 deficiency. Vitamin B12deficiency in hypothyroid patients can be oneof the most important causes of reversiblecognitive decline acting as a second hit inhypothyroid patients. In our study, statisticallysignificant neuropsychiatric manifestations wereseen between the B12-deficient hypothyroidpatients and the B12-sufficient patients:including depression (p=0.000082),paraesthesia (p=0.018), and impaired memory(p=0.027). Other complaints like hair loss,nausea/vomiting, abdominal pain anddecreased reflexes were common in both setsof patients; however, they were not statisticallysignificant in vitamin B12-deficient patients.
There was a significant improvement reportedin symptoms within 2-3 months of initiating oralcobalamin in hypothyroid B12-deficientpatients. Although some of the B12-sufficientpatients who had symptoms suggestive ofvitamin B12 deficiency, also had improvementin the symptoms, this may likely to be due toplacebo effect but this needs to be furtherinvestigated and determined by a placebo-controlled study.
Measurement of serum cobalamin is the mostcommonly used biochemical test for diagnosingcobalamin deficiency, but it lacks sensitivity.Studies in the past has established that markersof cobalamin function, particularly totalhomocysteine (tHcy) and Methylmalonic acid(MMA) are elevated in subtle cobalamindeficiency states not characterized by thetypical clinical symptoms [9]. Recently, it wasreported that plasma tHcy concentrations arehigher in vegans than in omnivores [16]. A
similar finding of elevated tHcy and MMA wasobserved in infants in a macrobiotic (vegan)community [17]. Determination of these levelscan lead to early detection of vitamin B12deficiency and can prevent morbidities inhypothyroid patients. Metabolism ofhomocysteine and methylmelonyl acid (MMA)involves cobalamin, which is associated withatherosclerosis [18, 19]. Although we did notmeasure homocysteine levels but other studieshave shown a relationship with hypothyroidismwhich improves with treatment to euthyroidstatus [20, 21].
In developing countries flour fortification wouldpotentially be helpful in improving the vitaminB12 status in the population at large becauseof low intake of vitamin from animal sourcefoods. It could benefit across the life span andit would especially be beneficial for pregnantand lactating women, children and elderly.
Conclusion
Our study has shown that vitamin B12deficiency is common in hypothyroid patientsas well as in patients rendered euthyroid bythyroxine replacement. Screening for vitaminB12 should be undertaken early in the diagnosisof hypothyroidism. Patients with suggestivesymptoms should be evaluated and followedup. Neuropsychiatric symptoms usually act assurrogate markers. Anaemia and macrocytosiscannot be relied upon to point towards vitaminB12 deficiency as it may develop in much laterstages of B12 deficiency. Since there is amarked improvement after replacementtherapy, early diagnosis and treatment isessential in preventing the long-term sequelaeand morbidities of vitamin B12 deficiency.
Acknowledgements
The authors thank the technical staff ofdepartment of nuclear medicine, AtomicEnergy Medical Center for all the technicalassistance.
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:25-31

PJNM 2016, Volume 6, Number 1 30
References
1. Dharmarajan TS, Norkus EP, Ehrenpreis ED,Herbert V, Swain R, Harris MS. Vitamin B12deficiency in the elderly - Population-basedresearch. Round Table Series - Royal Societyof Medicine. 1999;66:27-33.
2. Bhatia P, Kulkarni JD, Pai SA. Vitamin B12deficiency in India: Mean corpuscular volumeis an unreliablescreening parameter. NatlMed J India. 2012?25(6):336-338.
3. Berenson AB, Rahman M. Effect of hormonalcontraceptives on Vitamin B12 level and theassociation of the latterwith bone mineraldensity. Contraception. 2012?86(5):481-487.
4. Tung ML, Tan LK. Long term use ofmetformin leading to Vitamin B12 deficiency.Diabetes Res Clin Pract. 2014;104(3):e75-76.
5. Goodman KI, Salt WB 2 nd . Vitamin B12deficiency. Important new concepts inrecognition. Postgrad Med. 1990;88(3):147-158.
6. Fragasso A, Mannarella C, Ciancio A, SaccoA. Functional Vitamin B12 deficiency inalcoholics: An intriguing finding in aretrospective study of megaloblasticanemicpatients. Eur J Intern Med. 2010;21(2):97-100.
7. Allen LH. How common is Vitamin B12deficiency? Am J Clin Nutr.2009;89(2):693S-696S.
8. Scott JM. Folate and vitamin B12. Proc NutrSoc. 1999;58(2):441-448.
9. Lindenbaum J, Healton EB, Savage DG, BrustJC, Garrett TJ, Podell ER, Marcell PD, StablerSP, Allen RH. Neuropsychiatric disorderscaused by cobalamin deficiency in theabsence of anemia or macrocytosis. N EnglJ Med. 198830;318(26):1720-1728.
10. Nielsen MJ, Rasmussen MR, Andersen CB,Nexø E, Moestrup SK. Vitamin B12 transportfrom food to the body's cells--a sophisticated,
multistep pathway. Nat Rev GastroenterolHepatol. 2012;9(6):345-354.
11. Nachum-Biala Y, Troen AM. B-vitamins forneuroprotection: Narrowing the evidencegap. Biofactors. 2012;38(2):145-150.
12. Jabbar A, Yawar A, Waseem S, Islam N, UlHaque N, Zuberi L, Akhter J. Vitamin B12deficiency common in primaryhypothyroidism. J Pak Med Assoc.2008;58(5):258-261.
13. Snow CF, Laboratory diagnosis of vitaminB12 deficiency. Arch Intern Med.1999;159(12):1289-1298.
14. Lindenbaum J, Savage DG, Stabler SP, AllenRH. Diagnosis of cobalamin deficiency: II.Relative sensitivities of serum cobalamin,methylmalonic acid, and total homocysteineconcentrations. Am J Hematol.1990;34(2):99-107.
15. Camel R. Pernicious anemia. The expectedfindings of very low serum cobalamin levels,anemia, and macrocytosis are often lacking.Arch Intern Med. 1988;148(8):1712-1714.
16. Mann NJ, Li D, Sinclair AJ, Dudman NP, GuoXW, Elsworth GR, Wilson AK, Kelly FD. Theeffect of diet on plasma homocysteineconcentrations in healthy male subjects. EurJ Clin Nutr. 1999;53(11):895-899.
17. Schneede J, Dagnelie PC, van Staveren WA,Vollset SE, Refsum H, Ueland PM.Methylmalonic acid and homocysteine inplasma as indicators of functional cobalamindeficiency in infants on macrobiotic diets.Pediatr Res. 1994;36(2):194-201.
18. Clarke R, Daly L, Robinson K, Naughten E,Cahalane S, Fowler B, Graham I.Hyperhomocysteinemia: an independentrisk factor for vascular disease. N Engl J Med.1991;324(17):1149-1155.
19. Boushey CJ, Beresford SA, Omenn GS,Motulsky AG. JAMA. A quantitativeassessment of plasma homocysteine as arisk factor for vascular disease. JAMA.1995;274:1049-57.
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:25-31

PJNM 2016, Volume 6, Number 1 31
20. Lien EA, Nedrebø BG, Varhaug JE, NygårdO, Aakvaag A, Ueland PM. Plasma totalhomocysteine levels during short-termiatrogenic hypothyroidism. J Clin EndocrinolMetab. 2000;85(3):1049-1053.
21. Barbé F, Klein M, Chango A, Frémont S,Gérard P, Weryha G, Guéant JL, Nicolas JP.Homocysteine, folate, vitamin B12, andtranscobalamins in patients undergoingsuccessive hypo- and hyperthyroid states.J Clin Endocrinol Metab. 2001;86(4):1845-1846.
Pak J Nucl Med 2016;6:25-31 2221-0288(201601/01)6:1<25:VBDPAE>2.0.TX;2-M

PJNM 2016; 6:32-41 331691 © 2016 Pakistan Society of Nuclear Medicine
Validation of Ottawa ankle rule utilizingradionuclide skeletal scintigraphy
Shagufta Zafar Qureshi*,1, Fida Hussain Shah2,Mohammad Amin Waqar2
1Department of Nuclear Medicine, Federal Government Polyclinic Hospital,Islamabad, Pakistan
2Nuclear Medical Center (NMC) Armed Forces Institute of Pathology (AFIP)Rawalpindi, Pakistan
ORIGINAL ARTICLE
Abstract
Aims Ankle and foot injuries, especially amongteenagers and young adults, are frequentlyencountered by the primary care physicians.Most common ankle injuries are sprains due toinversion injuries to the lateral ankle ligaments.It has been observed that the overall number ofankle radiographs in the ER is around 15-20%,which includes about 30-40% unnecessaryradiographs. Ottawa Ankle Rule (OAR) was firstestablished in 1992, to reduce that unnecessaryload on x-ray departments. In light of the currentuniversal practice of evidence-based medicine itis important to undertake verification of thesubjective OAR. Bone scintigraphy by merit of itshigh sensitivity was chosen as the imagingmodality of choice to validate the accuracy ofOAR.
Methods The study population comprised of50 OAR-positive cases and 10 normal controls.
Each case was scanned using 3-phase bonescintigraphy (TPBS), following a preliminaryradiograph.
Results Out of 50 OAR-positive cases, x-raysshowed frank fractures in only 12 cases,whereas bone scan was positive in 45 cases,out of which 43 had active bone lesions, theremaining 2 had a soft-tissue injury. Byconsidering the TPBS bone scan as the goldstandard, we found the sensitivity of OAR was95% and specificity 61.5% with PPV and NPVat 90% and 80% respectively.
Conclusion We conclude that there is a highconcordance between the OAR and the bonescan and that the OAR is evidence-based asdetermined by the successful verification of theOAR by the TPBS in 95% of the cases. Basedon our findings we recommend the routinepractice of the OAR in all emergencydepartments. In patients with acute ankle/footinjuries, with a positive OAR, even with anegative x-ray, the injury should not be takenlightly and if required, a bone scan should beperformed for confirmation of lesion. Bonescintigraphy rather than plain radiographyappears to be the modality of choice in thissituation being cost- and time-effective withoutcompromising the quality of medical care.
*Correspondence
Dr shugufta Zafar Qureshi Nuclear Medical Centre (NMC) Armed Forces Institute of Pathology (AFIP) Rawalpindi Cantt Email: [email protected] Tel: +923367000725
www.pjnm.net 2221-0288(201601/01)6:1<32:VOOARU>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 33
Key words: Ottawa ankle rule, radionuclidebone scan, x-ray, radiograph
Introduction
Ankle and foot injuries, especially amongteenagers and young adults, are commonlyencountered by the primary care physicians.The commonest ankle injuries are sprains dueto inversion injuries to the lateral ankleligaments [1]. It has been observed that theoverall number of ankle radiographs in theemergency room (ER) is around 15-20% [2],which includes about 30-40% unnecessaryradiographs [3].
Although at first glance, ankle injuries mayappear to be minor, up to 44% of patientsmay have persistent symptoms one year afterthe injury. Though only a few of these casessuffer a fracture, nearly all are investigatedthrough plain x-rays of the ankle or foot, orboth [4]. To deal with this clinical problem, aset of guidelines known as the Ottawa anklerules, were first developed at the Universityof Ottawa in Canada in 1992 [5], stating thatankle x-rays are only required if there is anypain or tenderness at posterior edge or tip ofeither of the malleoli, and foot x-rays are onlyrequired if there is any pain or tenderness atthe base of 5th metatarsal or the navicularbone or the patient is unable to bear weightboth immediately post injury and in theemergency department.
Stiell et al. in 1994 [6] showed that by properimplementation of this rule there was areduction in ankle radiography by 28%.Pigman et al. [7] also studied acute ankleinjuries in emergency departments of threehospitals during the pre-intervention andintervention periods and observed significantreduction in radiographic requests.
The impact of the Ottawa ankle rules in a USArmy troops medical clinic in South Korea wasstudied by Spriger et al. [8] who reported asensitivity and specificity for the rules at 70%and 73% respectively. The positive andnegative predictive values were 31.8% and
93.3% respectively. Leisey et al. in 2004observed that correct implementation of theOAR has a definite potential to decrease theuse of radiographic resources in deployedmilitary population [9]. Papacostas et al.(2001) studied Ottawa ankle rules protocol inGreek athletes and concluded that the Ottawaankle rules protocol is 100% sensitive [10].Karpas et al. (2002) studied the application ofOAR in paediatric emergency department andfound that the use of the OAR had reducedthe radiography rate by 21% [11].
All prior reported studies were aimed atutilizing these rules for the prediction of frankfractures by plain radiography. In contrast,we have attempted to validate the OARthrough bone scintigraphy, the most sensitivediagnostic modality for skeletal trauma. Thisfirst reported study of its type compared theOAR findings with x-ray and bone scan resultswith an aim to validate the sensitivity andspecificity of OAR.
Patients and Methods
The study was carried out at Nuclear MedicalCenter, Armed forces Institute of Pathology,Rawalpindi. The patients were referred from theorthopaedic department of the CombinedMilitary Hospital, Rawalpindi. A total of 60subjects were studied, which included 10normal controls (6 males, 4 females) and 50patients with acute ankle or mid foot injuries(41 males, 9 females) fulfilling the criteria fora positive Ottawa ankle rule. The age of thesubjects ranged from 12 to 64 years (mean29±12 years). Each patient was examined by3 doctors including a general physician, asurgeon/orthopaedician and a nuclear medicinephysician. The study exclusion criteria weremore than 30 days since injury, pregnancy, anobvious deformity of ankle or foot, crushinjuries, diabetic foot, and children below 12years of age.
After routine history taking and clinicalexamination, fresh ankle and foot x-rays (APand lateral views), were advised. The studyprocedure was explained to the patient and
331691 © 2015 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:32-41

