Gastro Rounds
-
Upload
phoebecasenasbacalso -
Category
Documents
-
view
223 -
download
1
description
Transcript of Gastro Rounds

GENERAL DATAA.C.,66/f, married, Filipino, Housewife, Roman Catholic, born on November 19, 1948, Currently residing in Sitio Chicos Labogon, Mandaue City. Admitted for the first time in CDUH.

CHIEF COMPLAINT
JAUNDICE

HISTORY OF PRESENT ILLNESS 2 months PTA, patient had onset of
generalized skin pruritus (Condition tolerated) which was alleviated with warm compress. Patient also noted that her urine was dark orange in color. No dysuria noted, no flank pain, condition tolerated.

HISTORY OF PRESENT ILLNESS 5 months PTA, patient sought consult to
a private physician. Patient was prescribed with Cetirizine 10mg once daily HS for 7 days and Cloxacillin three times a day for 7 days with compliance. However, there was no relief of the condition.

HISTORY OF PRESENT ILLNESS 3 weeks PTA, condition persisted now
with generalized jaundice noted. Patient also noted that her stool was pale and creamy in color. Patient then sought consult for the second time and was given an unrecalled antihistamine and was advised for ultrasound. Patient has no other associated sign and symptom. No fever, no abdominal pain, no body malaise.

HISTORY OF PRESENT ILLNESS About 2 weeks PTA, patient sought consult to
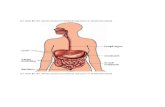
a gastroenterologist with the ultrasound result. Ultrasound revealed slightly dilated intrahepatic duct and distal common bile duct obstruction with gallbladder bile sludge. Blood chemistry also showed Increased ALT and AST, Alkaline Phosphatase was also increased, Total, direct and indirect bilirubin was also increased, Gamma glutamyl transferase was also increased.

HISTORY OF PRESENT ILLNESS Patient was then ordered CBC, CT scan,
Creatinine and TSH. Patient was then prescribed with Ofloxacin 400mg tablet taken twice a day for 7 days and Hyosine N-Butylbromide 10mg tablet taken three times a day for 2 days.

HISTORY OF PRESENT ILLNESS 2 days PTA, patient sought consult to an
Endocrinologist for her thyroid evaluation prior to CT scan but was then advised for admission.

PAST MEDICAL HISTORY Patient has a history of hypertension for
10 years. Her usual BP 120-140 systolic, 80-90 diastolic. Patient was also diagnosed with Diabeted milletus this year.
Patient have no known history of allergies.
Patient was diagnosed with PTB (1970s) and has completed the 6 months treatment regimen.

PAST SURGICAL HISTORY Patient underwent ORIF (unrecalled
year) on her left wrist.

PERSONAL/SOCIAL HISTORY Patient is not a known smoker. An
occasional alcoholic beverage drinker. No history of elicit drug use.

FAMILY HISTORY Patient has a family history of
Hypertension and Diabetes Milletus.

PHYSICAL EXAMINATION GENERAL SURVEY:Patient is awake, alert, ambulatory, cooperative, oriented to time, place and person, no signs of respiratory distress. VITAL SIGNS:BP - 100/60 mmHg (R) ARM LYINGPR - 72 BPM (R) RADIAL PULSE; REGULAR, BRISKRR - 20 CPM; TEMP. - 36.9°C (L) AXILLA

PHYSICAL EXAMINATION SKIN:
Brown, dry; no cyanosis, no pallor, no jaundice; warm to touch, good
mobility, good turgor NAILS:
Normal; no clubbing, no cyanosis; crt < 2 seconds

PHYSICAL EXAMINATION HEENT:Head is normocephalic; no deformities, no lesions. No hair loss, face is symmetrical, no involuntary movements. EYES: have good visual acuity, positive direct and consensual light reflexes in both eyes, full extraocular movement. EARS: symmetrical with no deformities, lesions or tenderness; NOSE: midline and symmetrical, no deformities, lesions, septal deviation and discharges, sinuses are clear and non-tender. MOUTH: patient has no inflammation in the mouth and ulceration with pink buccal mucosa, there are missing teeth (molars), and tongue is midline with no fasciculations or deviations.

PHYSICAL EXAMINATION NECK:Symmetrical with no masses, venous distention, tracheal deviation, lymphadenopathies, and thryroid enlargement.
CHEST AND LUNGS:Equal chest expansion; no costal retractions and deformities; normal, quiet breathing, equal tactile fremitus on both sides; no wheezing and crackles.

PHYSICAL EXAMINATION CVS:JVP is at 3cm from the sternal angle with the head of the bed elevated at 30 degrees
ABDOMEN:Has no lesions, striae, edema or tenderness; normoactive bowel sounds, liver is not enlarged with a span of 7cm midclavicular line and 5cm from midsternal line.

PHYSICAL EXAMINATION EXTREMITIES:No redness, no cyanosis, no edema or pallor.
BACK: (-)Pain upon palpation, No
deformities, no lesions, no edema.

PHYSICAL EXAMINATION NEUROLOGIC:Patient is awake, alert, coherent, cooperative, oriented to time, place and person, good insight and judgment

PHYSICAL EXAMINATIONCRANIAL NERVES:1 - intact sense of smell2 - able to read nameplate at a distance of 1 foot, normal fundoscopic findings3,4,6 - ( + ) direct & consensual light reflexes, intact eom, ( + ) accommodation5 - able to clench teeth, ( + ) corneal reflexes, intact facial sense7 - face is symmetrical, normal range of facial expressions8 - intact auditory faculties, can hear whispered voiced at a distance of 1 FOOT9, 10 - ( + ) gag reflex; ( - ) hoarseness; uvula is midline, symmetrical rise of soft palate11 - able to shrug shoulders and turn neck in both directions against resistance12 - tongue is midline; ( - ) atrophy, ( - ) fasciculations

PHYSICAL EXAMINATION MOTOR: ( - ) involuntary movements, Needs assistance in standing but claims to have been improving MUSCLE TONE:Adequate muscular tone; ( - ) rigidity, ( - ) spasticity MUSCLE STRENGTH:5/5 in the upper and 4/5 in the lower extremities REFLEXES:+2 SENSORY:Able to feel pain, temperature, light touch, heavy touch, vibration and position