PJNM 2016, Volume 6, Number 1 34
informed consent was taken. A 3-phase bonescan was performed on the next working dayusing dose injected in each case was 16 mCi.The patient was positioned supine under thegamma camera fitted with a low-energygeneral-purpose collimator and 16 mCi (~600MBq) of technetium-99m labelled methylenediphosphonate (99mTc-MDP) was injectedintravenously. A dynamic flow study (1stphase) was obtained at 1-sec/frame for 60seconds. This was followed by a blood poolimage at 2 minute (2nd phase), for 1 min. Fourdelayed static images in the anterior, posterior,right-lateral and left-lateral projections were
subsequently at 3 hours postinjection (3rdphase). The delayed spot views werecount-based with 300 k-counts per image.The scan were interpreted independently bythree nuclear medicine specialists.
Statistical analysis The data was tabulatedand the means and standard deviations (S.D.)were calculated for each group and thechi-squared test applied to obtain statisticalinference considering p value of <0.05 assignificant. Taking the bone scan as thegold-standard, the sensitivity, specificity, PPVand NPV of Ottawa ankle rule were calculated.
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:32-41
Sr.
no.
Clinical
Features
(symptoms)
Freq. % Freq. X-Ray Findings
(frequency)
Bone scan Findings
(frequency)
Fracture NAD A.B.L.
(% age of
lesion
detection)
NAD
1 Pain + Swelling
+ Inability of
wt.bearing
12 24 12
(100%)
- 12 (100%) -
2 Pain + Swelling. 6 12 - 6 6 (100%) -
3 Swelling only 2 4 - 2 2 (100%) -
4 Pain only 25 50 - 25 25 (100%) -
5 No pain, No
swelling
5 10 - 5 - 5
Sign:Tenderness
(OAR+ve)
50 100% 12 38 45 5
6 Medial
malleolus
18 36 3 15 16 (88.8%) 2
7 Lateral
malleolus
17 34 4 13 16 (94.1%) 1
8 Navicular 12 24 3 9 10 (83.3%) 2
9 Base of 5th
metatarsal
3 6 2 1 3 (100%) -
Net Result 50 100% 12 38 45 5
NAD: No abnormality detected. OAR: Ottawa ankle rule. Wt: weight. % Freq.: percentage frequency. A.B.L.: Activebone lesion.
Table 1 Relationship between clinical features, x-ray findings and bone scan in OAR-positivecases

PJNM 2016, Volume 6, Number 1 35
Results
Out of the 50 OAR-positive patients, only 12cases had a complete fracture detected byx-rays, with the patients complaining of pain,swelling and tenderness and all of them wereunable to bear weight on the affected side. Restof the clinical findings, x-rays and bone scanresults are shown in Table 1.
Out of the 50 OAR-positive cases, 45 hadpositive scans, i.e. 90% of lesions were pickedup by bone scan, while only 10% of OAR-positive cases had a normal bone scan.
Figure 1 shows the ability of various diagnosticmodalities to pick bone and soft-tissue lesions.In this study, out of 50 OAR-positive cases,x-ray could pick only 24% of the lesions (12 outof 50) and missed 76% of the lesions, whereasin contrast 90% of the lesions (45 out of 50)were picked up by bone scintigraphy which alsoincluded two soft-tissue injuries, that werepicked up by Ottawa ankle rule and wereconfirmed by the bone scan.
For our control group we selected 10 OAR-negative individuals as control subjects, 7 outof 10 of whom were army personnel.
Optimisation of results was performed todetermine the best technique for the diagnosisof acute ankle/foot injuries or arrive at the bestpossible combination (see Table 2).
Chi-squared test applied to obtain statisticalinference considering p value of <0.05 assignificant considered the null hypothesis, i.e.x-ray and bone scan are equally good forvalidation of Ottawa ankle rule. With thedegree of freedom 1 and p value as <0.05,we found that our calculated value (22.7) wasmuch higher than tabulated value (3.84),thereby rejecting the null hypothesis andallowing us to conclude that the bone scanwas significantly superior to x-ray forvalidation of Ottawa ankle rule.
Since OAR is a set of clinical criteria based onsubjective finding, it cannot form a criterionfor evidence based medicine. For its validationwe selected the most sensitive imagingmodality, i.e. bone scan, as the gold standardand determined the sensitivity of OAR at 95%,specificity at 61.5%, positive predictive value(PPV) at 90%, and negative predictive value(NPV) at 80%.
Discussion
Ankle and foot injuries are very common inclinical practice, constituting a majorproportion of cases in emergency medicine.X-Ray is considered to be the most importantmethod of evaluation of bone lesions, butmost of the times, it just increases the work
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:32-41
Table 2 Optimisation of the results
Group Number X-Ray Findings Bone scan Findings
Fracture NAD A.B.L. NAD
Patient (OAR +ve) 50 12 38 45 5
Control (OAR -ve) 10 - 10 2 8
NAD: No abnormality detected. A.B.L.: Active bone lesion.
Figure 1 Comparison between clinicalevaluation criteria (OAR), x-ray and bonescintigraphy

PJNM 2016, Volume 6, Number 1 36
load on x-ray department [2]. The Ottawaankle rule (OAR) was introduced in 1992 tocope with this problem. The OAR incorporatesguidelines for ordering x-rays in acute ankleand mid-foot injuries [5]. Appropriateutilization of OAR can reduce the number ofradiographic requests by 22.4% [12].
These days evidence-based medicine isstressed by the medical professionals. TheOAR, being only a set of clinical criteria, couldbe called as subjective only [15]. This is oneof the reasons that children below 12 years ofage were not included in the study, as OAR isa clinical judgement, which is difficult toappreciate in children correctly and there isalways a chance of over estimation. ThoughDayan et al. in 2004, observed malleolar zoneand mid-foot zone fractures in children andfound the rule to be reasonably sensitive [14].
In this particular scenario, it was essential,that there should be an evidence-based studyfor validating these rules, and for this purposewe chose the highly sensitive imagingtechnique of the radionuclide bone scan. Thusto fulfil the criteria of evidence-based medicinefor the validation of OAR, we utilized theradionuclide bone scan, which has proven highsensitivity and a reasonably high specificity[16,17] and found that the sensitivity of theOttawa ankle rule came out to be 95%,positive predictive value and negativepredictive value were 90% and 80%respectively.
We performed x-rays and bone scans on all ofthe 50 OAR-positive patients and observedthat that out of 50 cases only 12 (24%) hadfractures on x-rays whilst 45 (90%) hadpositive bone scans and out of these 45, 43had active bone lesions and 2 had soft-tissueinjuries.
Our control group included 10 volunteers, allOAR negative. But out of these 10, 7 weremilitary personnel, who routinely undertakephysically stressful activities [13] with theresult that 2 (20%) subject (Table 2), had afalse-positive scan. We presume that if wecould take a larger control group and all were
selected from the general public rather thana fixed occupational group, the results couldbe even better.
Our study is an analytical study in which wevalidated the OAR using the radionuclide bonescan. In the study, out of the 50 OAR-positivecases, only 12 (24%) came out to be frankfractures picked up by the plain radiographs(Table 1). The rest of the 38 cases weresprains, confirming the fact that a sprain ismuch more common problem that can beeasily missed by an x-ray, but can be pickedup by clinical assessment criteria i.e. OAR.
In this study, we could detect a wide range oflesions with fixed assessment criteria used.Figure 2 shows an intensely hot lesion at thebase of the 5th metatarsal in the left foot,which was due to a fracture picked up by plainradiography. But on the bone scan, it wasobserved that adjacent talus also had anactive bone lesion, which was not detected byplain x-ray, indicating the usefulness of bonescan in the diagnosis of such cases.
Another important finding was presence of soft-tissue lesions (Figure 4) indicating that OARcriteria are so valid and significant and thatthey can even pick up soft-tissue injuries,which definitely needs early identification andmanagement in order to avoid long-termcomplications [18].
In our control group, we have seen that thefalse-positive rate was rather high (20%)representing 2 out of 10 cases. This could bedue to high bone scan sensitivity [19], thatcan even pick up mild, localized inflammatorylesions, associated with routine stress (as inour case of military personnel) who wereotherwise asymptomatic. This results in highfalse-positive values, reducing the specificityof the rule, which in our study came out to beat 61.5%. We think that if we have to applyOAR randomly on the general public, thespecificity will be definitely higher due to lowerfalse-positive rate.
It was observed that, in almost all the casesthere was increased perfusion and blood pool
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:32-41

PJNM 2016, Volume 6, Number 1 37
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:32-41
Figure 2 A 52-year-old male (case 1) with a history of trauma to the left foot withtenderness at base of the left 5th metatarsal and navicular bones. Bone scan (left) showsactive bone lesions at the base of left 5th metatarsal and the adjacent talus, with the x-ray(right) showing fracture at the base of the left 5th metatarsal
Figure 3 A 34-year-old female (case 2) with history of trauma to the right foot withtenderness over the right navicular bone. Bone scan (left) shows an active bone lesion inthe right talus, with a normal x-ray (right)
Figure 4 A 41-year-old male (case 3) with history of trauma to the left foot with tendernessbelow and behind the lateral malleolus. Bone scan (left) shows increased uptake in lateralmalleolus on the perfusion and blood pool images with normal delayed views consistentwith soft-tissue injury; the x-ray is normal (right)

PJNM 2016, Volume 6, Number 1 38
on the contralateral side and delayed staticviews also showed slightly raised traceruptake. We know that whenever there isincreased pressure or weight bearing at anysite, this initiates a remodeling process in thebone, causing increased radiotracer uptake[20], but such uptake is physiological.
One may query the importance of a set ofclinical criteria. The answer to that questionis cost, time and convenience. A simple butthorough clinical examination involvesminimum time and cost equivalent to a singlevisit to a physician and with no radiationexposure. We may wonder that on a simpleclinical examination one may somehow misssome important findings. However, we haveseen that by simply utilizing the OAR criteria,we can pick as minute bone lesions, stressfractures, and even soft-tissue injuries, whichcan only be detected by bone scintigraphy.These stress-related injuries, if missed, cantransform into more serious lesions such asconversion of stress fractures into frankfractures, which can be avoided by utilizingthe OAR [21].
Another important aspect is the costeffectiveness of the implementation of therule. We have made a rough estimate of costfor unnecessary x-rays in this study, and itwas observed that at least 20-30% of the total
cost and a lot of precious time can be saved,if the OAR is properly utilized.
One thing that is worth mentioning is that, weare not recommending bone scan for everypatient with a positive OAR, rather we aresuggesting that there is no need of anydiagnostic test after a positive OAR in a patientwith acute ankle injury. We can directly switchon to the management, which in most of thecases is conservative and involvesimmobilization, analgesics and antiinflammatory drugs for 3-6 weeks [22]. But iffor some reason confirmation of lesion isessential, for example for somedocumentation like job requirements,insurance purposes, etc., one should go forbone scintigraphy as it will most accuratelypick up all types of bone lesions.
We therefore strongly recommend that with aOAR is positive, a person should be consideredas an injured person and he/she shouldreceive optimal treatment. But if the physicianhimself is not very confident in declaring thepatient as OAR-positive, in mild cases, only1-2 weeks immobilization with mild analgesicswill be enough and neither x-ray nor bonescanning is recommended [19].
The discussion above may give a falseimpression that perhaps we totally negate the
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:32-41
Figure 5 A 16-year-old female (case 4) with history of trauma to the left foot withtenderness over the lateral malleolus. Bone scan (left) shows an active bone lesion in theleft lateral malleolus; the preliminary x-ray was reported to be normal but a repeat x-rayconfirmed the lesion

PJNM 2016, Volume 6, Number 1 39
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:32-41
Acute ankle / foot injuries
History and Clinical examination
OAR positive OAR negative
ObserveGo for Management
For confirmation of lesion
X-Ray (very low
sensitivity): 24%
Bone scan (very high
sensitivity): 90%
Doubtful cases
Well localized, intense uptakeMild uptake
No need of x-rayx-ray indicated
Figure 6 An algorithm for assessment of the patients with acute ankle/foot injuries

PJNM 2016, Volume 6, Number 1 40
importance of plain radiograph. This is not thecase as x-rays are definitely indicated in somecases where we need a higher specificityrather than high sensitivity. So whenever anorthopaedician is suspecting a frank fracturethat may need some intervention like openreduction or internal fixation, x-ray is stronglyindicated.
Now the question arises when one should gofor x-ray after bone scintigraphy? The answeris, when the lesion is very hot and welllocalized in all the 3 phases of 3-phase bonescan. This is an indication for plain radiographafter bone scintigraphy but the simple visualimpression will not be enough. Semi-quantitative analysis should decide the cutoffpoint in such cases. A bone scan will thencompliment the x-rays. Another possibilitycould not be excluded was that that fractureswere present and radiologist was unable tosee the fractures. Even in our study, we had2 cases, one of which is shown in Figure 5,where the patient had a twisting eversioninjury of left foot and the initial x-ray wasreported as normal whereas bone scandetected an intense, well-localized lesion atleft lateral malleolus. Repeat x-ray was thenperformed, of the specific site with a specificzoom and it was then reported to have ahairline fracture at the level of the lateralmalleolus.
We propose an algorithm for the assessmentof the patients with acute ankle/foot injuries(Figure 6) and we expect that if the physiciansfollow this algorithm for evaluation of patientswith acute ankle/foot injuries, there will be aminimum chance of missing a significant lesionand the quality of medical care will definitelyimprove.
We recommend extensive utilisation of theOttawa ankle rule in surgical emergencydepartments, to detect all sorts of bone lesionsin acute ankle/foot injuries. The emergencystaff should be properly trained to learn andimplement OAR in all the cases with acuteankle and foot injuries.
Conclusion
Evidence supports the Ottawa ankle rule asan accurate and very effective instrument fordetection of the ankle and mid foot injuries.The OAR has a sensitivity of 95% which iscomparable to bone scintigraphy andreasonably high specificity at 61.5%.Therefore in patients with acute ankle/footinjuries, with positive OAR, even with anegative x-ray, the injuries should be takenseriously. However, in difficult cases, bonescan can play a complementary role to plainradiographs. The widespread application ofOAR can save both time and money withoutcompromising quality of medical care.
References
1. Bachmann LM, Kolb E, Koller MT, et al. The Ottawaankle rules have a high sensitivity for excludingfractures of the ankle and midfoot in acute anklesprain. Evid Based Med. 2003;8:185.
2. McCann B. Prospective survey to verify the Ottawaankle rules. J Accid Emerg Med. 2000Jan;17(1):75-76.
3. Dowling S et al. Accuracy of Ottawa Ankle Rules toexclude fractures of the ankle and midfoot inchildren: a meta-analysis. Acad Emerg Med. 2009Apr;16(4):277-287.
4. Murray SR, Reeder MT, Udermann BE, Pettitt RW.High-risk stress fractures. pathogenesis,evaluation, and treatment. Compr Ther.2006;32(1):20-25.
5. Stiell IG, Greenberg GH, McKnight RD, Nair RC,McDowell I, Worthington IR. A study to developclinical decision rules for the use of radiography inacute ankle injuries. Ann Emerg Med.1992;21:384-90.
6. Stiell IG, McKnight RD, Greenberg GH, et al.Implementation of the Ottawa Ankle Rules. JAMA.1994;271:827-32.
7. Pigman EC, Klug RK, Sanford S, et al. Evaluationof the Ottawa clinical decision rules for the use ofradiography in acute ankle and midfoot injuries inthe emergency department: An independent siteassessment. Ann Emerg Med. 1994;24:41-45.
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:32-41

PJNM 2016, Volume 6, Number 1 41
8. Springer et al. A Prospective Study of ModifiedOttawa Ankle Rules in a Military Population:Interobserver Agreement between PhysicalTherapists and Orthopedic Surgeons. J Am MedAssoc. 2000;28:864-868.
9. Leisey, John K, et al. Prospective Validation ofOttawa Ankle Rule in Deployed MilitaryPopulation.. Military Med. 2004;34:236-239.
10. Papacostas et al. Validation of Ottawa anklerules protocol in Greek athletes: study in theemergency departments of a district generalhospital and a sports injuries clinic; Br J SportsMed 2001;35:445-447.
11. Karpas et al. Utilization of the Ottawa AnkleRules by Nurses in a Pediatric EmergencyDepartment; Acad Emerg Med. 2002;9:130-133.
12. Auleley G-R, Ravaud P, Girauduaeu B, et al.Implimentation of the Ottawa ankle rule inFrance: a multicenter randomized controlledtrial. J Am Med Assoc. 1997;277: 1935-1939.
13. Rosen A, Sinopoli M et al. Impact of Ottawaankle rules in a U.S. Army troop medical clinicin South Korea. Military Med. 1999;164:793-794.
14. Dayan et al. Derivation of Clinical PredictionRules to Identify Children with Fractures afterTwisting Injuries of the Ankle Acad Emerg Med.2004;11:736-743.
15. Michelle J, Michael R. S, John D. K. ClinicalUsefulness of the Ottawa Ankle Rules forDetecting Fractures of the Ankle and Mid foot. JAthl Tr. 2010;45(5):480-482.
16. Cross well S, Leaman A, Phung W. Minimisingnegative ankle and foot X-rays in the EmergencyDepartment -- are the Ottawa ankle rules goodenough? Injury. 2014;45(12):2002-2004.
17. Freeman LM, Blaufox MD. Editors; Orthopedicnuclear medicine (part 1), Semin Nucl Med.1997;27:307-389.
18. Mcgriff-Lee, Management of Acute Soft TissueInjuries; J Pharm Pr. 2003;16:51-58.
19. Lowrence EH. Orthopedic Imaging in Traumaand Sports Medicine. In: Lowrence E. H, Manuel
L. B, eds. Skeletal Nuclear Medicine, 2ndedition.1990;225-258.
20. MatiYong-W Bahk, Yong-An Chung, Use ofGamma Correction Pinhole Bone Scans inTrauma. Nucl Med Mol Imaging.2012;46(1)10-19.
21. Thrall Bachmann et al. Accuracy of Ottawa Anklerules to exclude fractures of the ankle and midfoot: BMJ, Feb. 2003:326-417.
22. Jeffery D. Tiemstra. Update on Acute AnkleSprains. Am Fam Physician. 2012;12: 1170-1176.
Pak J Nucl Med 2016;6:32-41 2221-0288(201601/01)6:1<32:VOOARU>2.0.TX;2-M

PJNM 2016, 6:42-47 331691 © 2016 Pakistan Society of Nuclear Medicine
Radiosynoviorthesis in pigmentedvillonodular synovitis using Re-188 labelled tin
colloid: a case report
Aakif U Khan1, Hameedullah*,2, Abdul Saeed Shah2,Muhammad Rauf Khattak2
1Swat Institute of Nuclear Medicine, Oncology and Radiotherapy (SINOR),Saidu Sharif, Swat, Pakistan
2Institute of Radiotherapy and Nuclear Medicine (IRNUM),Peshawar, Pakistan
CASE REPORT
Abstract
Radiosynoviorthesis (RSO) is an attractivealternative to surgical synovectomy forcontrolling symptoms of rheumatoid arthritisand many other chronic proliferative jointdiseases. The procedure is not widely used inour country because of the non-availability ofsuitable radionuclides and radiopharmaceu-ticals. The production of rhenium-188 (188Re)from 188W/188Re generator and by labelling itwith particles of appropriate size, has a promiseto offer. We labelled 188Re with tin colloid andanalyzed its biodistribution and clinical efficacyafter injecting it to a patient with recurrentpigmented villonodular synovitis. Gammacamera imaging performed after 1, 24 and 48hrs showed no leakage of theradiopharmaceutical from the injected joint.The clinical outcome of this study was also
excellent, which suggests that 188Re labelledtin colloid is a potentially effectiveradiopharmaceutical for recurrent PVNS andcan be used for other chronic inflammatoryjoint diseases.
Key words: PVNS, Particle size, Radio-synoviorthesis, 188Re tin colloid
Introduction
Radiosynoviorthesis (RSO) is an effectivealternative tool for restoration of synoviumin chronic inflammatory joint diseases (CIJD)in carefully selected patients. The procedureis based on an intra articular injection ofß-emitting radiopharmaceuticals directly intothe affected joint space in an effort to ablatethe synovium [1-3]. The radiopharmaceuticaldeposits almost all of its ß energy on theinternal lining of the inflamed andproliferative synovium. This destroys theproliferating synovial cells of the involvedjoint and will enable it to restore a nearnormal lining. RSO can be helpful in a number
*CorrespondenceMr. HameedullahInstitute of Radiotherapy &Nuclear Medicine (IRNUM),Peshawar, PakistanTel: +92-091-9216114-7Email: [email protected]
www.pjnm.net 2221-0288(201601/01)6:1<42:RIPVSU>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 43
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:42-47
of conditions including rheumatoid arthritis(RA), osteoarthritis, haemophiliac synovitis,synovial chondromatosis, PVNS and someother rare inflammatory arthritic diseases[2-4].
PVNS is a rare, aggressive, non-malignantproliferative histiocytic joint lesion that causesswelling, pain and loss of mobility in theaffected joint [5]. The disease poseschallenges in the management. It is primarilytreated by open or orthroscopic synovectomywith reasonable success rates but there is ahigh risk of recurrence ranging from 8-46%depending on extent and severity of disease[6, 7].
In such conditions, RSO plays an appealingrole in that it selectively irradiates theproliferating synovium without any significantradiation burden to the rest of the body [8].Radiopharmaceuticals with strong ß emissionsand soft-tissue penetration are ideal for RSO[4, 9]. The most commonly used radiopharmaceuticals for RSO along with theirphysical properties are presented in Table 1.
188Re has excellent nuclear and chemicalproperties, therefore its potentials are beingexplored in a variety of clinical settings. 188Reis available from 188W/188Re generator whichoffers significant advantages in terms of
in-house availability and convenience with lowcost as compared to other therapeuticradionuclides [10]. Owing to its deep tissuepenetration (10 mm), 188Re is consideredsuitable for treatment of large and some timemedium joint diseases. In this study, 188Re Tincolloid was prepared and its biodistributionwas assessed after intra articular injection intothe knee joint affected by PVNS underultrasound guidance.
Case Report
A 17-year-old girl was referred to the nuclearmedicine department of Institute ofRadiotherapy and Nuclear Medicine (IRNUM)for treatment of PVNS. She had undergonemultiple open surgical synovectomies over thelast 18 months. On examination, she had alarge swollen right knee joint with multiplescars of past surgical synovectomies [Figure 1].The joint had a limited mobility and was tenseand tender. The patient had undergone de-bulking surgery and removal of septations priorto 188Re-RSO. After four weeks of the debulkingsynovectomy, the patient underwent RSO. 185MBq (5 mCi) of 188Re tin colloid was injectedinto the right knee joint under ultrasoundguidance at 2 sites. After 1 hour, an image ofthe knee was acquired to look for biodistributionof the radiopharmaceutical (Figure 2).
Table 1 Radiopharmaceuticals clinically used in radiosynovectomy
Radiopharmaceticals β Emax
(MeV)γEmax(KeV)
T1/2 Penetration(mm)
Particlesize (µm)
32P chromic phosphatecolloid
1.71 -- 14.3d 7.9 500-2000
90Y citrate or silicate 2.27 -- 2.7d 11 100
165Dy FHMA 1.29 95 2.33h 5.7 3000-8000
165Dy FHMA 1.29 95 2.33h 5.7 3000-8000
188Re microspheres 2.12 155 17h 10 10-20
169Er citrate 0.34 -- 9.4d 1.0 10

PJNM 2016, Volume 6, Number 1 44
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:42-47
Injection technique
The involved joint was draped and preparedaccording to standard sterile techniques. A 185 Mbqdose was then injected into the affected knee jointof the patient under ultrasound guidance using a20-gauge needle. The joint was brought through afull range of motion to improve distribution of theradiopharmaceutical and was then splinted forcomfort and for limiting the extra articular leakageof the radiopharmaceutical.
Follow-up procedure
We evaluated our patient for pain relief, swellingand quality of life at 2, 4, 6 and 8 weeks, and thenafter every 2 months until one year. At the timeof injection, the patient complained of tolerablepain, which subsided after the needle wasremoved. After 2 weeks, the patient had mildreduction in the pain, effusion and size of the jointswelling. After 4 weeks, the knee circumferencewas markedly reduced from 30.9 cm to 27.3 cm(Figure 3). The joint mobility was also improvedfrom completely immobile to flexion of about 450at the affected knee joint. After eight weeks thepatient was completely asymptomatic (pain free)
Figure 1
Figure 2 1-hour images of the kneeshowing the distribution of the radiopharmaceutical in the knee joint
To see any leakage, imaging was alsoperformed at 24 and 48 hours (Figure 3). Thepatient was assessed for pain, swelling andmobility, every two weeks from the date ofinjection for two months and then on everytwo months for one year.
Quality control of radiopharmaceutical
Radiochemical purity (RCP) of the radiopharmaceutical was determined by paperchromatography using Whatman paper 1 in normalsaline and acetone. RCP was found to be 98.0+0.2%,which was then brought to 100% throughcentrifugation. Particle size was also determinedthrough electron microscopy from CentralizedResource Laboratory, Peshawar University.
Figure 3 Delayed images of the knees(left) and pelvis (right) at 24 (top) and 48hours (bottom)

PJNM 2016, Volume 6, Number 1 45
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:42-47
without taking any analgesics and the swellingsubsided over the next six months. The patientis still free of symptoms and at timescomplains of slight pain which subsides aftersome rest.
Biodistribution
Early 1-hr and delayed 24-hr & 48-hr anterior andposterior images of the knee joint and pelvis(Figure 2) were acquired to see if there was anyleakage of the radiocolloid especially into theregional lymph nodes. The biodistribution studywas performed on Siemens Orbiter gammacamera with low-energy all-purpose (LEAP)collimator with energy window of 15% centeredat 155 KeV photo peak. We found no focal areaof abnormal tracer accumulation and all the 188Relabelled colloid was found localized to the injectedjoint space.
Discussion
PVNS is a rare, aggressive but benignproliferative histocytic joint lesion, whichresults in various degrees of villous and/ornodular changes in the affected joint structure[2, 11]. It poses serious challenges in themanagement because surgical attempts arenot successful in most of the cases andfrequent recurrences are common. Repeatedsurgeries are associated with greatermorbidity and may result in complications like
infections and limitation of movement [12].With recent advances in the field oftherapeutic nuclear medicine, in suchscenarios, RSO offers a quick and economicalsolution [3, 10].
In this process mostly ß-emitting radionuclideslabelled with particulate compounds areintroduced into the affected joints. As there ispresumably no leakage outside the jointcavity, the radiolabelled colloid deposits mostof its ß-energy on the internal lining of thejoints when these are phagocytosed by thefree floating fluid macrophages [4, 13].
RSO is regularly practiced in Australia andCanada as well as in other Western Europeancountries but it is very common in Germany.According to an estimate, RSO is performedin about 70,000 joints per year in Germany[4]. However, it hasn't gained widespreadacceptance in the developing or underdeveloping countries where its clinical benefitscan be better utilized, mainly due to thenon-availability of the isotopes and resultinglack of expertise in the field.
The physical and chemical properties of theradionuclide as well as the particle size of thelabelled colloid, are important factorsconsidered for RSO. The availability of 188Refrom 188W/188Re generator, has made thenuclear medicine community take interest inthis isotope because of its favourable physicalproperties. 188Re (T1/2=16.9 hrs) is the decayproduct of its parent 188W (T1/2=69.4 d). It hasa β energy of 2.12MeV (70%) accompaniedby a 155 KeV γrays. The additional 155 KeVγray emission can be helpful for imaging orbiodistribution studies. It has a deep tissuepenetration of 10 mm as compared to otherisotopes. These physical properties and itspotential low cost associated with a long-livedparent makes it a suitable candidate forradionuclide therapies in large joint RSO.
Similarly various size particles ranging from11000 μm has been applied for RSO in theliterature. But for homogenous distributionand to be phagocytosed easily by the lining
Figure 3

PJNM 2016, Volume 6, Number 1 46
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:42-47
cells of the synovium, particles with small sizeare preferred [13]. However, they have anassociated high risk of leakage from thetreated joints resulting in a higher radiationdose to the non-target organs. To overcomethis problem, radiolabelled particle of 210μmsize are considered suitable [14].
In this case, we selected tin colloid as a carrierwith particle size 0.1–2±0.2 μm. To avoidleakage, the larger labelled particles wereisolated from the smaller ones throughcentrifugation. The biodistribution studies(imaging at 1, 24 & 48 hours) showed thatfollowing intra-articular injection, 188Re tincolloid is retained in the knee joint throughoutthe study. The 24-hr and 48-hrs postinjectionimages prove the efficacy of 188Re tin colloidas a better radiation synovectomy agent.
This particular patient had undergone multiplerepeated surgical interventions, which hadcaused some degree of scarring and pocketformation in the joint space that was treatedby pre RSO surgical de-bulking and removalof intervening septa. The double site ofinjection ensured adequate distribution of thetracer. The clinical response at two years offollow-up is satisfactory. The patient marriedafter one year of treatment and has recentlygiven birth to a healthy male child. She hasslight limitations of movements with noswelling and occasional slight pain. Thelimitation of movement is attributed toscarring due to previous surgery.
The clinical outcome, ease of administrationand comparatively lower cost than surgicalsynovectomy, make RSO a reasonable optionin the therapy of PVNS. This is however asingle case and further studies are needed tobetter define the role of 188Re labelled tincolloid in PVNS.
Conclusion
PVNS is a slow growing but challenging jointlesion and RSO remains a viable option for itsmanagement [15]. In this connection 188Relabelled tin colloid is an economical and readily
available radiopharmaceutical for patients withrecurrent PVNS who are unresponsive totraditional therapy.
References
1. Mödder G. Radiosynoviorthesis. In:Biersack H J, Freeman LM, editors. ClinicalNuclear Medicine. Berlin Heidelberg:Springer-Verlag; 2007.p. 512-518.
2. Karavida N and Notopoulos A. RadiationSynovectomy: An effective alternativetreatment for inflamed small joints:Hippokratia 2010; 14(1): 22-27.
3. Clunie G, Fischer M. European Associationof Nuclear Medicine procedure guidelinesfor radiosynovectomy. Eur J Nucl Med MolImaging. 2003; 30 BP 12- 16.
4. Modder G, Modder-Reese R.Radiosynoviorthesis. In: Aktolun C,Goldsmith SJ. Nuclear Medicine therapy-principles and clinical applications, NewYork: Springer; 2012.p. 315-355.
5. Wu CC, Pritsch T, Bickels J, Wienberg T,Malawer MM. Two incision synovectomy andradiation treatment for diffuse pigmentedvillonodular synovitis of the knee with extraarticular component. Knee, 2007; 14: 99 -106.
6. Schweitzer ME, Laredo JD. New Techniquesin Interventional Musculoskeletal Radiology.Informa Healthcare, 2007. p.195-203.eBook ISBN: 978-1-4200-1430-3
7. Kat S, Elbracht T et al. Radiosynovectomyin pigmented villonodular synovitis. J NuclMed 2000; 39(7): 209-213.
8. Elgazzar, Abdelhamid H. Basis ofTherapeutic Nuclear Medicine. In: Synopsisof Pathophysiology in Nuclear Medicine;New York: Springer InternationalPublishing; 2014.p. 322-324.
9. Kampen WU, Fischer M. Local Treatment ofInflammatory Joint Diseases, Benefits andRisks; Springer, New York, 2015.p. 81-90.

PJNM 2016, Volume 6, Number 1 47
Pak J Nucl Med 2016;6:42-47 2221-0288(201601/01)6:1<42:RIPVSU>2.0.TX;2-M
10. Kampen WU, Brenner W, Kroeger S.Long-term results of radiationsynorectomy: a clinical follow-up study.Nucl Med Commun. 2001; 22: 239-246.
11. Nassar WAM, Bassiony AA, and ElghazalyHA. Treatment of Pigmented VillonodularSynovitis of the knee with combinedsurgical and radiosynovectomy. HSS J.2009; 5(1):19-13.
12. Siegel HJ, Luck VJ Jr, Siegel ME. Advancesin radionuclide therapeutics. J Am AcadOrthop Surg. 2004; 12: 55-64.
13. Valotassiou V, Wozniak G, DemakopoulosN, Georgoulias P. Radiosynoviorthesis -indications, side effects. Hell J Nucl Med.2006; 9: 187-188.
14. Schneider P, Farahati J, Reiners C.Radiosynovectomy in Rheumatology,Orthopedics, and Hemophilia. J Nucl Med2005; 46: 48S-54S.
15. Tyler WK, Vidal AF, Williams RJ and HealeyJH. Pigmented Villonodular Synovitis. JAm Acad Orthop Surg. 2006; 14(6):376-85.

PJNM 2016, 6:48-52 331691 © 2016 Pakistan Society of Nuclear Medicine
Unusual spinal metastases from an adenoidcystic carcinoma of the maxillary sinus seen on
a bone scan: a case report
O Ait Sahel*, I Ghfir, H Guerrouj, Y Benameur, N Benraiss
Department of Nuclear Medicine, IBN-SINA Hospital Center,University Med V-Rabat, Morocco
CASE REPORT
Abstract
Adenoid cystic carcinoma (ACC), the secondmost common cancer occurring in thesinonasal tract, is an aggressive malignancythat presents itself insidiously and is generallyadvanced when diagnosed. Current treatmentmodalities include surgery and irradiation.Despite advanced successful therapies, thesetumours are notoriously associated withlocoregional recurrences. This report presentsthe original case of a patient with adenoidcystic carcinoma of the maxillary sinus withan unusual clinical course and a thoracicvertebral metastases, with spinal cordcompression revealed by a bone scan,occurring only nine months after stoppingtreatment. The aggressive nature of thetumour and the skull base invasion at the timeof diagnosis probably explains the rapid onsetof this unusual site of metastases.
Key words: Adenoid cystic carcinoma, bonescan, maxillary sinus tumour, radiobiphosphonates, spinal metastases
Introduction
Adenoid cystic carcinoma (ACC) is a raremalignant tumour which represents less than1% of head and neck malignancies, and 10%of salivary gland tumours [1]. ACC mostcommonly occurs in the major and minorsalivary glands of the aerodigestive tract andskin [3]. The ACC are tumours with slow andinsidious growth, often discovered at a latestage and locally evolved. The sinonasallocations of ACC have the worst prognosis.Surgery is often complicated by the importanceof the local extension. Recurrence is commonand late and can occur many years after theinitial treatment [1]. Spinal metastasis of ACCof the maxillary sinus, have only been rarelyreported in the literature. We present a caseof a patient with maxillary sinus carcinoma withvertebral metastases revealed by 99mTc-HMDPbone scan.
Case report
A 45-year-old woman developed ACC of theright maxillary sinus, which was treated bysurgery and radiotherapy. The patientpresented 9 months later with limb weakness,which had progressed moderately over time.Neurological examination revealed para-paresis with preserved tendon reflexes andsensation.
*CorrespondenceOmar Ait SahelNuclear Medicine DepartmentIBN-SINA Hospital CenterUniversity Med V-RabatRabat, MoroccoTel: 0021 26284178Email: [email protected]
www.pjnm.net 2221-0288(201601/01)6:1<48:USMFAA>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 49
99mTc-hydroxyl-methylene diphosphonate(99mTc-HMDP), bone scan revealed increaseduptake of the right maxillary sinus, the rightorbital roof, and also heterogeneous aspect ofC7-T1 vertebral bodies (Figure 1).
SPECT-CT confirmed increased uptake in theright wing of sphenoid bone with cheekbonelysis (Figure 2) together with increased uptake
in C7 &T1 vertebral bodies (Figure 3). Afollow-up MRI of face and neck with andwithout contrast injection, showed two lesions:one in the right maxillary sinus extending tothe pterygopalatine fossa, and the secondaffecting the right wing of sphenoid bone withcheekbone lysis, and orbital and temporal soft-tissues extension (Figure 4). It also shows the
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:48-52
Figure 1 Planar whole-body scan withlocalized image, obtained 3 hours afteradministration of 740 MBq of 99mTc-hydroxyl-methylene diphosphonate (99mTc-HMDP), showing increased uptake in theright maxillary sinus, the right orbital roof,with heterogeneous uptake in the region ofthe C7-T1 vertebral bodies
Figure 2 Figure 2. Axial SPECT-CT scanshowing increased uptake of the maxillarysinus extending to involve the right wing ofsphenoid bone with cheekbone lysis

PJNM 2016, Volume 6, Number 1 50
the presence of a lesion in the T1 vertebralbody, with extension to the anterior paraspinaland epidural soft-tissue (Figure 5), causing acompression of the spinal cord at this level,with infiltration of the adjacent vertebralbodies.
An open surgical biopsy of spinal cord lesionwas carried out with laminectomies from the7th cervical to the 2nd thoracic vertebrae.Histopathological examination revealed ametastasis of the known ACC of the maxillarysinus in the vertebral column. Palliative localradiotherapy with chemotherapy was initiated.The patient died two months after completionof chemotherapy.
Discussion
Malignancies arising from the sinonasal tractare uncommon. Carcinoma of the maxillarysinus comprises 0.2% to 0.5% of all cancers
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:48-52
Figure 3 Axial and sagittal SPECT-CTscan images showing increased uptakein the 7th cervical and 1st thoracic vertebrae
Figure 4 Brain MRI scan showingintracerebral invasion of the adnoid cysticcarcinoma via the right maxillary nerve
Figure 5 Sagittal MRI scan showing thelesion in the first thoracic vertebra withposterior involvement and circumferentialepidural soft -issue mass compressing thespinal cord

PJNM 2016, Volume 6, Number 1 51
of the head and neck [4]. According to Wang[2], squamous cell carcinomas are the mostcommon form of maxillary sinus tumours,followed by adenoid cystic carcinoma andadenocarcinoma. The choice of optimal therapyfor ACC of the head and neck is affected bysite, stage, histologic grade, and biologicbehavior of the ACC. There are a number ofpublications that address the efficiency ofsurgery and radiation therapy in the treatmentof ACC of the head and neck [4-6].
ACC of the head and neck, and specifically ofthe nasal cavity and paranasal sinuses, posesnumerous treatment challenges for severalreasons: it has a high propensity for localinvasion to adjacent structures, makingresection more difficult; it is commonlydiagnosed late due to its insidious growth; andin 50% of cases it has caused perineural spreadat the time of diagnosis [7]. Furthermore, ACCis associated with high rates of distantmetastases, which have been noted to occuras late as 10 years after the diagnosis of theprimary lesion [8]. Clinicians are all too awarethat distant metastases often defeat successfultreatment of patients with ACC, despitelocoregional control, and are associated with alow long-term survival rate.
Histologically, ACC can be categorized into 3growth patterns: cribriform, tubular, and solid.In most studies, a solid growth pattern isassociated with a worse prognosis, caused byadvanced stage and development of distantmetastases [9, 10]. A unique feature of ACCis the propensity for perineural invasion, evenwith early-stage tumours. The tumour isgraded according to Szanto et al. [11] ascribriform or tubular (grade I), less than 30%solid (grade II), or greater than 30% solid(grade III). In our report the histopathologyrevealed a solid subtype. This is probably onefactor contributing to the bad outcome.
The reported incidence of spinal epiduralcompression from head and neck cancer isaround 1% [12], which is much lower than thatof compression by metastasis from breast(20-26%) or lung cancer (12-13%).Compression of the spinal cord or cauda equinaby metastatic disease is almost always
extradural [13]. This condition usually resultsfrom tumour involvement of the vertebralcolumn affecting either a vertebral body or aneuronal arch, as is the case in our patient.According to literature data, only four patientswith carcinoma of the maxillary sinus withspine metastases have been reported: withcompression of the cauda equina in two ofthem. Survival was short (three months) forboth [14,17,18].
The clinical course, in our reported case, wasatypical in terms of its chronology. Thediagnosis of spinal cord metastasis from ACCof the maxillary sinus only nine months aftercompletion of radiotherapy illustrates thehighly aggressive nature of this tumour.Decompression and stabilization of the spinalcord can maintain or improve quality of life.The role of decompression and/or fusion inspinal metastases with neurologic deficits isstill under debate, although recent studieshave confirmed the beneficial role of surgicalintervention in selected patients [15, 16].According to Patchell et al. directdecompressive surgery plus postoperativeradiotherapy seems to be superior to treatmentwith radiotherapy alone for patients with spinalcord compression caused by metastatic cancer[15].
In this reported case, the aggressive nature ofthe tumour and the presence of intracerebralinvasion of the skull base at the time ofdiagnosis probably explains the rapid onset ofthis unusual site of metastasis. The presenceof perineural invasion on the initial histologicalexamination should have been considered tobe a predictive factor of this progression.
Conclusion
Spinal metastases of maxillary sinus ACC areuncommon. Decompression and stabilizationof the spinal cord can maintain or improvequality of life. The clinical behavior of ACC, andits high propensity for local invasion toadjacent structures makes obligatory a periodicexamination throughout life.
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:48-52

PJNM 2016, Volume 6, Number 1 52
References
1. Chummun S, McLean NR, Kelly CG.Adenoid cystic carcinoma of the head andneck. Br J Plast Surg 2001; 54:476-80.
2. Wang JH, Lee JH, Han JH. Contralateralmaxillary sinus lesions in patients withnasal cavity and/or paranasal sinuscarcinoma: analysis of computedtomography findings. Ann Otol RhinolLaryngol 2008; 117(12):909-13.
3. Seab JA, Graham JH. Primary cutaneousadenoid cystic carcinoma. J Am AcadDermatol 1987; 17(1):113-8.
4. Le Q-T, Fu KK, Kaplan M. Treatment ofmaxillary sinus carcinoma. Cancer 1999;86:9.
5. Lupinetti AD, Roberts DB, Williams MD.Sinonasal adenoid cystic carcinoma. Cancer2007; 110:2726 31.
6. Rhee CS, Won TB, Lee CH. Adenoid cysticcarcinoma of the sinonasal tract: treatmentresults. Laryngoscope 2006; 116:982-6.
7. Amit M, Binenbaum Y, Sharma K. "Adenoidcystic carcinoma of the nasal cavity andparanasal sinuses: a metaanalysis,"Journal of Neurological Surgery B, SkullBase, vol. 74,no. 3, pp. 118-125, 2013.
8. Zald PB, Weber SM, Schindler J. Adenoidcystic carcinoma of the subglottic larynx:a case report and review of the literature,Ear, Nose and Throat Journal, vol. 89, no.4, pp. E27-E32, 2010.
9. Matsuba HM, Spector GJ, Thawley SE.Adenoid cystic salivary gland carcinoma: ahistologic review of treatment failurepatterns. Cancer 1986, 57:519-524.
10.Westra WH. The surgical pathology ofsalivary gland neoplasms. Otolaryngol ClinNorth Am 1999, 39:919-943.
11.Szanto PA, Luna MA, Tortoledo ME.Histologic grading of adenoid cysticcarcinoma of the salivary glands. Cancer1984, 54:1062-1069.
12. Ampil F, Nanda A, Aarstad RF, HoasjoeDK, Chin HK, Hardjasudarma M. Spinalepidural compression in head and neckcancer Report of five cases.. Journal ofCranio-Maxillo-Facial Surgery(1994)22;49-52.
13. Stark RJ, Henson RA, Evans SJW. Spinalmetastases, a retrospective survey froma general hospital. Brain 105 (1982)189-203.
14. Ampil FL, Lall C, Willis BK. Maxillary sinuscancer and metastatic compression of thecauda equina: report of two cases. J LaState Med Soc 2001; 153:497-500.
15. Patchell RA, Tibbs PA, Regine WF. Directdecompressive surgical resection in thetreatment of spinal cord compressioncaused by metastatic cancer: arandomised trial. Lancet 2005;366:643-8.
16. Ulmar B, Naumann U, Catalkaya S.Prognosis scores of Tokuhashi andTomita for patients with spinalmetastases of renal cancer. Ann SurgOncol 2007; 14:998-1004.
17. Caillot A, Veyssière A, Ambroise B,Bénateau H. Spinal cord metastasis ofsquamous cell carcinoma of the maxillarysinus. European Annals ofOtorhinolaryngology, Head and Neckdiseases 132 (2015) 97-99.
18. Hopf-Jensen S, Buchalla R, Rubarth O,Peters J, Dunker H, Hensler HM, Müller-Hülsbeck S, Börm W. Unusual spinalmetastases from an adenoid cysticcarcinoma of the maxillary sinus. CaseReports / Journal of Clinical Neuroscience19 (2012) 772-774
Pak J Nucl Med 2016;6:48-52 2221-0288(201601/01)6:1<48:USMFAA>2.0.TX;2-M

PJNM 2016, 6:53-58 331691 © 2016 Pakistan Society of Nuclear Medicine
SPECT/CT imaging of primary mediastinalgoitre: case report and literature review
Imad Ghfir1,*, Abdallah Achir2, Hasnae Guerrouj1, SalahNabih Oueriagli1, Omar Ait Sahel1, N Benraïs Aouad1
Departments of 1Nuclear Medicine and 2Thoracic Surgery, Ibn SinaHospital, Mohammed V University, Rabat, Morocco
CASE REPORT
Abstract
Primary mediastinal goitre (PMG) is an ectopicthyroid in a rare location, even more so whenassociated with an anomaly of the nativethyroid gland. It should be considered in thedifferential diagnosis of all mediastinalmasses.
We report the case of a 74-year-old womanpresenting primary anterior mediastinal goitrewith a toxic multinodular goitrous thyroidgland located in the thyroid bed in the anteriorneck. 99mTc pertechnetate scintigraphy (planarand SPECT/CT) confirmed the uptake of theradiotracer in the mediastinal mass, showingthe mass to be separate from the cervicalthyroid gland, thus confirming an ectopicPMG. A surgical resection of the cervicalmultinodular goitre and the intrathoracic masswas performed. Histopathology showed a
multinodular adenomatous goitre withoutsigns of malignancy. The patient has had anunremarkable postoperative recovery.
99mTc scintigraphy with SPECT-CT imagingseems to be the most important diagnostictool for the detection of ectopic thyroid tissueand shows the absence or presence of thyroidin its normal location. The technique is notonly important for establishing the diagnosis,but crucial in deciding upon the correcttherapeutic strategy, including the surgicalapproach.
Key words: Primary mediastinal goitre, 99mTcscintigraphy, SPECT/CT imaging
Introduction
Primary mediastinal goitre (PMG) or trueectopic mediastinal goitre in presence of amultinodular native thyroid is an exceedinglyrare entity representing less than 1% of allendothoracic tumours with only a few casesreported in the literature [1]. The diagnosismay be difficult and is based on the imagingdata. We present a case of a female witha toxic multinodular goitre located in the
*Correspondence
Dr Imad GHFIRDepartment of Nuclear MedicineIbn Sina hospital, Mohammed V UniversityRabat, MoroccoEmail : [email protected]él: 00212610327734
www.pjnm.net 2221-0288(201601/01)6:1<53:SIOPMG>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 54
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:53-58
anterior neck with a separate large anteriormediastinal ectopic goitre, imaged by hybridSPECT-CT imaging and subsequently treatedsuccessfully with surgical removal. bone scan.
Case report
A 74-year-old woman was admitted withcomplaint of dyspnoea and slight dysphagia.She had a history of hyperthyroidism treatedby antithyroid drugs. Physical examinationrevealed a thyroid goitre. Ultrasonographyof neck was performed which showed amultinodular goitre without any evidence ofretrosternal extension. A chest x-ray (Figure1) revealed marked mediastinal wideningand predominant right with a trachealdeviation. Cervical and thoracic CT scan(Figure 2) showed a multinodular cervicalgoitre, with a large retrosternal mass (12,8x 6,6 x 5,3 cm) with well defined borders,in the upper and middle mediastinumcontaining microcalcifications and showingan enhancement after iodinated contrast
Figure 1 Chest x-ray showing trachealdeviation (red arrow) and markedmediastinal widening with a prominent rightatruim (white arrow)
administration, without signs of infiltration.The appearances were compatible with adiagnosis of thymoma, teratoma or anintrathoracic goitre.
Figure 2 CT scan showing: (a) amultinodular orthotopic goitre (white arrow)and; (b) a large mixed density mass lesionin the anterior mediastinum containingmicrocalcifications showing enhancementafter iodine contrast administration withoutvascular invasion (yellow arrow)
b
a

PJNM 2016, Volume 6, Number 1 55
331691 © 2015 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:53-58
Laboratory tests showed normal thyroidfunction with the patient on anti-thyroidmedications. Anti-thyroperoxidase and anti-thyroglobulin antibodies were absent, withnormal serum calcitonin concentration andnormal βHCG and αFP levels.
Thyroid scintigraphy was carried out 20minutes after an intravenous injection of185 MBq of 99mTc pertechnetate. Imagingwas performed using a dual-headed hybrid(SPECT/CT)gamma camera fitted withparallel-hole, high-resolution low-energycollimators, with 20% energy windowscentered at 140 keV. SPECT/CT images wereobtained according to predeterminedparameters including 64 steps (20sec/step), 360° orbit and reconstruction ina 128 × 128 matrix with a three-dimensional ordered-subset expectationmaximization (OSEM) algorithm. Low-doseCT parameters included 120 kV and 100mAs, and images were reconstructed witha section thickness of 5 mm in a 256 × 256matrix. A CT-based attenuation correctionalgorithm was applied. The acquisition inplanar mode highlighted an intense uptakein the cervical multinodular thyroid gland(Figure 3), with less intense andheterogeneous uptake at the upper andmiddle mediastinal regions but without anycontinuity between the mass and thecervical thyroid gland. SPECT-CTcomplement confirmed the uptake ofradiotracer in the mediastinal mass,attesting the diagnosis of primaryintrathoracic goitre (Figure 4). CT scanguided mediastinal biopsy confirmed themass to be a benign colloid goitre. Themultinodular orthotopic goitre and theintrathoracic mass were completely resectedthrough a cervicotomy and a total mediansternotomy. There were no tissue orvascular connections between the mass andthe cervical thyroid gland. Histopathologyshowed a multinodular adenomatous goitrewithout signs of malignancy. Antithyroiddrugs were replaced by thyroid hormonereplacement therapy and the patient had aremarkable postoperative recovery.
Discussion
Primary mediastinal goitre (PMG) or trueectopic mediastinal goitre is a raredevelopmental abnormality involvingaberrant embryogenesis of the thyroidgland during its passage from the floor ofthe primitive foregut to its final pre-tracheal position [2, 3] . It correspondsto a rare location of ectopic thyroid wherethe intra-thoracic thyroid tissue isindependent of the native cervical thyroidgland. It represents about 0,2 - 1% ofintra-thoracic tumours with a femalepreponderance (female/male ratio: 3). Itis localized primarily in the anteriormediastinum (85% of cases). The middleand posterior mediastinum are lessfrequent locations in 15% of cases [4].
Figure 3 99mTc pertechnetate planarthyroid scan showing intense uptake in theorthotopic multinodular thyroid gland withless intense and heterogeneous uptake inthe upper and middle mediastinum (whitearrow) without continuity with theorthotopic thyroid

PJNM 2016, Volume 6, Number 1 56
331691 © 2015 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:53-58
Most ectopic goitres are asymptomatic at thetime of diagnosis but when they occur, clinicalmanifestations such as dysphagia , dyspnea,superior vena cava syndrome, are mostlyrelated to the compression of adjacent organs5 . Chest pain may be present in case of nervecompression [6]. Also, some cases ofhyperthyroidism have been reported in theliterature including certain forms oflymphocytic thyroiditis or toxic nodular goitresas in the present case [7].
A chest x-ray is the initial investigationshowing mediastinal widening and perhapscompression signs like tracheal deviation [8].
Ultrasound permits excellent characterizationof cervical thyroid tissue, but it is not veryeffective in the evaluation of the PMG [9].
Computed tomography (CT) of the thorax, inaddition to suggesting the thyroid origin of themediastinal mass, often in the form of multi-cystic appearance with calcifications in itsinterior, may show a lack of continuitybetween PMG and the cervical thyroid gland[10].
Magnetic resonance imaging may be useful inmore precisely defining the relationship of thetumour to the adjacent structures. However,
Figure 4 SPECT-CT complement with three orthogonal reconstructed images, confirmingthe uptake of radiotracer in the anterior mediastinal mass, without any continuity with theorthotopic thyroid (white arrows

PJNM 2016, Volume 6, Number 1 57
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:53-58
the definitive diagnosis is made only by meansof histopathological analysis, often achievedonly after removing the tumour. In somecases, biopsies can be obtained successfullyusing CT-guided puncture, as in our patient[11].
Further diagnostic tools are needed fordeciding upon the appropriate management.Scintigraphy can be useful for the differentialdiagnosis of thymoma and teratoma 12 .Indeed, radionuclide scintigraphy using99mTc, 131I, or 123I, is the most importantdiagnostic tool for detecting ectopic thyroidtissue and shows the absence or presence ofthyroid in its normal location. It provides anexcellent estimate of the functional status ofa mediastinal goitre, its nature and extent.Also, it is very useful for confirming adiscontinuity between the mediastinal massand the cervical thyroid gland in the PMG andfor delineating additional sites of thyroidtissue. It is considered the best preoperativeinvestigation as it can be performed quickly,reliably, and with very low radiation exposure[13-16].
Although compared with other radioisotopes131I is the preferred radionuclide for thyroidscintigraphy for imaging an intrathoracic goitredue to its low background activity, wecurrently prefer 99mTc to 131I/123I for severalreasons including its low expense, readyavailability, and the short time betweeninjection and imaging. Radioiodine thyroidimaging, however, is preferred to 99mTc for themanagement and the follow-up of patientswith well differentiated thyroid carcinoma.
Hybrid SPECT/CT combined with planardiagnostic 99mTc scintigraphy allows preciselocalization and accurate characterization offoci of radioactivity in the head, neck andthorax. Equivocal findings on planar imagingmay be clarified on SPECT/CT, withsubsequent changes made to treatment plans[17, 18] as in the present case. The ability tofuse functional data provided by SPECT slicesand morphological images provided by CT,combines physiologic information of onemethod with the superior anatomic resolution
of the other. In many cases, this allows moredefinitive diagnosis than can be obtained bysimple visual comparison of nuclear medicineimages and conventional cross-sectionalimaging [19].
Surgical resection is advocated for relievingcompressive symptoms, and for ruling outthe diagnosis of malignancy [20, 21]. Thespecific surgical modality depends on thegoitre location, size and its relationship toadjacent structures. Secondary intra-thoracicgoitres are usually resected through an inferiorcervical collar incision; nevertheless, extendedmediastinal tumours beyond the aortic archmay require additional extra-cervical incisionsincluding sternotomy, clavicular resection,anterior and posterolateral thoracotomy orvideo-assisted thoracoscopic surgery [22].
Conclusion
PMG is a rare condition, even more so in thepresence of a native multinodular toxic goitre.This case demonstrates the importance ofconsidering an ectopic thyroid in thedifferential diagnosis of mediastinal masses.99mTc scintigraphy with SPECT-CT imaging isnot only helpful in determining the aetiologyof the mediastinal mass but also helps in thetherapeutic strategy including the surgicalapproach. Surgical resection is advocated forrelieving compressive symptoms, and forruling out the presence of malignancy.
References
1. Valgas-Abrego BV, Alvarez-Maldonado P,Alcazar-Lopez RM, Lorente-Ludlow FC,Nunez-Perez RC. Primary MediastinalGoitre Resected via Cervical Approach. IntJ Respir Pulm Med 2015, 2:1.
2. Cherif L, Lakhoua Y, Khiari K, Hadj-Ali I,Rajhi H, Kaffel N, et al. Ectopic thyroid: twocases. Ann Endocrinol 2004; 65 (3) :233-235.
3. Baik SH, Choi JH, Lee HM. Dual ectopicthyroid. Eur Arch Otorhinolaryngol 2002;259 (2): 105-7.

PJNM 2016, Volume 6, Number 1 58
Pak J Nucl Med 2016;6:53-58 2221-0288(201601/01)6:1<53:SIOPMG>2.0.TX;2-M
4. Foroulis CN, Rammos KS, Sileli MN,Papakonstantinou C Primary intrathoracicgoitre: a rare and potentially serious entity.Thyroid 2009; 19: 213-218.
5. Nistor C, Ciuche A, Motas C, Mota? N,Bluoss C, et al. Cervicomediastinal thyroidmasses - our experience. Chirurgia (Bucur)2014: 109: 34-43.
6. Wang J, Fang J. Ectopic thyroid mass in theleft lateral neck and anterior mediastinum:a case report. Journal of Medical CaseReports 2014; 8: 351.
7. Wein RO, Norante JD. Hashimoto'sthyroiditis within ectopic thyroid glandmimicking the presentation of thyroglossalduct cyst. Otolaryngol Head Neck Surg2001; 125: 274-276.
8. Shah BC, Ravichand CS, Juluri S, AgarwalA, Pramesh CS, Mistry RC. Ectopic thyroidcancer. Annals of Thoracic andCardiovascular Surgery 2007; 13: 122-124.
9. Marinovic D, Garel C, Czernichow P, LegerJ. Ultrasonographic assessment of theectopic thyroid tissue in children withcongenital hypothyroidism. PediatricRadiology 2004; 34: 109-113.
10. Kobayashi H, Tashita H, Hara H, HasegawaY. Utility of computed tomography inidentifying an ectopic thyroid in infants andpreschool children. Endocrine Journal 2003;52: 189-19.
11. Mack E. Management of patients withsubsternal goitres. Surg Clin North Am1995; 75:377-94.
12. Noussios G, Anagnostis P, Goulis DG,Lappas D and Natsis K. Ectopic thyroidtissue: anatomical, clinical, and surgicalimplications of a rare entity. EuropeanJournal of Endocrinology 2011; 165: 375-382.
13. Bersaneti JA, Silva RD, Ramos RR,Matsushita Mde M, Souto LR. Ectopicthyroid presenting as a submandibularmass. Head and Neck Pathology 2011;5:63-66.
14. Toso A, Colombani F, Averono G, Aluffi P& Pia F. Lingual thyroid causing dysphagiaand dyspnoea. Case reports and reviewof the literature. ActaOtorhinolaryngologica Italica 2009; 29:213-217.
15. Peters P, Stark P, Essig G Jr, Lorincz B,Bowman J, Tran K, Coman S. Lingualthyroid: an unusual and surgically curablecause of sleep apnoea in a male. Sleepand Breathing 2010; 14: 377-380.
16. Chawla M, Kumar R, Malhotra A. Dualectopic thyroid: case series and review ofthe literature. Clinical Nuclear Medicine;2007: 321- 325.
17. Buck AK, Nekolla S, Ziegler S, et al.SPECT/CT. J Nucl Med 2008; 49 (8):1305-1319.
18. Bockisch A, Freudenberg LS, Schmidt D,Kuwert T. Hybrid imaging by SPECT/CTand PET/CT: proven outcomes in cancerimaging. Semin Nucl Med 2009; 39(4):276-289.
19. Knoll P, Krotla G, Koriska K, Rodriques M,Mirzaei S. SPECT/CT. J Nucl Med 2009;50 (6): 1009-1010.
20. 20. Netterville JL, Coleman SC, Smith JC,Smith MM, Day TA, Burkey BB.Management of substernal goitre.Laryngoscope 1998; 108:1611-17.
21. Houck WV, Kaplan AJ, Reed CE, Cole DJ.Intrathoracic aberrant thyroid:identification critical for appropriateoperative approach. Am Surg 1998;64:360-362.
22. Chen X, Xu H, Ni Y, Sun K, Li W. Completeexcision of a giant thyroid goitre inposterior mediastinum. J CardiothoracSurg 2013; 8: 207.

PJNM 2016, 6:59-62 331691 © 2016 Pakistan Society of Nuclear Medicine
SPECT/CT for the accurate localization of 67Gauptake in mycotic abdominal aortic aneurysm
Nada Almenieir1,*, Hani Hassoun1, Kent MacKenzie2,Vilma Derbekyan1
Divisions of 1Nuclear Medicine and 2Vascular Surgery, Royal VictoriaHospital, 1001 Decarie Boulevard, Montreal, Quebec H4A 3J1, Canada
CASE REPORT
Abstract
We report a case of mycotic abdominal aorticaneurysm where the use of hybrid imagingwith gallium scan demonstrated increaseduptake in the infected aneurysm and aided indifferentiating physiological uptake in thebowel from pathological uptake.
Key words: Gallium-67, SPECT, SPECT/CT,mycotic aortic aneurysm
Introduction
The term 'mycotic aneurysm' has been usedsince the 1800s for infected aneurysmsresulting from bacterial endocarditiscomplicated by septic arterial emboli [1, 3].Wilson et al. classified the infected aneurysmsaccording to their clinical characteristics:
mycotic (endocarditis-related), microbialarteritis, infection of existing aneurysm andpost-traumatic infected false-aneurysm [4].However, the majority of vascular surgeonsnowadays keep to the commonly useddefinition of mycotic aneurysm to include allkind of infected aneurysms.
We report a case of mycotic abdominal aorticaneurysm where the use of hybrid imaging withgallium scan demonstrated increased uptake inthe infected aneurysm and aided indifferentiating physiological uptake in the bowelfrom pathological uptake.
Case report
A 61-year-old male with hypertension and arecent travel history to Cuba presented witha 3 week history of mild but unremittingpain in the lower abdomen and an episode offever and chills 2 weeks prior topresentation. CT angiography of theabdomen was ordered for further evaluationof the pain, which revealed aortitis at thelevel of the infrarenal aorta with apseudoaneurysm and small penetratingulcer (Figure 1). A whole-body gallium-67scan was ordered to assess for infection,
*Correspondence
Dr. Nada Almenieir1001 Decarie BoulevardMontréal, Québec,Canada H4A 3J1Tel: (514) 934-1934 [email protected]
www.pjnm.net 2221-0288(201601/01)6:1<59:SFTALO>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 60
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:59-62
which showed focal accumulation in theaneurysmal sac (Figure 2). The patient wastreated with broad-spectrum antibiotics forone week. A repeat CT of the abdomen was
performed to assess the evolution of theinfection, which showed expansion of theaneurysmal sac (Figure 3).
Figure 1 Contrast-enhanced CT of the abdomen showing a pseudoaneurysm at theanterior right lateral aspect of the infrarenal aorta measuring approximately 0.8 cm. Theaortic lumen is patent and of normal calibre. Computed tomography with contrast is thefirst choice of imaging modalities for the evaluation of vascular and perivascularabnormalities [2]
Figure 2 A whole-body gallium-67 scan and SPECT/CT were acquired on the same dayas the first CT to assess for infection, which showed focal intense increased uptake in theknown pseudoaneurysm sac in the infrarenal abdominal aorta. Gallium-67 planar imagesof the abdomen show physiological activity in the abdomen (left) with the SPECT/CT scan(right) demonstrating increased uptake in the aneurysmal sac (white arrows), which isdistinct from bowel activity (red arrow)

PJNM 2016, Volume 6, Number 1 61
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:59-62
The patient underwent an operative procedureto repair the contained ruptured mycoticaneurysm with neo-aortic in-situ repair withright superficial femoral vein.
Microbiological examination and cultures of theresected aorta grew salmonella species,resistant to trimethoprim and ciprofloxacin,sensitive to ceftriaxone and ampicillin. He wasstarted on Ceftriaxone intravenous antibiotictherapy, and continued for 6 weeks, then wasswitched to oral cefixime for a duration of 6months.
Discussion
Organisms have been isolated fromaneurysmal tissue in up to 76 percent ofpatients with mycotic aneurysms [5].Staphylococcus spp. and Salmonella spp.remain the most common [6, 7]. The diseasedaorta appears to be vulnerable to Salmonella,and this pathogen is frequently isolated ininfected aneurysms due to bacteraemicseeding of atherosclerotic plaque [8].
The role of gallium-67 uptake in infected aortic
aneurysms was previously described [9] onplanar imaging with the aid of 3-phase 99mTc-MDP bone scan. Aneurysms have beenreported as incidental findings on the bloodflow and blood pool images of 99mTc-MDP or99mTc tagged erythrocytes [10, 11]. Infectedaneurysms have been previously described inthe literature with several radiotracers, suchas gallium-67, In-111 tagged leukocytes,99mTc-hexamethylpropylene amine oxime(HMPAO) labelled leukocyte and 18F-FDG.[12-16]. Gallium-67 scan is considered notreliable in the abdomen because ofphysiological bowel activity. In this case,hybrid imaging with SPECT/CT was able todifferentiate physiological gallium-67 uptakein the bowel and pathological uptake in theabdomen and also localized the uptake to theaortic pseudoaneursym, which indicated thepresence of an infected psdudoaneurysm, apotentially life-threatening condition [17].
References
1. Osler w. the Gulstonian lectures onmalignant endocarditis. BMJ 1885; 1: 467.
Figure 3 Follow-up contrast-enhanced CT of the abdomen after one week of broad-spectrum antibiotic therapy showing enlargement in the size of the aorta/aortic wall, withincreased perfusion of the pseudoaneurysm area, which nonetheless remained contained.There were no signs of active inflammatory change beyond the aortic wall or sign ofbleeding into the retroperitoneal space

PJNM 2016, Volume 6, Number 1 62
Pak J Nucl Med 2016;6:59-62 2221-0288(201601/01)6:1<59:SFTALO>2.0.TX;2-M
1. Osler w. the Gulstonian lectures onmalignant endocarditis. BMJ 1885; 1: 467.
2. Azizi L, Henon A, Belkacem A, et al.Infected aortic aneurysms: CT features.Abdom Imaging. 2004;29:716 –720.
3. Lewis D, Schrager J. Embolomycoticaneurysms. JAMA 1808;1909:63.
4. S.E. Wilson, P. Van Wagenen, E. PassaroJr. Arterial infection, Curr Probl Surg, 15(1978), p. 5.
5. Ernst CB, Campbell HC Jr, Daugherty ME,et al. Incidence and significance of intra-operative bacterial cultures duringabdominal aortic aneurysmectomy. AnnSurg 1977; 185:626.
6. Moneta GL, Taylor LM Jr, Yeager RA, etal. Surgical treatment of infected aorticaneurysm. Am J Surg 1998; 175:396.
7. Marques da Silva R, Caugant DA, EribeER, et al. Bacterial diversity in aorticaneurysms determined by 16S ribosomalRNA gene analysis. J Vasc Surg 2006;44:1055.
8. Hsu RB, Tsay YG, Wang SS, Chu SH.Surgical treatment for primary infectedaneurysm of the descending thoracicaorta, abdominal aorta, and iliac arteries.J Vasc Surg 2002; 36:746.
9. Hsu C, Huang Y. et al, Detection of aninfected abdominal aortic aneurysm withthree-phase bone scan and gallium-67scan. Clin Nucl Med. 2008; 33:4.
10. Carson BJ, McEwan AJ, Hoskinson ME, etal. Detection of an abdominal mycoticaneurysm on three-phase bone scan. Acase report. Clin Nucl Med. 1995;20:267–269.
11. Duarte PS, Zhuang H, Aldighieri F, et al.Incidental detection of an abdominalaortic aneurysm during evaluation ofgastrointestinal bleeding with Tc-99m
tagged erythrocytes. Clin Nucl Med.2002;27:824.
12. Chua R, Rees D. Mycotic coronary arteryaneurysm detected by gallium-67scintigraphy. Heart Lung Circ.2004;13:101–105.
13. Ben-Haim S, Seabold JE, Hawes DR, etal. Leukocyte scintigraphy in the diagnosisof mycotic aneurysm. J Nucl Med.1992;33:1486 –1493.
14. Cortes J, Alonso JI, Ruiz-Oliva F, et al.Tc-99m HMPAO-labeled leukocytes in thediagnosis of mycotic aneurysm. Clin NuclMed. 2002;27:817– 818.
15. Vijayakumar V, Shah RK. Role of delayedTc-99m HMPAO labeled leukocytescintigraphy in the diagnosis of coronarymycotic aneurysm. Clin Nucl Med.2005;30:682- 684.
16. Davison JM, Montilla-Soler JL, BroussardE, et al. F-18 FDG PET-CT imaging of amycotic aneurysm. Clin Nucl Med.2005;30:483- 487.
17. Muller BT, Wegener OR, Grabitz K, et al.Mycotic aneurysms of the thoracic andabdominal aorta and iliac arteries:experience with anatomic and extra-anatomic repair in 33 cases. J Vasc Surg.2001;33:106-113.

PJNM 2016, 6:63-68 331691 © 2016 Pakistan Society of Nuclear Medicine
Functional ectopic cystic parathyroid adenomas:case reports and literature review
Nigora Rasulova*, Qaisar Hussain Siraj, Amir Javaid,Anwar Al-Banna
Department of Nuclear Medicine, Farwania Hospital Kuwait
CASE REPORT
Abstract
Parathyroid adenomas are the commonestcause of primary hyperparathyroidism. About10 percent of the parathyroid adenomas areectopic in location. Cystic degeneration inparathyroid adenomas is seen in 4% of thecases and represents 1-2% of the cases withprimary hyperparathyroidism. Hence, thecombination of parathyroid cysts, which areboth ectopic and functional is extremely rare.Functional parathyroid cysts can be either"silent" or associated with a wide range ofclinical symptoms. We present two cases offunctional mediastinal parathyroid cysts, onewith and the other without clinicalmanifestations.
Introduction
Cysts of parathyroid glands occurs in less than0.001% cases of the neck mass [1]. Themajority of parathyroid cysts (PCs) are non-functioning and presents as an asymptomatic
nodule(s) in variable locations extendingfrom the cervical to the mediastinal regions,with 10% of the ectopic PCs located in themediastinum [2].
Parathyroid cysts do not have a specificsonographic appearance [3] and in somecases definitive differentiation of these rarelesions on the basis of sonographicappearance and location alone may not bepossible [4]. Since the ectopic locations arevariable and the results of radiographic andcytologic modalities may lead to confusion, inpatients with hypercalcaemia andhyperthyroidism, dual-phase technetium-99msestamibi (99mTc-MIBI) scan is the method ofchoice for the accurate localization of ectopicfunctional parathyroid cysts. The treatmentof choice is complete surgical removal of thecyst and therefore pre-surgical localization ofthe functional parathyroid cysts by dual-phaseMIBI scan can be extremely helpful to thesurgeon. 99mTc-MIBI parathyroid scintigraphyaccurately localizes the tumour in 90% ofcases and simplifies the surgical management[5].
We present 2 cases with ectopic mediastinalfunctional parathyroid cysts both with andwithout clinical manifestations.
Key words: 99mTc-sestamibi, SPECT/CT,parathyroid adenoma, parathyroid cyst
www.pjnm.net 2221-0288(201601/01)6:1<63:FECPAC>2.0.TX;2-M
*Correspondence
Dr. Nigora RasulovaNuclear Medicine DepartmentFarwania HospitalPO Box 18373Kuwait 81004Email: [email protected]

PJNM 2016, Volume 6, Number 1 64
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:63-68
Case 1
A 46-year-old lady presented in theemergency department with severe abdominalpain associated with vomiting and fever. Adiagnosis of acute pancreatitis was establishedand the patient managed conservatively. Herroutine laboratory results raised WBC countsand raised CRP, and also showed high serumcalcium 4.14 mmol/L (normal range: 2.2-2.6).Serum parathormone (PTH) level was raisedat 25.1 pmol/L (normal range: 1-7.5). Chestx-ray showed a mass in the right mediastinum(Figure 1). Contrast-enhanced CT (Figure 2)showed a fairly well-defined cystic lesion in theright paratracheal region measuring5.5x4.0x3.7 cm with marginal enhancementand fine internal septations .
The patient's MIBI parathyroid scan (Figure 3)showed a large doughnut-shaped lesion in theright upper mediastinum characterized byincreased uptake at the periphery, which wasseen to correspond to the lesion seen on CT.Pre-surgical serial PTH levels showed a risingpattern with the highest value of 125.40pmol/L. A diagnosis of bronchogenic cyst wasmade and video-assisted thoracoscopicsurgery performed. Excision biopsy of thelesion confirmed parathyroid adenoma. PTHlevel fell to 38.3 following surgery. A repeatdual-phase MIBI scan was negative (Figure 4).
Figure 1 Chest x-ray of Case 1
Figure 2 Contrast-enhanced CT scanshowing the mediastinal cyst
Figure 3 Early (left) and late (right)baseline 99mTc-MIBI scans showing adoughnut-shaped mediastinal lesion
Figure 3 Early (left) and delayed (right)postoperative 99mTc-MIBI scan showingnormal uptake

PJNM 2016, Volume 6, Number 1 65
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:63-68
Case 2
A 16-year-old male was found to behypercalcaemic with a corrected serumcalcium of 4.14 mmol/L (normal range: 2.2-2.6). Serum parathormone (PHT) level wassubsequently also found to be raised at 50pmol/L (normal range: 1-7.5). Chest X-rayshowed mediastinal widening and a right sidedshadow suggesting a tumour (Figure 5).
The contrast CT showed a multicystic masslesion in the mediastinum measuring 6x5x7cm located between the sternum and the greatvessels, with well-defined low-attenuation fluiddensity areas and tiny foci of fat densitysuggesting a thymic neoplasm (Figure 6).
The patient's planar 99mTc-MIBI scan imagesshowed a large eccentric rim of increaseduptake, with the SPECT/CT scan (Figure 7)showing central photopaenia with increaseduptake in periphery corresponding to themulticystic mass on the CT component (Figure8).
Discussion
Only about 10% parathyroid cysts (PCs) arereported to be functional associated withhypercalcaemia and primary hyper-parathyroidism which can manifest as fatigue,
Figure 5 Chest x-ray showing mediastinalwidening
Figure 6 Contrast-enhanced CT scanshowing a mediastinal mass
Figure 3 Early (left) and delayed (right)postoperative 99mTc-MIBI scan showing
Figure 7 Planar early (left) and late (right)MIBI scan showing a half doughnut lesionin the mediastinum
Figure 8 Fused SPEC/CT scan showing aperipheral rim of increased MIBI uptake in

PJNM 2016, Volume 6, Number 1 66
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:63-68
weakness, polydepsia, polyuria, depression,nephrolithiasis, osteoporosis, peptic ulcerdisease, abdominal pain, in some casesresulting to parathyroid crisis [6, 7].
These so-called functional parathyroid cystsare in essence parathyroid adenomas withsecondary cystic changes within the adenoma.The non-functional parathyroid cysts are notassociated with increased serum calcium andPTH levels but are identified by a raised levelof PTH in the cystic fluid [8]. These functionalPCs have reported to present as parathryroidcrises [A, B]. There are only a few publishedcase reports on this entity in the radiologyliterature [6, 7].
The heterogeneous clinical presentation of PCsis determined by their hormonal activity, sizeand location. The clinical manifestation ofdisease in case 1 was acute pancreatitis. Acutepancreatitis secondary to hypercalcemia is anuncommon presentation of primary hyper-parathyroidism and has been reported in 1-8%of cases [10-13]. Previous publications aboutacute pancreatitis induced by primaryhyperparathyroidism suggest that therelationship between the two clinical conditionsis not incidental [14-21]. Hypercalcaemiainduces pancreatic injury via a secretory block,accumulation of secretory proteins, andpossibly activation of proteases [22]. In casesof metabolic pancreatitis, in addition tostandard routine management of pancreatitis,a careful monitoring of metabolicabnormalities is crucial due to the dangerrecurrent bouts of acute pancreatitis whichmay be life threatening [23]. Increased levelsof serum calcium documented in a patientpresenting with an episode of acutepancreatitis should raise the suspicion ofprimary hyperparathyroidism [24].
In Case 2 patient, who was clinicallyasymptomatic, routine pre-operativescreening x-ray showed mediastinal wideningwith routine biochemical testing showingincidentally raised serum PTH and calciumlevels. CT examination however wassuggestive of a possible thymic neoplasm, Thepresence of parathyroid and thymic tissue inthe same locations may be explained on
embryological basis as thymus and inferiorparathyroids both usually develop from thethird pharyngeal pouch with the inferiorparathyroids separating from the thymic tissuebut remaining close to lower pole of thethyroid, whereas the thymus descends intothe mediastinum. During thymic migration,small fragments of thymus may separate andattach themselves to any site along this route,with the parathyroid tissue either close to orembedded within the thymus as a result oftheir common origin and path of descent [25].
Functional hybrid imagine technique such aSPECT/CT with 99mTc sestamibi of the neck andchest allows accurate preoperative localizationof ectopic parathyroid adenomas, both cysticand non-cystic [26]. In our cases Tc99mSestamibi SPECT/CT scan showed increasedtracer uptake in periphery with photopenicdefects at the centre confirmed by the CTcomponent. In both cases 99mTc-sestamibiSPECT/CT was more specific than x-ray andCT scan.
Conclusion
Functional mediastinal parathyroid cysts arean extremely rare cause of primaryhyperparathyroidism, which in our opinion canonly be diagnosed correctly in vivo byfunctional radionuclide imaging. The dual-phase MIBI parathyroid scintigraphictechnique is valuable not only in pre-surgicallocalization but also helps in the differentialdiagnosis.
References
1. Asghar A, Ikram M, Islam N. A case report:Giant cystic parathyroid adenomapresenting with parathyroid crisis afterVitamin D replacement. BMC EndocrDisord 2012;12:14.
2. Danielle A. da Silva, Márcia C. Machado,Lúpercio L. Brito1, Renato A et al.Parathyroid cysts: diagnosis andtreatment. Rev Bras Otorrinolaringol.2004;70(6):840-4.

PJNM 2016, Volume 6, Number 1 67
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:63-68
3. Halenka M, Frysak Z, Koranda P, KucerovaL. Cystic parathyroid adenoma within amultinodular goiter: A rare cause ofprimary hyperparathyroidism. J ClinUltrasound 2008;36:243-246 10.
4. Som PM, Sacher M, Lanzieri CF, et al. PParenchymal cysts of the lower neck.Radiology 1985 157 399-406.
5. Muthukrishnan J, Verma A, Modi D,Kumaresan K, Jha S. Ectopic parathyroidadenoma - the hidden culprit. JAPI2007;55:515-518.
6. Senthilkumar Krishnasamy, Probal Moulik& Andrew Macleod. Ectopic parathyroidcyst presenting with parathyroid crisis.Endocrine Abstracts, 2012;28:82.
7. Shields TW, Immerman SC. Mediastinalparathyroid cysts revisited. Ann ThoracSurg. 1999;67(2):581-90.
8. Pontikides N, Karras S, et al. Diagnosticand therapeutic review of cysticparathyroid lesions. Hormones (Athens).2012;11(4):410-8.
9. Nathan A. Johnson, Linwah Yip andMitchell E. Tublin. Cystic ParathyroidAdenoma: Sonographic Features andCorrelation With 99mTc-Sestamibi SPECTFindings. AJR 2010;195:1385-1390.
10. Agarwal A, George RK, Gupta SK, MishraSK: Pancreatitis in patients with primaryhyperparathyroidism. Indian JGastroenterol, 2003;22:224-225.
11. Carnaille B, Oudar C, Pattou F,Combamale F, Rocha J, Proye C:Pancreatitis and primaryhyperparathyroidism: forty cases. Aust NZ J Surg 1998,68:117-119.
12. Shepherd JJ. Hyperparathyroidismpresenting as pancreatitis or complicatedby postoperative pancreatitis. Aust N Z JSurg 1996;66:85-87.
13. Koppelberg T, Bartsch D, Printz H, Hasse
C, Rothmund M. Pancreatitis in primaryhyperparathyroidism (pHPT) is acomplication of advanced pHPT. DtschMed Wochenschr, 1994;119:719-724.
14. Husova L, Senkyrik M, Lata J, Hrbkova V,Husa P, Dolina J, Podral M, OurednicekP. Acute pancreatitis as the road todiagnosis of primaryhyperparathyroidism. Vnitr Lek,2000;46:724-727.
15. Boneschi M, Erba M, Beretta L, Miani S,Bortolani EM. Primaryhyperparathyroidism and acutepancreatitis. A rare clinical association.Minerva Chir, 1999;54:451-454.
16. Shimizu H, Kodama A. Hypercalcemia andpancreatitis as a first symptom of primaryhyperparathyroidism adenoma: a casereport. J Laryngol Otol, 1996;110:602-603.
17. Nieves-Rivera F, Gonzalez-Pijem L.Primary hyperparathyroidism: an unusualcause of pancreatitis in adolescence. P RHealth Sci J, 1995;14:233-236.
18. Ginn DR, Gate J, Tootle K, Salazar S,Watson S. Parathyroid adenomamanifested as pancreatitis and polyuria.South Med J, 1991;61:396-398.
19. Maddern GJ, Fielding GA, Knaus JP, ZinngE, Blumgart LH. A case of severepancreatitis with parathyroid adenoma.Aust N Z J Surg, 1991;84:1023-1025.
20. Abdullah M. Pancreatitis in primaryhyperparathyroidism. Med J Malaysia,2003;58:600-603.
21. Meldahl I, Ljungstrom KG, Wickerts CJ,Von Sigers K. Fulminant acutepancreatitis caused by a largeparathyroid adenomaHyperparathyroidism was diagnosed after5 years. Lakartidningen, 1999;26:2603-2606.
22. Frick TW, Mithöfer K, Fernández-del

PJNM 2016, Volume 6, Number 1 68
Pak J Nucl Med 2016;6:63-68 2221-0288(201601/01)6:1<63:FECPAC>2.0.TX;2-M
Castillo C. Hypercalcemia causes acutepancreatitis by pancreatic secretory block,intracellular zymogen accumulation, andacinar cell injury. Am J Surg. 1995Jan;169(1):167-72
23. Kota SK, Krishna S, Lakhtakia S, Modi KD.Metabolic pancreatitis: Etiopathogenesisand management. Indian J Endocr Metab2013;17:799-805.
24. Christophoros N Foroulis, SotiriosRousogiannis, Christos Lioupis et al.Ectopic paraesophageal mediastinalparathyroid adenoma, a rare cause ofacute pancreatitis. World Journal ofSurgical Oncology, 2004;2:41.
25. Gayatri P, Sanjay D, Ajay N, Amrut A.Mixed multilocular ectopic thymic cystwith parathyroid element presenting asneck mass. Ann Acad Med Singapore,2012;41(6):271-2.
26. Haber RS1, Kim CK, Inabnet WB.Ultrasonography for preoperativelocalization of enlarged parathyroidglands in primary hyperparathyroidism:comparison with (99m)technetiumsestamibi scintigraphy. Clin Endocrinol(Oxf), 2002;57(2):241-9.

PJNM 2016, 6:69-71 331691 © 2016 Pakistan Society of Nuclear Medicine
Pulmonary arteriovenous malformationdiagnosed on a 18F-fluorodeoxyglucose
PET/CT scanKhattab Khaled*, Amir Javaid, Qaisar Hussain Siraj
Department of Nuclear Medicine, Farwania Hospital Kuwait
IMAGING GAMUT
Key words: AV malformation, PET/CT scan
Background A 68-year-old female withknown gastric cancer in 2011 had a routinefollow-up CT scan in Nov 2016, which showeda pulmonary nodule in the right lung. Thepatient was referred to the nuclear medicinedepartment for an 18FDG-PET scan toinvestigate the nature of the lesion.
Procedure 18F-flourodeoxyglucose (277 MBq)was injected intravenously and PET/CT imagingperformed after 60 minutes. PET, CT and fusedimages were reconstructed in the transaxial,coronal and sagittal axes (Figure 1).
Findings The PET-CT scan showed ahypermetabolic lesion in the lateral segmentof the lower lobe of the right lung with SUVmax
of 4.3 (Figure 1a). This mass-like lesion wasseen to be interposed between the rightinferior pulmonary vein and branches of theright interlobar artery (Figure 1b) with the CT
appearance of fingers-in-a-glove, a sign inkeeping with a pulmonary arteriovenousmalformation (AVM). This was seen tocorrespond to the hypermetabolic lesion(Figure 1c). The scan was otherwise normal.
Conclusion The PET/CT scan findings wereconsistent with a hypermetabolic right lung masssuspicious of an AVM. A contrast-enhanced CTconfirmed this impression (Figure 2).
Comments Pulmonary AVM is a rarecongenital anomaly with uncertain aetiology[1]. Since the patients are usuallyasymptomatic and an undiagnosed AVM maybe associated with serious complications [2]it is important to make an early diagnosis forinstituting correct and timely treatment.
In a patient with known previous gastriccarcinoma, an FDG-avid mass-like lesion couldhave raised the possibility of malignancy andmay have resulted in misdiagnosis leading tofurther unnecessary bronchoscopic biopsy.There are however several benign conditionswhich show increased FDG avidity. A literaturesearch revealed a previous report of a patientwith AVM showing increased FDG uptake [3].
This case underscores the importance ofcareful evaluation of both the CT and the PETimages taking into consideration the entire
*Correspondence
Khattab KhaledNuclear Medicine DepartmentFarwania HospitalPO Box 18373Kuwait 81004Email: [email protected]
www.pjnm.net 2221-0288(201601/01)6:1<69:PAMDOA>2.0.TX;2-M

PJNM 2016, Volume 6, Number 1 70
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:69-71
Figure 1 PET-CT scan showing PET image (left row), the CT image (middle row), and thefused image (right row) in the transaxial (a), coronal (b) and sagittal (c) axes. The PETcomponent shows an FDG-avid (SUVmax 4.3) nodule in the lower lobe of the right lung.The CT component shows a mass-like para-hilar lesion in the lateral segment of the rightlower lobe of the lung. The fused images shows the focal increased FDG uptake tocorrespond to the mass-like lesion
b
c
a

PJNM 2016, Volume 6, Number 1 71
Pak J Nucl Med 2016;6:69-71 2221-0288(201601/01)6:1<69:PAMDOA>2.0.TX;2-M
gamut of the reported benign pulmonarypathologies, which may show increased 18F-flourodeoxyglucose uptake to avoid making amisdiagnosis.
References
1. Gossage JR, Kanj G. Pulmonaryarteriovenous malformations: a state ofthe art review. Am J Respir Crit Care Med1998; 158: 643-61.
2. Sood N, Sood N, Dhawan V. Pulmonaryarterioveneous malformation (AVM)causing hemothorax in a pregnant womanrequiring emergent cesarean delivery.Pulm Med 2011; 2011: 865195.
3. Elboga U, Kalender E, Çelen ZY, Yilmaz M,Aktolun C. Pulmonary arteriovenousmalformation mimicking a pulmonarytumour on 18F-fluorodeoxyglucosepositron-emission tomography/computedtomograph. Arch Med Sci 2015; 11, 2:461–462.
Figure 2 Axial section of the contrast-enhanced CT of the chest showing vascularenhancement in the well circumscribedmass-like lesion

PJNM 2016, 6:72-74 331691 © 2016 Pakistan Society of Nuclear Medicine
Multifocal osteomyelitis on bone scan performedfor mandibular mass with uncertain malignancy
Salah Oueriagli Nabih*, Hassna El Guerrouj, Imad Ghfir,Nouzha Ben Raïs
Department of Nuclear Medicine, IBN-SINA Hospital Center,University Med V-Rabat, Morocco
IMAGING GAMUT
Key words: Osteomyelitis, Bone scan
Background A 10-years-old boy presentedwith a mandibular mass and pain in the rightleg. The patient had a suffered from a benignmandibular tumour, an ameloblastoma, whichis a rare disorder of the jaw involvingabnormal tissue growth. MRI centered on theright inferior member showed osteomyelitis inthe right lower extremity involving the femoraldiaphysis with a subperiosteal abscess. Bonescan with radiobiphosphonates was performedto investigate the possibility of bonemetastases and to confirm the presence ofmusculoskeletal infection [1].
Procedure The Planar whole-body bone scanwas performed in the anterior and posteriorprojections 3 hours after an injection of99mTc-hydroxymethylene diphosphonate.Single-photon emission computed tomogra-phy (SPECT-CT) was additionally performed
to investigate the nature of the hot-spotsdocumented on the whole-body bone scan.
*Correspondence
Salah Oueriagli NabihNuclear Medicine DepartmentIBN-SINA Hospital CenterUniversity Med V-RabatRabat, MoroccoTel: 0021 26284178Email: [email protected]
www.pjnm.net 2221-0288(201601/01)6:1<72:MOOBSP>2.0.TX;2-M
Figure 1 Whole-body bone scan showingmultifocal osteomyelitis of the lower third ofthe left forearm, the right and the leftfemoral diaphyses (black arrows). Note theintense uptake in the right mandible relatedto the mandibular mass with uncertainmalignancy (red arrow)

PJNM 2016, Volume 6, Number 1 73
Findings The whole-body bone scan imagesshowed intense uptake in the right mandibularmass at the site of the known tumour (Figure1). The bone scan additionally showed a lineararea of intense uptake involving the medialcortex of the middle one-thirds of the leftfemoral shaft with a similar but smaller lesionseen at the junction of the middle and thelower thirds of the right femoral shaftmedially. There was a also a fusiform focus ofincreased activity seen two-thirds down theleft ulnar shaft (Figure 1). These lesions wereconfirmed as multifocal osteomyelitis on theSPECT-CT scan, which showed subperiostealabscesses in these locations (Figure 2).
Conclusion The bone scan findings wereconsistent with multifocal osteomyelitis, of thelower third of the left forearm, the right and the leftfemoral diaphyseal with subperiosteal abscesses.SPECT-CT has also eliminated septic arthritisand possibility of fractures. These diagnoseswere confirmed by MRI acquisition centered onthe two femoral diaphyseal (Figure 3). Thepatient was taken for incision and drainage andwas also treated with intravenous antibiotics.
The histologically confirmed mandibular mass,an ameloblastoma, also required surgicaltreatment (Figure 4).
Comments 3-phase bone scintigraphy withradiobiphosphonates is particularlyrecommended for the diagnosis of multifocalosteomyelitis and septic arthritis [2]. Hybridimaging (SPECT-CT) is useful in confirmingthe clinical diagnosis of osteomyelitis and also
Figure 2 (A) SPECT / CT centered on theleft femoral diaphysis in transaxial sectionsshowing intense uptake related toosteomyelitis with subperiosteal abscess.(B) SPECT / CT centered on of the leftforearm showing uptake in the left ulnarelated to another focus of osteomyelitiswith subperiosteal abscess
Figure 3 MRI image in axial sectionshowing the bilateral diaphysealosteomyelitis of the two femora withhypertintense subperiosteal abscesses
Figure 4 Histological section from the rightmandibular biopsy showing, on ahaemorrhagic and inflammatory background, a vascularized loose fibroblastappearance of tumour proliferation withatypical lobular provision cubic coating(appearances compatible with mandibularameloblastoma
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:72-74

PJNM 2016, Volume 6, Number 1 74
Pak J Nucl Med 2016;6:72-74 2221-0288(201601/01)6:1<72:MOOBSP>2.0.TX;2-M
provides essential information on the site andextent of the infection, which helps theclinician in planning medical and surgicaltreatment [3].
References
1. Riise OR, Kirkhus E, Handeland KS, FlatoB, Reiseter T, Cvancarova M, Nakstad B,Wathne KO. Childhood osteomyelitisincidence and differentiation from otheracute onset musculoskeletal features in apopulation based study. BMC Pediatrics2008; 8:45.
2. Giedion A, Holthusen W, Masel LF, VischerD. Subacute and chronic "symmetrical"osteomyelitis. Ann Radiol 1972; 15:329-42.
3. Sia IG, Berbari EF. Osteomyelitis. BestPract Res Clin Rheumatol 2006; 20:10651081.

PJNM 2016, 6:75-78 331691 © 2016 Pakistan Society of Nuclear Medicine
Unsuspected chronic multifocal osteomyelitisdiagnosed on a whole-body
18F-FDG PET/CT scanQaisar Hussain Siraj*, Amir Javaid, Khattab Khaled,
Anwar Al-Banna
Department of Nuclear Medicine, Farwania Hospital Kuwait
IMAGING GAMUT
Key words: Osteomyelitis, PET/CT, 18F-flourodeoxyglucose
Background A 24-year-old male with prunebelly syndrome suffering from end-stage renaldisease for which he was undergoing routinehaemodialysis reported with a 2-week historyof swelling of the left knee associated withfever. Blood culture revealed gram +ve cocci(s. aureus). The patient was referred to thenuclear medicine department to investigatethe possibility of septic arthritis of the leftknee and to rule out any osteomyelitis.
Procedure 18F-flourodeoxyglucose (245 MBq)was injected intravenously and PET/CT imagingperformed after 60 minutes. PET, CT and fusedimages were reconstructed in the transaxial,coronal and sagittal axes.
Findings The whole-body PET/CT scanimages (Figure 1) showed mild increasedsoft-tissue uptake (SUVmax 2.4) above and at
*Correspondence
Qaisar Hussain SirajNuclear Medicine DepartmentFarwania HospitalPO Box 18373Kuwait 81004Email: [email protected]
www.pjnm.net 2221-0288(201601/01)6:1<75:UCMODA>2.0.TX;2-M
Figure 1 PET whole-body MIP scan image

PJNM 2016, Volume 6, Number 1 76
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:75-78
the lateral aspect of the left knee withoutevidence of any increased bone uptake seento suggest local osteomyelitis (Figure 2).
The whole-body PET/CT scan imagesadditionally showed focal increased uptake(SUVmax 3.8) in the right 3rd rib anterolaterallywith the CT component showing fusiform localexpansion of the rib and cortical disruption(Figure 3).
There was intense focal FDG uptake (SUVmax
8.2) in the left pelvis corresponding to theleft pubic body, the inferior pubic ramusand the adjacent ischium, with the CTcomponent showing medullary expansionand cortical destruction (Figure 4).
A focus of intense uptake (SUVmax 6.0) wasseen in the right distal fibula with the CTcomponent showing medullary expansion,bone destruction and fracture at this site(Figure 5).
Figure 2 PET/CT scan with the CT (left), PET (middle) and the fused CT & PET (right)images showing heterogenously increased soft-tissue uptake (SUVmax 2.4) in thesymptomatic left knee (arrows) without bone involvement consistent with soft-tissueinfection/inflammation with bilateral arthritic changes seen in the knee joints (chevrons)
Figure 3 PET/CT scan with the CT (left), PET (middle) and the fused CT & PET (right)images showing focal increased uptake (SUVmax 3.8) in the right 3rd rib laterally with theCT component showing fusiform local expansion of the rib and cortical disruption (arrows)

PJNM 2016, Volume 6, Number 1 77
331691 © 2016 Pakistan Society of Nuclear Medicine Pak J Nucl Med 2016;6:75-78
Figure 4 PET/CT scan with the CT (left), PET (middle) and the fused CT & PET (right)images showing intense focal FDG uptake (SUVmax 8.2) in the left pelvis corresponding tothe left pubic body, the inferior pubic ramus and the adjacent ischium, with the CTcomponent showing medullary expansion and cortical destruction
Figure 5 PET/CT scan with the CT (left), PET (middle) and the fused CT & PET (right)images showing intense focal FDG uptake (SUVmax 6) intense focal increased uptake in thedistal right distal fibula with the CT component showing medullary expansion, bonedestruction and fracture at this site

PJNM 2016, Volume 6, Number 1 78
Pak J Nucl Med 2016;6:75-78 2221-0288(201601/01)6:1<75:UCMODA>2.0.TX;2-M
Conclusion The PET/CT findings wereconsistent with soft-tissue infection/inflammation in the symptomatic left kneeregion. However, the other multiplehypermetabolic osseous bone lesionsdocumented on the PET/CT scan seeninvolving the right 3rd rib, in the left pelvisand the right fibula, were consistent withchronic polyostotic osteomyelitis.
Comments Positron emission tomography/computed tomography (PET/CT) with theglucose analogue, 18F-fluoro-2-deoxyglucose(18F-FDG), has an established role inoncological imaging but is being increasinglyused for the diagnosis of musculoskeletalinfection. The accumulation of FDG at sites ofinfection/inflammation is due to its uptake bythe activated granulocytes, which use glucoseas an energy source. Inside the cells, the FDGis phosphorylated by hexokinase to 18F-fluoro-2-deoxyglucose-6-phosphate, which is notfurther metabolized. Increased cellularmetabolism in the activated inflammatory cellsresults in an increased expression of glucosetransporter (GLUT) proteins by these cells,which coupled with an increase in the affinityfor glucose by the glucose transporterssecondary to the effects of cytokines andgrowth factors results in high FDG uptake atsites of infection/inflammation [1]. FDG-PETimaging is particularly useful for diagnosingchronic and low-grade infection because of thehigh uptake of FDG in activated macrophages,the predominant cell type present in chronicinfection [1].
The sensitivity and specificity of FDG-PET fordiagnosing chronic osteomyelitis is reportedat 100% and 92%, respectively by Guhlmannet al. [2], with de Winter et al. [3] reportinga sensitivity, specificity, and accuracy of100%, 88%, and 93% respectively. Zhuanget al. [4] reported similar results.
The superior imaging characteristics and theshorter imaging time span of positron imagingcoupled with its higher spatial resolutioncompared to conventional nuclear medicineinfection imaging techniques such as labelledwhite cells or the gallium scanning, is a distinct
advantage. Also, the combination of functionaland morphological imaging provided by thehybrid techniques is evidently superior toeither the structural imaging modalities suchas the CT or MRI or the conventional nuclearmedicine imaging of infection alone. ThePET/CT technique not only proved highlysensitive in confirming the soft-tissueinfection/inflammation in the region of theleft knee and excluding the presence of localosteomyelitis, but also additionally identifiedpreviously unsuspected multifocalosteomyelitis. The presence of concomitantstructural changes also proved very specificin establishing the chronic nature of theosteomyelitis.
References
1. A. Signore, Glaudemans AWJM. Themolecular imaging approach to imageinfections and inflammation by nuclearmedicine techniques. Annals of NuclearMedicine, 2011;25(10):681–700.
2. Guhlmann A, Brecht-Krauss D, Suger G, etal. Chronic osteomyelitis: detection withFDG/PET and correlation withhistopathologic findings. Radiology,1998;206:749-754.
3. de Winter F, van de Wiele C, Vogelaers D,et al. Fluorine-18 fluorodeoxyglucosepositron emission tomography: a highlyaccurate imaging modality for thediagnosis of chronic musculoskeletalinfections. J Bone Joint Surg Am, 2001;83-A:651-660.
4. Zhuang H, Duarte PS, Pourdehand M, etal. Excusion of chronic osteomyelitis withF-18 fluorodeoxyglucose positron emissiontomographic imaging. Clin Nucl Med, 2000;25:281-284.

EDITORIALWhither Nuclear Medicine Training in Pakistan?Durr-e-Sabih
1
ORIGINAL ARTICLESEstimation of time for release of patients after the administration of I-131 tothyrotoxicosis patientsMuhammad Muhammad Akhtar*, Jawad Akhtar Hussain, Akbar Ali, Sheraz Akhtar
3
Lactate dehydrogenase (LDH) as predictive factor of the pain free syndrome durationafter radionuclide treatment of bone metastases in patients with breast cancerNigora Rasulova, Dauranbek Arybzhanov, Vladimir Lyubshin, Abdulla Abdikhakimov, ShamsutdinSagdullaev, Sherzod Nishonov, Gayrat Arifhodjaev,Yuliya Shakirova, Valery Krylov, MaratKhodjibekov
11
Assessment of renal parenchymal damage by DMSA after PCNL procedure in childrenusing adult-sized equipmentMohammad Sohaib, Manoj U Shenoy, Michael J Kellett, Patrick G Duffy, Isky Gordon
19
Vitamin B12 deficiency: prevalence and evaluation of a reversible co-morbidity inhypothyroid patientsAniqa Jabeen, Sumaira Mushtaq, Hassan Raza, Mohammd Ali Memon
25
Validation of Ottawa ankle rule utilizing radionuclide skeletal scintigraphyShagufta Zafar Qureshi, Fida Hussain Shah, Mohammad Amin Waqar
32
CASE REPORTSRadiosynoviorthesis in pigmented villonodular synovitis using rhenium-188 labelled tincolloid: a case reportAakif U Khan, Hameedullah, Abdul Saeed Shah, Muhammad Rauf Khattak
42
Unusual spinal metastases from an adenoid cystic carcinoma of the maxillary sinus seenon a bone scan: a case reportO Ait Sahel, I Ghfir, H Guerrouj, Y Benameur, N Benraiss
48
SPECT/CT imaging of primary mediastinal goitre: case report and literature reviewImad Ghfir, Abdallah Achir, Hasnae Guerrouj, Salah Nabih Oueriagli, Omar Ait Sahel, N Benraïs Aouad
53
SPECT/CT for the accurate localization of 67Ga uptake in mycotic abdominal aorticaneurysmNada Almenieir, Hani Hassoun, Kent MacKenzie, Vilma Derbekyan
59
Functional ectopic cystic parathyroid adenomas: case reports and literature reviewNigora Rasulova, Qaisar Hussain Siraj, Amir Javaid, Anwar Al-Banna
63
IMAGING GAMUTSPulmonary arteriovenous malformation diagnosed on a 18F-fluorodeoxyglucose PET/CTscanKhattab Khaled, Amir Javaid, Qaisar Hussain Siraj
69
Multifocal osteomyelitis on bone scan performed for mandibular mass with uncertainmalignancySalah Oueriagli Nabih, Hassna El Guerrouj, Imad Ghfir, Nouzha Ben Raïs
72
Unsuspected chronic multifocal osteomyelitis diagnosed on a whole-body 18F-FDG PET/CTscanQaisar Hussain Siraj, Amir Javaid, Khattab Khaled, Anwar Al-Banna
75